The Health of a Community Depends on Fair Health Insurance Practices Antonio Rios
The Health of a Community Depends on Fair Health Insurance Practices Antonio Rios – it’s a statement that resonates deeply, isn’t it? We often hear about healthcare access and affordability, but how much do we truly understand the interconnectedness between fair insurance practices and the overall well-being of our communities? This post dives into that crucial relationship, exploring the principles of fairness, the challenges faced by vulnerable populations, and the vital role of government regulation in creating a healthier society for everyone.
We’ll examine different health insurance models, analyze the impact of unaffordable premiums on community health outcomes, and look at successful examples of communities that have prioritized fair insurance practices. Get ready to explore the vital link between equitable access to healthcare and a thriving community!
Defining Fair Health Insurance Practices
Source: slideplayer.com
Fair health insurance practices are crucial for ensuring a healthy community. They represent a system designed to provide equitable access to quality healthcare, mitigating financial burdens and promoting overall well-being for all members of society. This goes beyond simply providing coverage; it encompasses a comprehensive approach that addresses accessibility, affordability, and the quality of care received.Fair health insurance practices, in the context of community health, prioritize equitable access to necessary medical services regardless of socioeconomic status, geographic location, or pre-existing conditions.
This means everyone within a community has a reasonable opportunity to obtain the healthcare they need, without facing insurmountable financial obstacles or discriminatory practices. The principles underpinning fairness involve a balance between individual responsibility and societal support, aiming to minimize health disparities and improve population health outcomes.
Accessibility of Healthcare Services
Accessibility focuses on removing barriers that prevent individuals from accessing necessary healthcare. This includes geographical barriers (lack of providers in rural areas), financial barriers (high premiums, deductibles, and co-pays), and systemic barriers (complex application processes, language barriers, discrimination). Addressing these barriers might involve expanding provider networks, implementing subsidies or financial assistance programs, simplifying enrollment procedures, and offering multilingual services.
For example, the expansion of telehealth services has significantly improved access for individuals in remote areas or those with mobility limitations. The implementation of community health clinics in underserved neighborhoods also directly addresses accessibility challenges.
Affordability of Healthcare
Affordability centers on making healthcare financially manageable for individuals and families. This requires controlling healthcare costs while ensuring that essential services remain accessible. Strategies to improve affordability include negotiating lower prices with pharmaceutical companies, promoting preventive care to reduce the need for expensive treatments, and implementing cost-sharing mechanisms that are proportionate to income. For instance, countries with universal healthcare systems often utilize progressive taxation to fund healthcare, ensuring that those with higher incomes contribute a larger share.
In contrast, systems with high out-of-pocket costs can lead to delayed or forgone care, particularly among low-income populations.
Quality of Healthcare Services
Quality of care encompasses the effectiveness, safety, and patient-centeredness of medical services. This involves ensuring that healthcare providers adhere to best practices, utilizing evidence-based treatments, and prioritizing patient satisfaction and shared decision-making. Measuring quality involves tracking key metrics such as patient outcomes, readmission rates, and patient experience surveys. Examples of initiatives to improve quality include implementing electronic health records to improve coordination of care, promoting continuing medical education for healthcare providers, and establishing patient advocacy programs.
A high-quality system fosters trust and ensures that individuals receive the best possible care.
Comparison of Health Insurance Models
Different models of health insurance systems significantly impact community health. A single-payer system, like in Canada, provides universal coverage but may face challenges in managing costs and ensuring timely access to specialized care. A multi-payer system, such as in the United States, offers more choice but can lead to significant disparities in access and affordability depending on an individual’s employment and insurance coverage.
Social health insurance systems, common in many European countries, combine elements of both, aiming to balance universality with market-based mechanisms. The effectiveness of each model depends on various factors, including the specific design, regulatory environment, and the country’s overall healthcare infrastructure. Each model presents unique advantages and disadvantages regarding accessibility, affordability, and quality, ultimately impacting the overall health of the community.
Access to Healthcare and Insurance Coverage
Fair health insurance practices are fundamentally linked to a community’s access to healthcare. Without equitable insurance coverage, many individuals and families face significant barriers to receiving necessary medical care, leading to poorer health outcomes and exacerbating existing health disparities. The availability and affordability of healthcare services are directly influenced by the design and implementation of health insurance systems.Access to healthcare hinges on having both health insurance coverage and the ability to utilize that coverage effectively.
Fair insurance practices ensure that coverage is comprehensive, affordable, and accessible to all members of the community, regardless of socioeconomic status, geographic location, or pre-existing conditions. Conversely, unfair practices, such as discriminatory pricing, restrictive coverage limitations, or inadequate provider networks, severely restrict access to care for vulnerable populations.
Barriers to Healthcare Access for Vulnerable Populations
Several barriers prevent vulnerable populations from accessing healthcare, with insurance coverage playing a crucial role. These barriers often intersect and compound each other, creating significant challenges for individuals and families. For instance, high deductibles and co-pays associated with even seemingly comprehensive insurance plans can be prohibitive for low-income individuals, effectively rendering the insurance useless for anything but catastrophic events.
Similarly, limited provider networks within insurance plans can restrict access to specialists or facilities, particularly in rural or underserved areas, forcing patients to travel long distances or forgo necessary care altogether. Language barriers, cultural differences, and a lack of health literacy can further complicate access, even when insurance is available. Finally, undocumented immigrants often face significant obstacles to accessing healthcare, even for emergency situations, due to fear of deportation and lack of affordable insurance options.
A Hypothetical Healthcare Access Program
To address these barriers, a comprehensive healthcare access program incorporating fair insurance practices is needed. This program would focus on several key elements. First, it would mandate universal healthcare coverage, ensuring that all community members have access to a basic level of healthcare regardless of their employment status or income. This coverage would include comprehensive benefits, with minimal out-of-pocket costs for essential services.
Second, the program would establish a robust network of healthcare providers across all geographic areas, including rural and underserved communities. This network would include primary care physicians, specialists, and mental health professionals, ensuring accessibility for all residents. Third, the program would actively address language and cultural barriers through multilingual services, culturally sensitive healthcare providers, and health education materials in multiple languages.
Finally, the program would promote health literacy through community outreach programs and educational initiatives, empowering individuals to make informed decisions about their healthcare. Crucially, the program would strictly enforce fair insurance practices, preventing discriminatory pricing, restrictive coverage limitations, and inadequate provider networks. This would ensure that all members of the community receive equitable access to the healthcare services they need.
The program could be partially funded through progressive taxation, ensuring that those with greater means contribute more towards the collective good. This system would resemble successful models in other countries, such as the National Health Service in the United Kingdom, adapted to the specific needs and context of the community in question.
Affordability of Healthcare and Insurance Premiums
The affordability of healthcare and insurance premiums is a critical determinant of a community’s overall health. When healthcare is too expensive, individuals delay or forgo necessary care, leading to preventable illnesses and worsening chronic conditions. This, in turn, impacts productivity, increases emergency room visits (which are often more costly), and ultimately strains the community’s resources. The high cost of insurance also pushes many families into financial hardship, forcing them to choose between necessities like food and shelter and essential medical care.High healthcare costs and unaffordable insurance premiums significantly impact community health outcomes.
Delayed or forgone preventative care leads to the progression of manageable conditions into serious, costly health problems. This is particularly true for chronic diseases like diabetes and hypertension, where early intervention can dramatically improve outcomes. Furthermore, the financial burden of medical debt can cause stress, impacting mental health and overall well-being. The inability to access necessary medications or treatments can lead to disability, lost productivity, and even premature death.
Strategies for Improving Affordability
Several strategies can make healthcare and insurance more affordable for low-income families and individuals. Expanding access to affordable health insurance through government subsidies and programs like Medicaid and the Affordable Care Act (ACA) is crucial. Negotiating lower drug prices and implementing cost-containment measures within the healthcare system itself can also significantly reduce expenses. Furthermore, investing in preventative care and public health initiatives can reduce the overall burden of disease and associated costs.
Finally, promoting transparency in healthcare pricing and providing individuals with tools to compare costs and benefits of different plans empowers them to make informed decisions.
Comparison of Health Insurance Plans in [Community Name – e.g., Springfield, Illinois]
The following table provides a hypothetical comparison of four different health insurance plans available in Springfield, Illinois. Note that these are illustrative examples and actual plans and costs will vary depending on the provider, coverage level, and individual circumstances. It’s crucial to check with insurers directly for up-to-date information.
| Plan Name | Monthly Premium | Deductible | Co-pay (Doctor Visit) | Out-of-Pocket Maximum |
|---|---|---|---|---|
| Bronze Plan A | $200 | $6,000 | $50 | $7,000 |
| Silver Plan B | $350 | $3,000 | $40 | $5,000 |
| Gold Plan C | $500 | $1,500 | $30 | $4,000 |
| Platinum Plan D | $700 | $500 | $20 | $3,000 |
Quality of Healthcare and Insurance Services
Source: slideplayer.com
Fair health insurance practices are inextricably linked to the quality of healthcare received by a community. Without access to quality care, even the most comprehensive insurance plan is rendered ineffective. The quality of healthcare services directly impacts individual and community health outcomes, underscoring the critical importance of this aspect in achieving true health equity.The effectiveness of fair health insurance practices hinges on ensuring access to quality healthcare providers and facilities.
Insurance acts as a crucial bridge, connecting individuals with the care they need. Without adequate insurance coverage, many individuals, particularly those from lower socioeconomic backgrounds, face significant barriers to accessing timely and appropriate care from qualified professionals, leading to poorer health outcomes and increased healthcare disparities. Effective insurance policies should incentivize providers to maintain high standards of care, knowing that their services are more readily accessible to a wider population.
The Interplay Between Insurance and Quality Healthcare Access
Insurance plays a multifaceted role in ensuring access to quality healthcare. Firstly, it facilitates access to a wider network of providers. Individuals with insurance can choose from a broader range of specialists and facilities, often including those with higher quality ratings and advanced technologies. Secondly, insurance mitigates financial barriers. The cost of healthcare, including consultations, treatments, and hospital stays, can be prohibitive.
Insurance significantly reduces out-of-pocket expenses, allowing individuals to prioritize their health without facing crippling financial burdens. This increased affordability enables individuals to seek preventative care and early intervention, ultimately improving health outcomes and reducing the need for more expensive treatments later. Finally, insurance can encourage preventative care. By covering routine check-ups and screenings, insurance plans incentivize individuals to proactively manage their health, leading to earlier detection of diseases and better overall health.
The absence of this crucial safety net significantly limits access to quality care.
Indicators of Quality Healthcare Services
Measuring the quality of healthcare services within a community requires a multifaceted approach, considering various perspectives. A robust assessment needs to incorporate both the structural aspects of healthcare delivery (facilities, equipment, provider qualifications) and the process of care (patient satisfaction, clinical outcomes, adherence to best practices). The role of health insurance is woven throughout these measurements. For example, the percentage of the population with insurance coverage directly influences access to preventive care, resulting in early detection and treatment of diseases.
This, in turn, improves the overall health of the community.
- Provider qualifications and experience: The number of board-certified specialists, average years of experience, and continuing medical education participation rates are crucial indicators. Insurance plans often influence this by preferentially including highly qualified providers in their networks.
- Facility accreditation and infrastructure: Accreditation by reputable organizations (e.g., The Joint Commission) and the availability of advanced medical technology and equipment are essential indicators. Insurance companies often negotiate contracts with facilities based on their quality ratings and infrastructure.
- Patient satisfaction scores: Surveys measuring patient experiences, including wait times, communication with providers, and overall care quality, are valuable indicators. Insurance plans can use these scores to evaluate and select providers who consistently demonstrate high patient satisfaction.
- Clinical outcomes and readmission rates: Measures like mortality rates, infection rates, and hospital readmission rates after specific procedures reflect the quality of care provided. Insurance companies can utilize this data to assess the effectiveness of different providers and facilities and to design programs that improve these metrics.
- Preventive care utilization rates: The percentage of the insured population receiving recommended preventive screenings and vaccinations is a key indicator of a system’s effectiveness in promoting proactive healthcare. Insurance coverage significantly influences these rates.
The Role of Government Regulation in Ensuring Fair Practices: The Health Of A Community Depends On Fair Health Insurance Practices Antonio Rios
Source: slideplayer.com
Government regulation plays a crucial role in establishing and maintaining a fair and equitable health insurance system. Without robust oversight, the market can easily become skewed, leaving vulnerable populations underserved and undermining the overall health of the community. Effective regulation ensures that insurance companies act responsibly, providing accessible, affordable, and quality healthcare coverage to all citizens.Government regulation fosters fair health insurance practices by setting minimum standards for coverage, preventing discriminatory practices, and ensuring transparency and accountability within the industry.
This involves establishing clear guidelines on what services must be covered, preventing insurers from denying coverage based on pre-existing conditions or other discriminatory factors, and mandating the public disclosure of pricing and coverage details. This proactive approach helps protect consumers and promotes a healthier, more equitable society.
Government Mechanisms for Regulation
Several key mechanisms are employed by governments to regulate health insurance. These include the establishment of independent regulatory bodies responsible for overseeing the industry, the implementation of standardized insurance contracts, and the enforcement of consumer protection laws. For example, many countries have agencies that monitor insurer compliance with regulations, investigate consumer complaints, and impose penalties for violations. Standardized contracts help ensure that consumers understand their coverage, while consumer protection laws safeguard individuals from unfair or deceptive practices by insurance companies.
The effectiveness of these mechanisms varies considerably depending on the level of government resources dedicated to enforcement and the specific regulatory framework in place.
Consequences of Insufficient Regulation
Insufficient or ineffective government regulation can have severe consequences for community health. Without adequate oversight, insurance companies may prioritize profit maximization over patient care, leading to practices such as denying necessary treatments, imposing excessive premiums, or limiting access to essential healthcare services. This can disproportionately affect low-income individuals and marginalized communities, widening existing health disparities and exacerbating existing inequalities.
The result is a less healthy population, increased healthcare costs due to delayed or forgone care, and a decline in overall societal well-being. For instance, a lack of regulation concerning pre-existing conditions can lead to individuals being denied coverage for critical illnesses, forcing them to bear significant medical expenses, leading to financial hardship and potentially impacting their overall health.
Comparative Regulatory Approaches
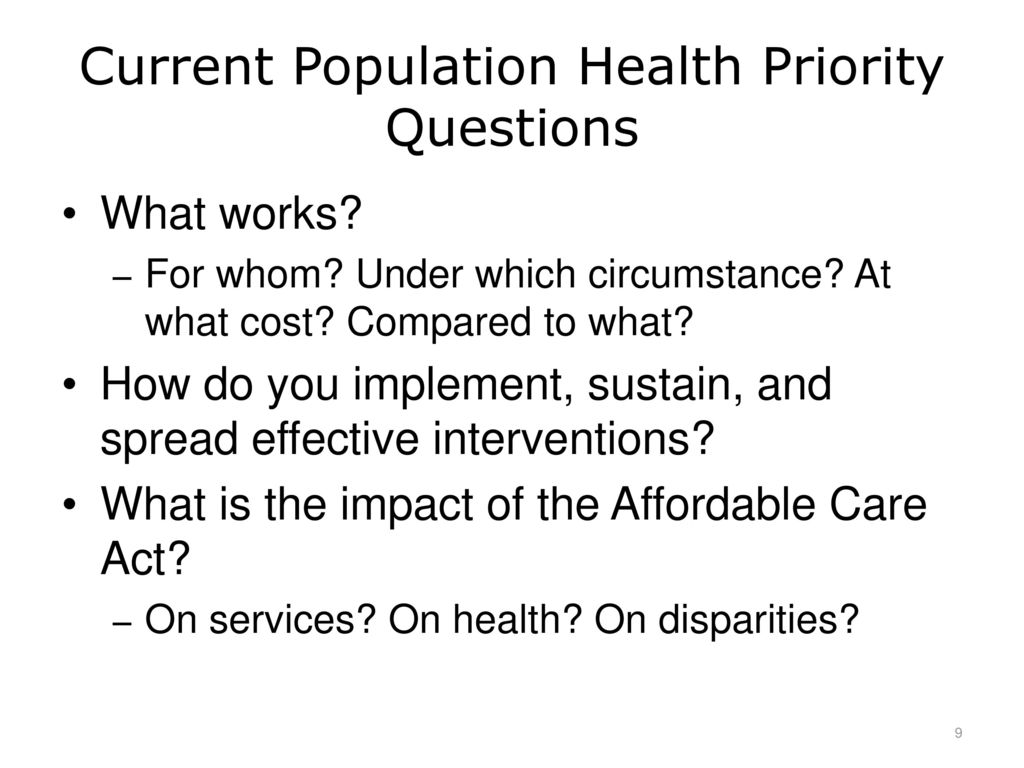
Different countries employ varying regulatory approaches to health insurance. Some countries, like Canada, utilize a single-payer system where the government directly funds healthcare, leading to universal coverage and greater equity. This model offers strong regulation and control over healthcare costs and access. In contrast, the United States operates a largely private insurance market with a significant degree of government regulation through legislation like the Affordable Care Act (ACA).
The ACA aimed to expand coverage and regulate insurance practices, but it still leaves millions uninsured or underinsured. The European Union demonstrates a diverse approach, with member states employing various models ranging from universal single-payer systems to more market-based models with varying degrees of government intervention. These diverse approaches highlight the complex interplay between government intervention, market forces, and the pursuit of fair and equitable health insurance practices.
Antonio Rios is right: a healthy community needs fair health insurance. Access to quality care is key, and that hinges on efficient record-keeping. Improving this efficiency is exactly what the new integration of Nuance’s generative AI scribe with Epic EHRs, as detailed in this article nuance integrates generative ai scribe epic ehrs , aims to do. Streamlining documentation frees up healthcare professionals, ultimately benefiting patients and reinforcing Rios’s point about equitable access to healthcare.
The effectiveness of each approach is subject to ongoing debate and evaluation.
Community Health Outcomes and Fair Insurance
Fair health insurance practices are not merely a matter of economic policy; they are fundamentally intertwined with the health and well-being of entire communities. Access to affordable and quality healthcare, facilitated by equitable insurance systems, directly impacts a community’s overall health outcomes, leading to measurable improvements in various health metrics. This connection is crucial for understanding how societal investment in fair insurance translates into a healthier population.Improved access to healthcare, a direct consequence of fair insurance practices, demonstrably improves community health outcomes.
When individuals can readily access preventative care, early diagnosis, and timely treatment, the incidence of preventable diseases and chronic conditions decreases. This reduces the burden on healthcare systems, improves quality of life, and extends lifespans. Furthermore, access to mental healthcare, often overlooked, is equally crucial, and fair insurance ensures that these vital services are within reach for all community members.
Improved Access and Reduced Health Disparities
Fair insurance practices, such as community rating (where premiums are based on the community’s overall risk rather than individual risk factors) and guaranteed issue (where insurers cannot deny coverage based on pre-existing conditions), actively reduce health disparities. These practices ensure that vulnerable populations, often marginalized due to socioeconomic status or health conditions, receive the same access to care as the rest of the community.
The result is a healthier, more equitable society where health outcomes are less determined by socioeconomic factors. For example, studies have shown that the expansion of Medicaid, a form of government-sponsored health insurance, in certain states led to significant reductions in uninsured rates and improvements in access to care, particularly for low-income populations. This improved access, in turn, led to better health outcomes and reduced mortality rates among those populations.
Examples of Successful Implementations and Improved Health Metrics, The health of a community depends on fair health insurance practices antonio rios
Massachusetts’s landmark health care reform in 2006 provides a compelling case study. By implementing a system with an individual mandate (requiring individuals to obtain health insurance), community rating, and subsidized coverage for low-income individuals, Massachusetts significantly reduced its uninsured rate. Subsequent studies indicated improvements in several key health metrics, including decreased hospitalizations and mortality rates. Similarly, countries with universal healthcare systems, such as Canada and the United Kingdom, have consistently demonstrated better population health outcomes compared to countries with predominantly market-based healthcare systems, reflecting the positive impact of widespread access to care facilitated by fair insurance practices.
Visual Representation of the Correlation
Imagine a graph with two axes. The horizontal axis represents the level of fairness in health insurance practices, ranging from “unfair” (high disparities in access, high costs, limited coverage) to “fair” (equitable access, affordable premiums, comprehensive coverage). The vertical axis represents key community health outcomes, such as life expectancy, infant mortality rate, and prevalence of chronic diseases. The graph would show a clear positive correlation: as the level of fairness in insurance practices increases (moving along the horizontal axis towards “fair”), the community health outcomes improve (moving upwards along the vertical axis), demonstrating a significant reduction in infant mortality rates, increased life expectancy, and a lower prevalence of preventable diseases.
Antonio Rios is right; a healthy community hinges on equitable healthcare access, and that starts with fair insurance practices. The recent news about NextGen exploring a sale, as reported by Reuters nextgen exploring sale reuters , highlights how even large corporations grapple with financial pressures that ultimately impact the affordability and accessibility of healthcare. This underscores the critical need for strong regulations and transparent insurance policies to protect vulnerable populations.
The line representing this correlation would be an upward-sloping curve, indicating that the improvements in health outcomes accelerate with greater fairness in insurance practices. This visual representation clearly demonstrates that a more equitable healthcare system, underpinned by fair insurance practices, results in a healthier community.
Antonio Rios is right: a healthy community needs fair health insurance. Access to quality care is fundamental, and the recent struggles highlighted by the new york nurse strike deal reached at Mount Sinai and Montefiore underscore this. These nurses fought for better patient care, indirectly impacting the health of their community by ensuring fair working conditions and adequate staffing levels – all linked to affordable and accessible healthcare for everyone.
The Impact of Health Insurance on Vulnerable Populations
Fair health insurance practices are crucial for the well-being of any community, but their impact is especially profound on vulnerable populations. These groups, often facing systemic disadvantages, are disproportionately affected by unfair or inadequate insurance coverage, leading to poorer health outcomes and exacerbating existing inequalities. Understanding this disparity is essential for designing effective policies that promote health equity.Unfair health insurance practices significantly hinder access to necessary healthcare for vulnerable populations.
This includes the elderly, who often face higher healthcare costs and may have limited incomes; low-income individuals, who may struggle to afford even basic insurance premiums or out-of-pocket expenses; and minority groups, who frequently experience discrimination in healthcare access and quality. These populations often face higher rates of chronic illnesses and require more frequent medical care, yet their limited access to affordable and comprehensive insurance leaves them at a significant disadvantage.
The lack of preventative care and delayed treatment due to financial constraints can lead to more severe health problems and higher overall healthcare costs in the long run.
Disproportionate Impact of Unfair Practices on Vulnerable Groups
The consequences of unfair health insurance practices are particularly devastating for vulnerable populations. For example, the elderly, facing age-related health issues, may be denied coverage for necessary treatments or medications due to pre-existing conditions clauses. Low-income individuals may be forced to choose between essential needs and healthcare, leading to delayed or forgone care, potentially resulting in preventable hospitalizations or worsening health conditions.
Minorities, already facing systemic health disparities, may encounter discrimination in insurance coverage, leading to inadequate access to quality care and poorer health outcomes. This disparity is often amplified by factors such as language barriers, cultural differences, and a lack of trust in the healthcare system.
Policies and Programs for Protecting Vulnerable Populations
Several policies and programs can enhance the protection and support of vulnerable populations through fairer insurance practices. Expanding access to affordable healthcare coverage through initiatives like the Affordable Care Act (ACA) in the United States is a crucial step. Strengthening regulations to prevent discriminatory practices by insurance companies and ensuring transparency in pricing and coverage are also essential.
Implementing programs that provide financial assistance for healthcare costs, such as subsidies and tax credits, can significantly improve access to care for low-income individuals and families. Furthermore, investing in community-based health centers and culturally competent healthcare providers can improve access to quality care for minority groups and address language barriers.
Case Study: Impact of the ACA on Low-Income Individuals
The Affordable Care Act (ACA) in the United States serves as a relevant case study. Before the ACA, millions of low-income Americans lacked health insurance, resulting in delayed or forgone care and poorer health outcomes. The ACA significantly expanded access to health insurance through subsidized marketplace plans and Medicaid expansion, leading to a substantial reduction in the uninsured rate.
While the ACA has faced challenges and limitations, studies have shown that it has had a positive impact on the health and well-being of low-income individuals, particularly by improving access to preventative care and reducing financial burdens associated with healthcare. However, ongoing challenges remain, such as affordability of premiums and deductibles, and access to care in rural and underserved areas.
These ongoing challenges highlight the need for continued efforts to ensure that healthcare is truly accessible and affordable for all, particularly vulnerable populations.
Ultimate Conclusion
Ultimately, Antonio Rios’s assertion rings true: a healthy community is built on a foundation of fair health insurance practices. By addressing affordability, accessibility, and quality of care, we can create a system that supports everyone, regardless of their socioeconomic status or background. It’s not just about numbers and statistics; it’s about building a society where everyone has the opportunity to live a long, healthy, and fulfilling life.
Let’s continue the conversation and work towards a future where healthcare is a right, not a privilege.
Essential FAQs
What are some examples of unfair health insurance practices?
Examples include discriminatory practices based on pre-existing conditions, excessively high premiums that make coverage unaffordable, and limited access to necessary specialists or treatments.
How does fair insurance impact life expectancy?
Studies show a strong correlation between access to quality healthcare (facilitated by fair insurance) and increased life expectancy, particularly among vulnerable populations.
What role do non-profit organizations play in ensuring fair health insurance practices?
Non-profits advocate for policy changes, provide resources to underserved communities, and offer support services to navigate the complexities of the healthcare system.