5 Healthcare Consumer Trends to Prepare For
5 Healthcare Consumer Trends to Prepare For: The healthcare landscape is changing rapidly, driven by technological advancements, shifting consumer expectations, and a growing focus on preventative care. Understanding these trends is crucial for navigating the complexities of modern healthcare and making informed decisions about your health and well-being. This post explores five key trends that will significantly impact how we access and experience healthcare in the years to come.
From the rise of telehealth and the increasing use of wearable technology to the growing importance of personalized medicine and consumer empowerment, we’ll delve into the implications of each trend and offer practical advice on how to best prepare yourself. Get ready to navigate the future of healthcare with confidence!
The Rise of Telehealth: 5 Healthcare Consumer Trends To Prepare For
Telehealth, the remote delivery of healthcare services using technology, has experienced explosive growth, transforming how patients access care and impacting healthcare costs significantly. This shift is driven by factors like increased access to high-speed internet, advancements in medical technology, and a growing preference for convenient healthcare options. The implications for both patients and the healthcare system are profound and far-reaching.Telehealth’s Impact on Patient Access and Healthcare CostsTelehealth significantly improves access to care, particularly for individuals in rural areas or those with limited mobility.
The elimination of geographical barriers allows patients to consult specialists who might otherwise be inaccessible. Furthermore, telehealth can reduce healthcare costs by decreasing the need for expensive in-person visits, reducing travel expenses, and potentially leading to earlier diagnosis and treatment, preventing more costly interventions later. Studies have shown that telehealth can be cost-effective for managing chronic conditions like diabetes and hypertension, leading to lower hospitalization rates and improved patient outcomes.
Successful Telehealth Implementations and Outcomes
Several successful telehealth implementations demonstrate its effectiveness. For example, the Mayo Clinic’s telehealth program has shown improved patient satisfaction and reduced hospital readmissions for patients with chronic heart failure. Similarly, the use of telehealth for stroke care has led to faster diagnosis and treatment, improving patient outcomes. In rural communities, telehealth has enabled access to specialist consultations, improving the overall health and well-being of residents.
These successful implementations highlight telehealth’s potential to improve healthcare access and quality while managing costs effectively.
Advantages and Disadvantages of Telehealth Versus In-Person Care, 5 healthcare consumer trends to prepare for
Telehealth offers several advantages, including convenience, reduced travel time and costs, increased access to specialists, and potentially improved patient engagement through remote monitoring. However, it also presents disadvantages, such as the lack of physical examination, potential technological barriers for some patients, and concerns about data privacy and security. In-person care, while often more expensive and less convenient, allows for a thorough physical examination and facilitates a stronger doctor-patient relationship built on direct interaction.
The ideal approach often involves a blended model, integrating telehealth with in-person visits to leverage the strengths of both.
Technological Infrastructure for Effective Telehealth
Effective telehealth relies on robust technological infrastructure. This includes reliable high-speed internet access for both patients and healthcare providers, secure video conferencing platforms compliant with HIPAA regulations, electronic health record (EHR) systems integrated with telehealth platforms, and appropriate medical devices for remote monitoring (e.g., blood pressure monitors, wearable sensors). The quality of the technology directly impacts the quality of care delivered, highlighting the importance of investing in and maintaining a reliable infrastructure.
Furthermore, training for both providers and patients is crucial to ensure effective use of the technology.
A Hypothetical Telehealth Program for the Elderly
A telehealth program designed for the elderly could focus on remote monitoring of chronic conditions such as hypertension, diabetes, and heart failure. The program would involve regular virtual check-ins with a healthcare provider, remote monitoring of vital signs using wearable devices, and medication adherence support through automated reminders and virtual counseling. The program would also incorporate educational resources on healthy aging and fall prevention.
This program would leverage technology to enhance the quality of life for elderly individuals, enabling them to age in place with increased independence and access to timely healthcare. The program would require user-friendly interfaces and robust technical support to ensure accessibility and ease of use for the elderly population.
Personalized Medicine and Data-Driven Care
The healthcare landscape is rapidly shifting towards a more personalized and data-driven approach. This means moving away from a “one-size-fits-all” model to treatments tailored to an individual’s unique genetic makeup, lifestyle, and environment. This trend is fueled by advancements in genomics, data analytics, and artificial intelligence, promising more effective and efficient healthcare.
Genetic Information’s Impact on Healthcare Decisions
Genetic information is revolutionizing healthcare by allowing for proactive identification of disease risks and the tailoring of treatments based on an individual’s genetic predisposition. For example, genetic testing can reveal a predisposition to certain cancers, heart conditions, or neurological disorders, enabling early interventions and preventative measures. This allows for more targeted screening, earlier diagnosis, and personalized treatment plans, significantly improving patient outcomes.
Pharmacogenomics, a branch of personalized medicine, analyzes how an individual’s genes affect their response to drugs. This helps doctors choose the most effective medication and dosage, minimizing adverse reactions and maximizing therapeutic benefits. For instance, certain genetic variations can predict whether a patient will respond well to a particular chemotherapy drug, allowing for a more informed treatment choice.
Examples of Personalized Medicine Applications and Their Efficacy
Personalized medicine is already impacting various areas of healthcare. In oncology, genomic sequencing helps identify specific mutations driving a patient’s cancer, leading to the selection of targeted therapies. This approach has shown improved survival rates in several cancer types compared to traditional chemotherapy. In cardiology, genetic testing can identify individuals at high risk for heart disease, allowing for lifestyle modifications and preventative medication to reduce their risk.
Similarly, in pharmacogenomics, genetic testing guides medication selection for conditions like depression and anxiety, improving treatment efficacy and reducing side effects. For example, certain antidepressants are more effective in individuals with specific genetic variations, while others may experience increased side effects. The efficacy of these personalized approaches is demonstrated through numerous clinical trials and real-world applications showing improved patient outcomes and reduced healthcare costs in the long run.
Ethical Considerations Surrounding the Use of Patient Data in Healthcare
The increasing use of patient data in personalized medicine raises significant ethical concerns. Protecting patient privacy and ensuring data security are paramount. Strict regulations and ethical guidelines are crucial to prevent unauthorized access, misuse, or discrimination based on genetic information. Informed consent is essential, ensuring patients understand how their data will be used and have control over its access and sharing.
Addressing potential biases in algorithms used for data analysis is also crucial to avoid perpetuating health disparities. Transparency in data usage and the development of robust data governance frameworks are vital to build trust and ensure ethical implementation of personalized medicine.
The Role of Artificial Intelligence in Improving Personalized Medicine
Artificial intelligence (AI) plays a crucial role in advancing personalized medicine. AI algorithms can analyze vast amounts of patient data, including genomic information, medical history, lifestyle factors, and environmental exposures, to identify patterns and predict individual risks and responses to treatments. AI-powered diagnostic tools can improve the accuracy and speed of diagnosis, while AI-driven drug discovery can accelerate the development of new personalized therapies.
Machine learning models can predict patient outcomes based on individual characteristics, helping clinicians make more informed decisions about treatment strategies. For example, AI can analyze medical images to detect early signs of cancer, enabling earlier intervention and improving survival rates.
Comparison of Different Personalized Medicine Approaches
| Approach | Focus | Data Used | Examples |
|---|---|---|---|
| Genomic Medicine | Genetic variations | DNA sequencing | Cancer treatment, pharmacogenomics |
| Pharmacogenomics | Drug response | Gene-drug interactions | Antidepressant selection, chemotherapy optimization |
| Proteomics | Protein expression | Protein analysis | Disease biomarker discovery, drug target identification |
| Lifestyle Medicine | Lifestyle factors | Dietary habits, physical activity, stress levels | Personalized nutrition plans, exercise recommendations |
The Growing Importance of Preventative Care
Preventative care, once a secondary consideration in healthcare, is rapidly gaining prominence. This shift is driven by a confluence of factors, including a growing awareness of the long-term benefits of proactive health management, advancements in screening technologies, and the increasing costs associated with treating chronic diseases. By focusing on prevention, we can significantly improve overall health outcomes and reduce the burden on healthcare systems.The increased emphasis on preventative care stems from several key drivers.
Rising healthcare costs are making proactive measures more financially attractive in the long run. Furthermore, a greater understanding of the links between lifestyle choices and chronic diseases is motivating individuals to take a more active role in their health. Finally, technological advancements, such as sophisticated screening tools and personalized risk assessment models, are making preventative care more accessible and effective.
Factors Driving the Increase in Preventative Care Services
Several interconnected factors are contributing to the rising importance of preventative care. The escalating costs of treating chronic conditions like heart disease, diabetes, and cancer are forcing a reevaluation of healthcare strategies. Investing in prevention is demonstrably more cost-effective than managing these conditions after they develop. Simultaneously, improved understanding of the role of lifestyle factors—diet, exercise, stress management—in disease prevention is empowering individuals to take control of their health.
Finally, technological advancements, such as advanced imaging techniques for early disease detection and personalized genetic testing to identify risk factors, are enhancing the effectiveness of preventative strategies.
Examples of Effective Preventative Care Programs
Effective preventative care programs are multifaceted and tailored to specific populations. For instance, workplace wellness programs often incorporate health screenings, educational workshops on healthy eating and stress management, and on-site fitness facilities. Community-based initiatives may focus on increasing access to affordable health screenings, providing health education to underserved populations, and promoting healthy lifestyles through community events. National campaigns, such as those focused on cancer screening or immunizations, leverage public health infrastructure to reach large populations.
The success of these programs hinges on accessibility, cultural sensitivity, and effective communication strategies.
Challenges in Promoting Preventative Care Among Diverse Populations
Promoting preventative care across diverse populations presents significant challenges. Access to healthcare services remains a major barrier for many, particularly those in low-income communities or rural areas. Cultural beliefs and practices can also influence health-seeking behaviors, making it crucial to tailor preventative care programs to specific cultural contexts. Language barriers, health literacy levels, and mistrust of the healthcare system can further complicate efforts to promote preventative care.
Addressing these challenges requires culturally competent outreach programs, affordable and accessible services, and effective communication strategies that resonate with diverse communities.
Preventative Care Plan for Young Adults (Ages 18-25)
A preventative care plan for young adults should emphasize establishing healthy lifestyle habits and addressing potential risks early on. This plan could include:
- Annual physical exams including blood pressure, cholesterol, and glucose checks.
- Mental health check-ups to address stress, anxiety, and depression.
- Vaccinations against influenza, HPV, and meningococcal disease.
- Education on healthy eating habits, regular physical activity, and safe sex practices.
- Screening for sexually transmitted infections (STIs).
Early detection and intervention are key to preventing serious health problems later in life.
Long-Term Cost Savings Associated with Preventative Care
The long-term cost savings associated with preventative care are substantial. Studies have shown that investing in preventative measures can significantly reduce healthcare expenditures by preventing the development of chronic diseases. For example, regular colorectal cancer screenings can detect precancerous polyps, allowing for early intervention and preventing the need for costly and invasive treatments later on. Similarly, routine blood pressure monitoring and management can prevent heart attacks and strokes, avoiding the significant costs associated with hospitalization and long-term care.
The economic benefits of preventative care extend beyond individual savings, impacting healthcare systems and national economies. The cost-effectiveness of preventative care is well-documented, making it a fiscally responsible and ethically sound healthcare strategy.
Consumer Empowerment and Healthcare Transparency

Source: innovamarketinsights.com
The healthcare landscape is undergoing a significant shift, driven by a growing demand for transparency and consumer empowerment. Patients are no longer passive recipients of care; they’re actively seeking information, comparing prices, and demanding greater control over their health decisions. This trend reflects a broader societal shift towards informed consumerism, where individuals expect clarity and choice in all aspects of their lives, including healthcare.The increasing demand for healthcare price transparency is a key driver of this empowerment.
Consumers are increasingly frustrated by the lack of upfront information about the cost of medical services. Surprise medical bills and opaque billing practices contribute to financial anxieties and create barriers to accessing necessary care. This lack of transparency disproportionately affects vulnerable populations who may struggle to understand complex medical bills and navigate the insurance system. The push for price transparency aims to equip consumers with the knowledge needed to make informed choices about their healthcare spending, promoting both cost-effectiveness and improved patient outcomes.
Healthcare Price Transparency Initiatives
Several initiatives are underway to improve healthcare price transparency. Government regulations, such as those requiring hospitals to publicly disclose their prices, are gaining momentum. Furthermore, many private healthcare providers are developing online tools and resources to allow patients to estimate the cost of procedures and services before receiving care. While the implementation and effectiveness of these initiatives vary, the overall trend is toward greater transparency in healthcare pricing.
For example, some states have implemented laws requiring hospitals to post their standard charges online, allowing consumers to compare prices across different facilities. This has led to increased competition and, in some cases, reduced prices for certain procedures.
Strategies for Improving Healthcare Communication and Patient Engagement
Effective communication is paramount to empowering healthcare consumers. Strategies for improving communication include using plain language in all patient materials, offering multiple communication channels (e.g., phone, email, online portals), and actively involving patients in shared decision-making. Patient portals, which provide secure online access to medical records and communication tools, are becoming increasingly popular. These platforms allow patients to easily access their test results, schedule appointments, and communicate with their healthcare providers, promoting greater engagement and control over their care.
Regular follow-up calls and proactive communication from healthcare providers can also improve patient satisfaction and outcomes. For example, a post-operative check-in call from a surgeon can alleviate anxiety and ensure that patients are adhering to their treatment plan.
The Role of Patient Advocacy Groups in Improving Healthcare Access
Patient advocacy groups play a vital role in improving healthcare access and ensuring that patients’ voices are heard. These groups provide support, education, and resources to patients and their families, often focusing on specific conditions or healthcare issues. They also advocate for policy changes that improve healthcare access and affordability. For instance, advocacy groups have played a crucial role in pushing for legislation related to insurance coverage for pre-existing conditions and affordable prescription drugs.
Their efforts contribute to a more equitable and patient-centered healthcare system.
Navigating the 5 healthcare consumer trends to prepare for can feel overwhelming, especially when considering access to care. One significant factor impacting this is the changing landscape of rural healthcare, as highlighted in this insightful article on Rural Hospitals Labor Delivery & which directly relates to the availability of essential services. Understanding these challenges helps us better prepare for the future of healthcare consumerism and the potential impact on our access to care.
The Impact of Online Health Information on Consumer Decision-Making
The proliferation of online health information has significantly impacted consumer decision-making. Patients now have access to a vast amount of information about diseases, treatments, and healthcare providers. While this access can be empowering, it also presents challenges. Consumers need to be able to critically evaluate the credibility and accuracy of online health information, recognizing that not all sources are reliable.
The rise of medical misinformation necessitates health literacy education and the promotion of reliable sources such as government health agencies and reputable medical organizations. For example, a patient researching a particular condition might encounter conflicting information from various online sources, highlighting the need for discerning evaluation and verification of sources.
Resources for Navigating the Healthcare System
Access to reliable information and support is crucial for navigating the complexities of the healthcare system. Below are some resources that can help consumers make informed decisions and advocate for their needs:
- The Centers for Medicare & Medicaid Services (CMS): Provides information about Medicare and Medicaid programs, as well as resources for navigating the healthcare system.
- The Agency for Healthcare Research and Quality (AHRQ): Offers evidence-based information on a wide range of health topics.
- The National Institutes of Health (NIH): Conducts and supports medical research, providing valuable information about various health conditions and treatments.
- State and local health departments: Offer information and resources specific to your community.
- Patient advocacy groups: Provide support and advocacy for individuals with specific health conditions.
The Influence of Wearable Technology and Health Apps
The rise of wearable technology and health apps is revolutionizing how we monitor, manage, and improve our health. These tools offer unprecedented access to personal health data, empowering individuals to take a more active role in their well-being and providing healthcare providers with valuable insights. This trend is rapidly transforming healthcare delivery, leading to more personalized and preventative approaches to care.
So, you’re trying to get ahead of the curve with those 5 healthcare consumer trends? Smart move! One area impacting this is personalized medicine, and a fascinating development is the potential for widespread use of digital twins. Check out this insightful study on study widespread digital twins healthcare to see how this technology could shape the future.
Understanding this will definitely help you navigate those 5 trends more effectively.
Wearable technology and health apps are becoming increasingly sophisticated, offering a wide array of functionalities beyond simple step counting. The integration of these technologies with traditional healthcare systems promises to improve patient outcomes and streamline healthcare processes. However, it’s crucial to understand the limitations and potential risks associated with this rapidly evolving field.
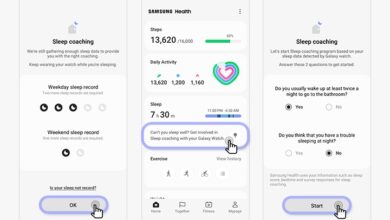
Types of Wearable Health Technology and Their Applications
Wearable health technology encompasses a diverse range of devices designed to monitor various physiological parameters. Smartwatches, for example, can track heart rate, sleep patterns, and activity levels. Fitness trackers often provide similar functionalities, sometimes with added features like GPS tracking for exercise. More specialized devices, such as continuous glucose monitors (CGMs) for diabetics or electrocardiogram (ECG) monitors for heart health, provide detailed data for specific conditions.
These devices empower individuals to actively monitor their health, potentially identifying issues early and improving adherence to treatment plans. For instance, a CGM can provide real-time glucose readings, enabling diabetics to adjust their insulin dosages more effectively.
Examples of Health Apps Changing Healthcare Delivery
Health apps are transforming healthcare delivery in several ways. Many apps offer remote patient monitoring capabilities, allowing healthcare providers to track patients’ vital signs and other health data remotely. This is particularly useful for managing chronic conditions, reducing hospital readmissions, and improving patient engagement. Other apps provide medication reminders, appointment scheduling, and telehealth consultations, streamlining the healthcare experience.
Mental health apps are also becoming increasingly popular, offering tools for managing stress, anxiety, and depression. For example, apps like Calm and Headspace provide guided meditation and mindfulness exercises, while others offer cognitive behavioral therapy (CBT) techniques.
Accuracy and Reliability of Wearable Health Trackers
The accuracy and reliability of wearable health trackers vary significantly depending on the device and the specific metric being measured. While many trackers provide reasonably accurate measurements of steps taken and calories burned, the accuracy of heart rate monitoring and sleep tracking can be less consistent. Factors such as skin tone, body hair, and the fit of the device can all affect accuracy.
It’s important to remember that these devices are generally not intended to replace medical-grade diagnostic tools. Data from wearable trackers should be considered supplementary information and not a definitive diagnosis. For instance, a smartwatch might detect an irregular heartbeat, prompting a user to seek medical attention, but it cannot provide a definitive diagnosis of a heart condition.
Potential Privacy Concerns Associated with Wearable Technology
The collection and storage of personal health data by wearable devices and health apps raise significant privacy concerns. The potential for data breaches and unauthorized access to sensitive information is a real risk. Moreover, the use of this data for marketing or other commercial purposes without informed consent is a major ethical concern. Regulations and guidelines are constantly evolving to address these issues, but users need to be aware of the potential risks and take steps to protect their privacy.
This includes carefully reviewing the privacy policies of apps and devices before use, and being mindful of the permissions granted to these applications.
Hypothetical Scenario Illustrating Positive Impact of a Health App
Imagine Sarah, a 45-year-old woman with a history of high blood pressure. She begins using a health app that tracks her blood pressure, activity levels, and sleep patterns. The app provides personalized recommendations for lifestyle changes, including regular exercise and a healthier diet. It also sends reminders to take her medication and provides educational materials about managing her condition.
Over time, Sarah’s blood pressure improves significantly, and she experiences a reduction in her symptoms. The app’s data provides valuable insights for her doctor, allowing them to monitor her progress and adjust her treatment plan as needed. This hypothetical scenario demonstrates how a health app, coupled with appropriate medical supervision, can lead to improved health outcomes.
So, you’re thinking about those 5 healthcare consumer trends to prepare for? One thing impacting the future of healthcare is the rapid integration of AI, like what we’re seeing with nuance integrates generative ai scribe epic ehrs , which will likely change how patient information is handled. This tech is just one example of the shifts shaping how we access and experience healthcare, meaning staying informed about these 5 trends is more important than ever.
Outcome Summary

Source: buxtonco.com
The future of healthcare is undeniably consumer-centric, driven by technology and a demand for greater transparency and personalization. By understanding the five trends discussed – telehealth, personalized medicine, preventative care, consumer empowerment, and the influence of wearable technology – you can proactively manage your health and navigate the evolving healthcare system more effectively. Embrace these changes, stay informed, and take control of your healthcare journey!
Q&A
What are the privacy risks associated with telehealth?
Telehealth involves sharing personal health information electronically, so it’s crucial to choose reputable providers with strong data security measures. Be mindful of the platform’s privacy policy and ensure your connection is secure.
How can I find a telehealth provider?
Many healthcare systems and individual doctors offer telehealth services. Check your insurance provider’s website for a list of in-network providers, or search online for telehealth platforms specializing in your needs.
Is all data from wearable tech accurate?
The accuracy of wearable technology varies widely depending on the device and the metric being tracked. While they can be helpful for tracking trends, they shouldn’t replace professional medical advice or diagnosis.
How can I access my medical records online?
Many healthcare providers offer online patient portals where you can access your medical records, test results, and appointment information. Contact your doctor’s office to inquire about access to your online portal.