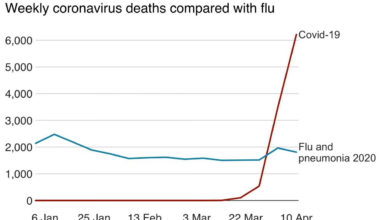
COVID-19 Public Health Emergency Ends
Covid 19 public health emergency ends – COVID-19 Public Health Emergency Ends: The world is breathing a collective sigh of relief, but the impact of the pandemic’s official end is far from over. From the lingering effects on healthcare systems and the economy to the ongoing mental health challenges and the need for stronger pandemic preparedness, the legacy of COVID-19 is complex and multifaceted. This post explores the various ways the end of the emergency declaration continues to shape our world.
We’ll delve into the significant changes in healthcare resource allocation, the economic consequences for businesses and individuals, and the lasting social and psychological impacts on communities worldwide. We’ll also examine the lessons learned and the crucial adjustments needed in public health policies to better prepare for future health crises. Get ready for a deep dive into the post-emergency landscape.
Impact on Healthcare Systems: Covid 19 Public Health Emergency Ends

Source: tegna-media.com
The end of the COVID-19 public health emergency marked a significant turning point for healthcare systems worldwide. While the immediate crisis had passed, the lingering effects on hospital capacity, staffing, resource allocation, and overall preparedness continue to shape the landscape of healthcare delivery. The transition has been complex, requiring careful strategic planning and adaptation to meet evolving needs.
Changes in Hospital Capacity and Staffing Levels
The initial surge in COVID-19 patients overwhelmed many hospitals, leading to a significant expansion of capacity through the conversion of existing spaces and the construction of temporary facilities. Following the emergency declaration, many hospitals scaled back these expansions, returning to pre-pandemic bed numbers. This reduction, however, has not always been matched by a corresponding decrease in demand for services, leading to ongoing challenges with capacity in certain areas and specialties.
Staffing levels also experienced significant fluctuations. The burnout and attrition experienced by healthcare workers during the pandemic continue to impact staffing shortages, particularly among nurses and physicians. Recruitment and retention strategies are now critical to address this ongoing challenge.
Shift in Healthcare Resource Allocation
During the public health emergency, a substantial portion of healthcare resources were diverted towards COVID-19 response efforts. This included the allocation of personal protective equipment (PPE), ventilators, and medications, as well as the prioritization of COVID-19 testing and treatment. The shift away from this focused approach has required a reassessment of resource allocation, with a focus on restoring services in other areas that were neglected or delayed during the pandemic.
This includes addressing the backlog of elective procedures and managing the ongoing mental health crisis exacerbated by the pandemic. The process of reallocating resources is ongoing and presents unique challenges for healthcare administrators.
Potential Long-Term Effects on Healthcare Infrastructure and Preparedness
The COVID-19 pandemic exposed vulnerabilities in healthcare infrastructure and preparedness, highlighting the need for improvements in several key areas. The long-term effects may include a greater emphasis on telehealth and remote patient monitoring, improved surge capacity planning to handle future outbreaks, and a strengthened focus on public health infrastructure. Investment in robust data systems for tracking disease outbreaks and improved communication channels between healthcare providers and public health agencies will also be crucial.
The pandemic underscored the need for flexible and resilient healthcare systems capable of adapting to unforeseen crises.
Healthcare System Performance Comparison
| Metric | Before COVID-19 | During COVID-19 Peak | Post COVID-19 PHE |
|---|---|---|---|
| Hospital Bed Occupancy Rate | ~70% (average, varies by region) | >90% in many areas; significant shortages reported | Variable; some areas still experience high occupancy; others have returned to pre-pandemic levels |
| Staffing Levels (Nursing) | Adequate in many areas, but shortages in some specialties | Significant shortages due to burnout, illness, and attrition | Ongoing shortages; recruitment and retention remain critical challenges |
| Elective Procedure Backlog | Minimal | Substantial delays and cancellations | Significant backlog remains; gradual clearing through increased capacity and prioritization |
| Mental Health Service Utilization | Increasing trend pre-pandemic | Significant increase due to pandemic stress | Continued high demand; increased focus on mental health services needed |
Economic Consequences
The end of the COVID-19 public health emergency, while signifying a return to normalcy, carries significant economic ramifications. The lingering effects of the pandemic, coupled with the sudden shift in government support and public health measures, created a complex economic landscape with both positive and negative consequences for businesses and individuals. Understanding these impacts is crucial for navigating the ongoing economic recovery.The termination of the public health emergency led to a ripple effect across various sectors, impacting unemployment rates, economic growth, and specific industries.
While some sectors experienced a rebound, others continue to grapple with the long-term consequences of the pandemic. This analysis explores the multifaceted economic impacts and their implications for the future.
Unemployment Rates and Economic Growth
The initial stages of the pandemic saw a sharp increase in unemployment rates as businesses shut down and economic activity plummeted. Government stimulus packages, such as enhanced unemployment benefits and the Paycheck Protection Program (PPP), helped mitigate some of the immediate impacts. However, the end of these programs, coupled with lingering economic uncertainty, led to a more nuanced picture of unemployment recovery.
For example, while the overall unemployment rate decreased, certain demographics, such as low-wage workers and those in service industries, experienced prolonged unemployment. Economic growth, measured by indicators like GDP, also experienced a volatile period, with initial sharp contractions followed by uneven recovery. The speed and strength of the recovery varied significantly across different regions and sectors, highlighting the heterogeneous nature of the economic impact.
The long-term impact on economic growth remains uncertain, with factors like inflation and supply chain disruptions continuing to play a significant role.
Impact on Specific Industries
The tourism and hospitality sectors were among the hardest hit during the pandemic. Travel restrictions, lockdowns, and social distancing measures led to a dramatic decline in revenue and widespread job losses. Even with the end of the public health emergency, these industries face ongoing challenges, including lingering travel hesitancy, reduced consumer spending, and increased operating costs. For instance, many hotels and restaurants experienced significant financial losses during the pandemic and are still struggling to recover pre-pandemic levels of business.
The aviation industry also suffered immensely, with many airlines forced to reduce flights and lay off staff. The recovery in these sectors is expected to be gradual, with ongoing challenges related to labor shortages and changing consumer behavior. Other industries, such as healthcare and technology, experienced contrasting trends, with some sectors thriving while others faced specific challenges.
Long-Term Economic Implications
The long-term economic implications of the pandemic and the end of the public health emergency are complex and multifaceted. Increased national debt due to government spending on pandemic relief measures poses a significant challenge for long-term fiscal sustainability. Supply chain disruptions and inflationary pressures continue to impact businesses and consumers. The pandemic also accelerated the adoption of remote work and e-commerce, leading to significant shifts in labor markets and consumer behavior.
These changes will likely have long-lasting effects on the structure and dynamics of the economy. Furthermore, the pandemic highlighted existing inequalities, exacerbating existing disparities in wealth, health, and access to opportunities. Addressing these inequalities will be crucial for ensuring a just and equitable economic recovery. Predicting the exact trajectory of the long-term economic consequences remains difficult, but understanding the interplay of these factors is crucial for informed policymaking and strategic planning.
Public Health Preparedness
The COVID-19 pandemic exposed critical weaknesses in global and national public health preparedness. While healthcare systems struggled with immediate patient care, the pandemic highlighted the urgent need for systemic improvements in surveillance, response protocols, and resource allocation to effectively mitigate future outbreaks. Lessons learned must translate into concrete action to strengthen our collective resilience against future pandemics.
Lessons Learned from COVID-19
The COVID-19 pandemic offered stark reminders of the interconnectedness of global health security. Early warning systems proved insufficient, leading to delayed responses. Supply chain vulnerabilities became evident, particularly regarding personal protective equipment (PPE) and testing materials. Furthermore, inconsistent messaging and a lack of trust in public health authorities hampered effective communication and compliance with public health measures.
The pandemic also highlighted existing health inequities, with disproportionate impacts on vulnerable populations. These disparities underscore the need for equitable resource allocation and culturally sensitive communication strategies. Finally, the rapid spread of misinformation and disinformation online significantly complicated the public health response.
Improvements Needed in Surveillance Systems and Disease Response Protocols
Effective pandemic preparedness necessitates robust surveillance systems capable of detecting and tracking emerging infectious diseases rapidly. This includes enhancing laboratory capacity for rapid pathogen identification and genomic sequencing, expanding disease surveillance networks to incorporate diverse data sources (including wastewater surveillance), and strengthening international collaboration to share information and coordinate responses. Improved response protocols should include standardized guidelines for testing, isolation, contact tracing, and treatment, as well as clear escalation procedures for managing outbreaks at local, national, and international levels.
Regular pandemic preparedness exercises and drills are also crucial for testing and refining these protocols.
Plan for Future Pandemic Preparedness
A comprehensive plan for future pandemic preparedness must prioritize resource allocation and communication strategies. This includes investing in a robust public health workforce with adequate training and resources, establishing strategic stockpiles of essential medical supplies, and developing flexible healthcare systems capable of scaling up to meet surges in demand. Clear and consistent communication strategies are essential to build public trust and ensure adherence to public health measures.
This involves utilizing multiple communication channels to reach diverse populations, addressing misinformation proactively, and fostering transparency and accountability in public health decision-making. The plan should also include mechanisms for equitable resource allocation, ensuring that vulnerable populations receive adequate support and protection. For example, investing in community-based healthcare providers and addressing social determinants of health can significantly enhance pandemic preparedness and response in underserved communities.
Key Recommendations for Strengthening Public Health Infrastructure
Strengthening public health infrastructure requires a multi-faceted approach. This includes:
- Increased funding for public health agencies at all levels.
- Expansion of the public health workforce with appropriate training and incentives.
- Investment in advanced surveillance technologies and data analytics.
- Development of robust supply chains for essential medical supplies and equipment.
- Strengthening international collaboration and information sharing.
- Implementation of effective communication strategies to build public trust and promote health literacy.
- Addressing health inequities through targeted interventions and equitable resource allocation.
- Regular pandemic preparedness exercises and drills to test response capabilities.
Social and Psychological Impacts
The COVID-19 pandemic cast a long shadow, extending far beyond the immediate health crisis. Its impact on the social and psychological well-being of individuals and communities continues to unfold, revealing complex and multifaceted consequences that demand sustained attention and proactive interventions. The prolonged period of uncertainty, isolation, and grief has left an indelible mark on mental health globally.The pandemic exacerbated existing mental health challenges while creating new ones.
Increased rates of anxiety, depression, and post-traumatic stress disorder (PTSD) were observed across various demographics. The economic hardship, job losses, and disruptions to education and social support networks further compounded these issues, particularly affecting vulnerable populations like the elderly, low-income families, and essential workers who faced heightened risks and stressors. Furthermore, the constant barrage of negative news and the ever-shifting public health guidelines contributed to a pervasive sense of fear and uncertainty, impacting overall mental and emotional well-being.
Challenges in Addressing Pandemic-Related Mental Health Issues
Addressing the mental health fallout from the pandemic presents significant challenges. Firstly, there is a substantial gap in access to mental healthcare services, particularly in underserved communities. Many individuals lack insurance coverage or face geographical barriers that limit access to qualified professionals. Secondly, the stigma associated with mental illness often prevents individuals from seeking help, even when they are experiencing significant distress.
So, the COVID-19 public health emergency is finally over. It’s a huge shift, and while we’re moving on, it’s interesting to consider the long-term health impacts. For example, I was reading a report on the soaring costs of GLP-1 medications for weight loss among Medicare beneficiaries, check out this insightful piece from KFF: medicare glp1 spending weight loss kff.
It makes you wonder about the long-term budgetary implications as we emerge from the pandemic and face new health challenges.
Thirdly, the sheer scale of the need has overwhelmed existing mental health systems, leading to long wait times and limited resources. Finally, the long-term effects of the pandemic on mental health are still emerging, requiring ongoing monitoring and adaptable interventions.
Community-Based Initiatives Supporting Mental Health and Well-being
Numerous community-based initiatives have emerged to address the mental health needs arising from the pandemic. These initiatives often leverage existing community resources and networks to provide accessible and culturally sensitive support. For example, many community centers and faith-based organizations have organized support groups and peer-to-peer counseling programs to foster a sense of connection and shared experience. Some initiatives have focused on providing telehealth services to overcome geographical barriers and increase access to mental healthcare.
Other programs have focused on promoting mindfulness and stress reduction techniques through online resources and workshops. A successful example is the widespread adoption of virtual support groups, allowing individuals to connect with others facing similar challenges from the comfort and safety of their homes. These initiatives highlight the crucial role of community engagement in building resilience and promoting mental well-being.
Strategies for Promoting Social Cohesion and Resilience
The pandemic underscored the importance of social cohesion and community resilience in navigating crises. Strengthening these aspects is crucial for long-term recovery.
- Invest in accessible and affordable mental health services: Expanding access to mental healthcare, particularly in underserved communities, is paramount. This includes increasing the number of mental health professionals, providing telehealth options, and reducing the stigma associated with mental illness.
- Promote social connection and community engagement: Supporting community-based initiatives that foster social interaction and a sense of belonging is vital. This can include funding for community centers, supporting volunteer programs, and promoting intergenerational activities.
- Strengthen social safety nets: Robust social safety nets are crucial for providing economic support and reducing stress during times of crisis. This includes unemployment benefits, affordable housing, and access to food security programs.
- Promote public awareness and education: Raising public awareness about mental health issues and reducing stigma is essential. This can involve public health campaigns, educational programs in schools and workplaces, and promoting open conversations about mental health.
- Invest in research and data collection: Continued research is needed to understand the long-term impacts of the pandemic on mental health and to develop effective interventions. This includes collecting data on mental health outcomes across various populations and evaluating the effectiveness of different interventions.
Changes in Public Policy
The end of the COVID-19 public health emergency marked a significant shift in public health policies worldwide. Governments transitioned from emergency response measures to a more sustainable approach, integrating lessons learned into long-term strategies. This involved a complex process of amending, repealing, and implementing new regulations, impacting various sectors of society.The shift from emergency to sustained public health management involved a reassessment of the balance between individual liberties and collective well-being.
So, the COVID-19 public health emergency is finally over, right? It feels like a monumental shift, and I’m curious how healthcare will adapt. This new focus on preventative care is interesting, especially with the CMS launching a primary care Medicare model ACO, as detailed in this article: cms launches primary care medicare model aco. Hopefully, this shift will help us build a more resilient system, ready for whatever comes next after the COVID-19 pandemic.
It’ll be fascinating to see how this impacts long-term healthcare strategies post-emergency.
Pre-emergency policies focused primarily on routine disease surveillance and prevention, with limited capacity for rapid, large-scale responses. The pandemic highlighted critical gaps in preparedness and response capabilities, necessitating substantial policy adjustments.
Changes in Public Health Surveillance and Reporting
Post-emergency public health policies emphasized enhanced surveillance systems for infectious diseases. This includes improved data collection, analysis, and reporting mechanisms, allowing for quicker identification and response to future outbreaks. For example, many countries invested in advanced digital tools to track disease spread, enabling faster communication and coordination among healthcare providers and public health authorities. Pre-emergency systems often lacked the real-time capabilities and interoperability necessary to effectively manage a pandemic.
The enhanced systems, however, are not without their challenges, including data privacy concerns and the need for ongoing technological upgrades and workforce training.
Modification of Healthcare Resource Allocation
The pandemic exposed significant disparities in healthcare access and resource allocation. Post-emergency policies aim to address these inequities by increasing funding for under-resourced healthcare facilities and communities, particularly those disproportionately affected by COVID-19. This includes strengthening telehealth infrastructure to improve access to care for remote and underserved populations. Before the pandemic, many healthcare systems operated under a model prioritizing acute care over preventative measures and long-term care needs.
The shift towards a more equitable and resilient system requires significant investment and policy reform. For instance, the increased focus on telehealth services, while beneficial, also requires addressing digital literacy disparities to ensure equitable access.
Adjustments to Pandemic Preparedness Plans
Lessons learned during the COVID-19 pandemic led to significant adjustments in national and international pandemic preparedness plans. This includes increased stockpiling of essential medical supplies, development of more robust testing and treatment protocols, and improved communication strategies to effectively inform and engage the public during future health crises. Pre-emergency plans often lacked the necessary flexibility and scalability to respond to a rapidly evolving pandemic.
The new plans emphasize greater coordination between different levels of government, healthcare providers, and community organizations. For example, many countries have developed more comprehensive plans for managing mass vaccination campaigns, incorporating lessons learned from the challenges faced during the COVID-19 vaccine rollout.
Impact of Policy Changes on Vulnerable Populations
Policy changes following the COVID-19 emergency significantly impact vulnerable populations. For instance, continued investment in healthcare infrastructure and equitable access to care directly benefits individuals with pre-existing conditions, low-income families, and marginalized communities who were disproportionately affected by the pandemic. Similarly, policies aimed at improving access to mental health services address the lasting psychological impacts on vulnerable groups.
However, the success of these policies depends on effective implementation and ongoing monitoring to ensure they reach the intended beneficiaries. A potential challenge lies in ensuring that these policies are not only implemented but also sustained in the long term, to avoid a return to pre-pandemic inequalities. This necessitates sustained political will and continued investment in social safety nets.
Long-Term Health Effects of COVID-19

Source: nyt.com
The COVID-19 pandemic, while seemingly receding from the headlines, continues to leave a significant mark on global health. Beyond the immediate acute symptoms, a substantial portion of those infected experience lingering health problems, collectively known as “long COVID” or Post-COVID-19 Condition. Understanding these long-term effects is crucial for developing effective treatment strategies and supporting those affected.Long COVID encompasses a wide range of persistent symptoms that can emerge weeks or months after the initial infection, even in individuals who had mild or asymptomatic cases.
These symptoms vary greatly between individuals, making diagnosis and treatment challenging. Known long-term consequences include fatigue, shortness of breath, cognitive dysfunction (“brain fog”), heart palpitations, chest pain, and persistent cough. Less common, but still significant, are neurological problems such as loss of smell or taste (anosmia and ageusia), and even more serious conditions like kidney and liver damage.
The potential long-term impact on cardiovascular health is a particular area of concern, with studies showing an increased risk of heart conditions even in young adults previously free of such problems. The exact mechanisms driving these long-term effects are still under investigation, but ongoing research points to several possibilities, including persistent inflammation, damage to various organ systems, and autoimmune responses.
Ongoing Research into Long COVID and its Management
Research efforts globally are focused on understanding the pathophysiology of long COVID, identifying reliable diagnostic markers, and developing effective treatments. Large-scale studies are tracking the long-term health outcomes of COVID-19 survivors, comparing them to control groups to pinpoint the specific risks and prevalence of various long-term complications. Researchers are exploring different therapeutic approaches, including rehabilitation programs, medications to manage specific symptoms (such as fatigue or cognitive impairment), and investigating the potential of repurposed drugs.
For example, studies are examining the role of antiviral medications, immunomodulators, and anticoagulants in mitigating long-term complications. Furthermore, research is investigating the effectiveness of various rehabilitation therapies, such as pulmonary rehabilitation for respiratory problems and cognitive rehabilitation for brain fog.
Implications for Healthcare Systems in Addressing Long-Term COVID-19 Care, Covid 19 public health emergency ends
The surge in long COVID cases presents a significant challenge to healthcare systems worldwide. The diverse range of symptoms and the lack of standardized diagnostic tools and treatments require a multidisciplinary approach to care. Healthcare systems need to invest in specialized clinics and support networks to provide comprehensive assessment and management of long COVID. This includes establishing dedicated long COVID clinics staffed by specialists from various medical fields, such as pulmonology, cardiology, neurology, and rehabilitation medicine.
Furthermore, healthcare systems need to develop strategies for early identification and referral of individuals with persistent symptoms following COVID-19 infection. This might involve incorporating screening tools into primary care settings to identify potential long COVID cases and facilitate timely access to specialized care. The financial burden of providing long-term care for a potentially large population of long COVID patients is also a substantial concern, requiring careful resource allocation and policy adjustments.
Support Services Available for Individuals with Long COVID
Several support services are emerging to assist individuals navigating the challenges of long COVID. Many organizations are providing information and resources on managing symptoms, connecting patients with healthcare professionals, and facilitating access to clinical trials. Support groups, both online and in-person, offer a vital platform for individuals to share their experiences, learn coping strategies, and receive emotional support from others facing similar challenges.
So, the COVID-19 public health emergency is finally over, right? But the healthcare landscape is still shaky. I was reading about the struggles faced by Steward Health Care, and their potential Ohio hospital closures, with a Pennsylvania facility also steward ohio hospitals closures pennsylvania facility at risk , which makes you wonder how much the pandemic’s strain truly contributed to this instability.
It really highlights that while the emergency is declared over, the health challenges linger. The long-term effects of COVID-19 on our healthcare system are going to be felt for years to come.
These groups can be invaluable for reducing feelings of isolation and providing a sense of community. Moreover, some organizations are advocating for policy changes to improve access to healthcare and disability benefits for individuals with long COVID. These efforts aim to ensure that those affected have the necessary support to manage their condition and participate fully in society.
Examples include patient advocacy groups pushing for better insurance coverage for long COVID treatments and rehabilitation services.
Global Implications
The end of the COVID-19 public health emergency marks a significant turning point, not just for individual nations, but for the global community as a whole. The pandemic exposed vulnerabilities in international cooperation, highlighted disparities in healthcare access, and reshaped global economic landscapes. Understanding the lasting global implications is crucial for building a more resilient and equitable future.The varied responses of different countries to the pandemic offer a complex case study in global health governance.
Some nations prioritized swift and stringent lockdowns, while others adopted more targeted measures or implemented less restrictive approaches. These diverse strategies yielded varying levels of success in controlling the virus’s spread and mitigating its economic and social impacts, underscoring the influence of factors such as governmental capacity, public health infrastructure, and societal compliance.
International Cooperation and Global Health Security
The COVID-19 pandemic severely tested the capacity for international cooperation in responding to a global health crisis. Initial delays in information sharing and the uneven distribution of vaccines highlighted the need for improved mechanisms for coordinated global action. While some collaborative efforts, such as the development of multiple COVID-19 vaccines through international research partnerships, proved successful, significant challenges remained in ensuring equitable access to these life-saving resources.
The pandemic exposed weaknesses in the existing international health architecture, prompting calls for reform and strengthened global health security mechanisms to better prepare for future pandemics. Examples include improved surveillance systems, enhanced capacity for rapid response, and more robust mechanisms for equitable resource allocation.
Global Economic Impacts
The pandemic’s economic repercussions were felt worldwide, although the severity varied considerably across nations. Supply chain disruptions, lockdowns, and decreased consumer spending led to global recessionary pressures. The recovery has been uneven, with some countries bouncing back more quickly than others, largely depending on pre-existing economic strength, access to financial resources, and the effectiveness of government stimulus packages.
Developing nations, particularly those heavily reliant on tourism or international trade, faced disproportionately severe economic challenges. For example, many small island developing states saw their economies severely impacted due to the collapse of the tourism sector, highlighting the interconnectedness of global economies and the unequal distribution of pandemic-related economic burdens.
A Visual Representation of Global Impact
Imagine a world map. Each country is shaded according to the severity of its COVID-19 impact, ranging from a pale yellow (minimal impact) to deep red (severe impact). The darker shades cluster in regions with weaker healthcare systems, limited access to resources, or higher population densities. Interconnecting lines represent global supply chains, some thick and vibrant (representing strong, resilient supply chains), others thin and faded (representing disrupted or fragile chains).
A network of thinner lines connecting countries represents international cooperation efforts – some lines are bold and bright, signifying strong collaborations, while others are faint and broken, reflecting challenges in coordinated global responses. This visualization demonstrates the uneven and interconnected nature of the pandemic’s global impact.
Ending Remarks
The end of the COVID-19 public health emergency marks not an ending, but a transition. While the immediate crisis has subsided, the long-term effects on global health, economies, and societies will be felt for years to come. Understanding these lasting impacts is crucial for building a more resilient and prepared future. Let’s learn from the past, adapt to the present, and strive to create a healthier tomorrow.
General Inquiries
Will my health insurance still cover COVID-19 treatment?
Coverage may vary depending on your insurance plan and location. Check with your provider for the most up-to-date information.
What long-term health effects are still being studied?
Ongoing research focuses on “long COVID,” including fatigue, brain fog, and cardiovascular issues. More research is needed to fully understand these effects.
Are there still any COVID-19 related travel restrictions?
Travel restrictions are largely lifted globally, but it’s always wise to check the specific requirements of your destination before traveling.
What can I do to protect myself from future outbreaks?
Maintain good hygiene, get vaccinated and boosted against COVID-19 and other illnesses, and stay informed about public health guidelines.