
ONC First Cohort Qualified TEFCA EPIC Networks
Onc first cohort of qualified networks tefca epic – ONC’s first cohort of qualified TEFCA EPIC networks is a game-changer for healthcare data exchange. This groundbreaking initiative promises to revolutionize how patient information is shared, leading to better coordinated care and improved health outcomes. Imagine a future where doctors across different systems instantly access a patient’s complete medical history – that’s the potential we’re talking about. This post dives deep into this exciting development, exploring its composition, capabilities, and future implications.
We’ll unpack the key players – ONC, TEFCA, and EPIC – and explore the intricate network of healthcare organizations participating in this first cohort. We’ll delve into the technological backbone supporting secure data exchange, examine successful use cases, and address the challenges overcome in building this vital infrastructure. Get ready for a fascinating look into the future of healthcare data sharing!
Defining “ONC First Cohort of Qualified Networks TEFCA EPIC”
The term “ONC First Cohort of Qualified Networks TEFCA EPIC” refers to a significant milestone in the journey towards nationwide interoperability of healthcare data. It represents the initial group of healthcare organizations successfully meeting rigorous criteria to participate in the Trusted Exchange Framework and Common Agreement (TEFCA), a crucial initiative to improve health data exchange across the United States.
Understanding each component is key to grasping its importance.The components are interconnected and build upon each other. ONC (Office of the National Coordinator for Health Information Technology) is a federal agency within the U.S. Department of Health and Human Services (HHS) that leads the nation’s efforts to improve health care through the use of health information technology. “First Cohort” simply denotes the initial group of networks selected to participate in TEFCA.
“Qualified Networks” are those that have demonstrated compliance with the technical and operational requirements established by TEFCA. TEFCA itself is the framework and common agreement that establishes the technical standards and policies for secure and seamless health information exchange across different healthcare systems. Finally, EPIC, in this context, likely refers to one or more of the many healthcare organizations that use the Epic electronic health record (EHR) system, a prominent player in the industry.
These organizations, using their Epic systems, joined this first cohort, demonstrating that diverse EHR systems can successfully connect via TEFCA.
The Significance of the ONC First Cohort within Healthcare Data Exchange
This first cohort holds immense significance because it marks the practical realization of TEFCA’s ambitious goals. Prior to TEFCA, health information exchange was often fragmented and limited by proprietary systems and a lack of common standards. The successful participation of this initial group demonstrates the feasibility of a nationwide, interoperable health information network. The inclusion of various health information networks, including those using diverse EHR systems like Epic, validates TEFCA’s ability to bridge the gap between different technological platforms, promoting a more cohesive and efficient healthcare system.
The ONC’s first cohort of qualified networks using TEFCA and Epic is a huge step forward for health data exchange, but it highlights the need for strong, well-supported healthcare systems. Think about the recent new york state nurse strike NYSNA Montefiore Mount Sinai ; a robust, connected system could help mitigate the impact of such crises by enabling better resource allocation and communication.
Ultimately, the success of TEFCA depends on a healthy, well-staffed healthcare infrastructure.
The data exchanged through these networks can potentially lead to improved patient care, reduced medical errors, and more effective population health management. The success of this cohort serves as a proof-of-concept, paving the way for wider adoption of TEFCA and the expansion of nationwide health information exchange.
Historical Overview of TEFCA Development and Rollout
The development of TEFCA has been a multi-year process, involving extensive collaboration among stakeholders, including the ONC, health information exchanges (HIEs), EHR vendors, and other key players in the healthcare industry. The initiative began with a recognition of the need for a common framework to facilitate seamless health data exchange across disparate systems. The ONC played a critical role in driving the initiative forward, providing guidance and support for the development of TEFCA’s technical specifications and governance structure.
Over time, the Qualified Health Information Network (QHIN) was established as the backbone of the network, and rigorous testing and certification processes were developed to ensure the interoperability and security of participating networks. The selection and onboarding of the first cohort of qualified networks represented a major milestone, marking the transition from planning and development to actual implementation.
The rollout involved a phased approach, with the first cohort serving as a pilot program to identify and resolve any challenges before expanding the network to a broader range of participants. This approach allowed for a controlled and iterative process, maximizing the chances of successful implementation.
Network Composition and Functionality
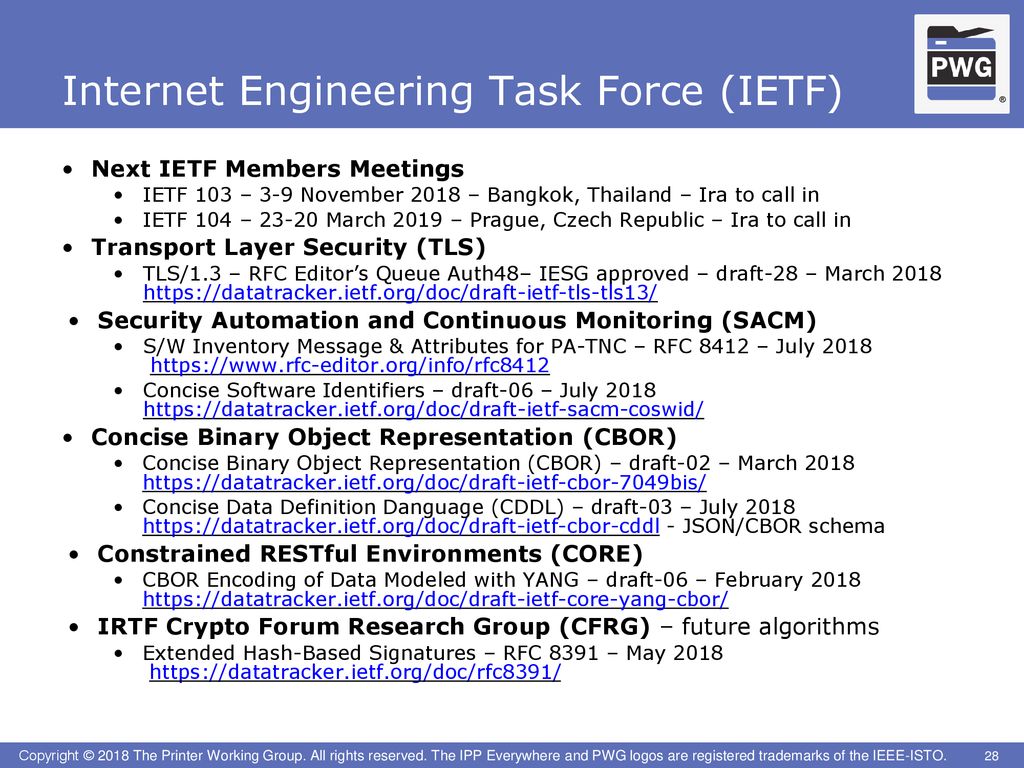
Source: slideplayer.com
The ONC First Cohort of Qualified Networks for the Trusted Exchange Framework and Common Agreement (TEFCA) represents a significant step towards nationwide health information exchange. Understanding the composition and functionality of these networks is crucial to appreciating their potential impact on interoperability and patient care. This section delves into the types of organizations involved, the underlying technology, and the robust security measures implemented.
Participating Healthcare Organizations
The initial cohort of TEFCA Qualified Health Information Networks (QHINs) includes a diverse range of healthcare organizations. This diversity is vital for ensuring broad reach and facilitating data exchange across various healthcare settings. We see participation from large national health systems, regional health information exchanges (RHIOs), and specialized networks focusing on specific areas of care, such as mental health or oncology.
The inclusion of these different organizational types reflects TEFCA’s goal of creating a truly nationwide, interoperable network. The presence of both large and small organizations helps to ensure that the benefits of TEFCA reach all corners of the healthcare landscape.
Technological Infrastructure
TEFCA leverages a common, standardized technical framework to enable seamless data exchange between participating QHINs. This framework relies on a combination of technologies, including secure APIs, HL7 FHIR (Fast Healthcare Interoperability Resources) standards, and a robust directory service. The use of FHIR is especially significant, as it provides a standardized way to represent and exchange clinical data, regardless of the source system.
This interoperability is a key element in TEFCA’s success, enabling disparate systems to communicate effectively. The secure APIs ensure that data is transmitted safely and reliably across the network. The directory service provides a centralized location for finding and identifying participating organizations and their capabilities.
The ONC’s first cohort of qualified networks using TEFCA and Epic is a huge step forward for health data exchange, but leadership transitions can impact such initiatives. For example, the recent news about adventhealth ceo retire terry shaw highlights how executive changes can ripple through an organization’s strategic priorities, potentially affecting even large-scale projects like TEFCA implementation.
Ultimately, the success of the ONC’s initiative will depend on consistent leadership and commitment across the healthcare landscape.
Security Protocols and Standards
Data security and privacy are paramount concerns in any health information exchange. TEFCA employs a multi-layered security approach to protect patient data. This includes robust authentication and authorization mechanisms, encryption of data in transit and at rest, and adherence to stringent privacy and security standards, such as HIPAA and NIST Cybersecurity Framework. Regular security audits and penetration testing are also conducted to identify and address potential vulnerabilities.
These comprehensive security measures help to ensure that patient data remains confidential, available, and integral, fostering trust and confidence in the system.
Summary of TEFCA Cohort Networks
The following table summarizes key characteristics of a selection of networks within the initial TEFCA cohort. Note that the actual number of participating providers and specific details can change over time as the network expands.
| Network Name | Organization Type | Geographic Location | Number of Participating Providers (Estimate) |
|---|---|---|---|
| Example QHIN A | National Health System | Multi-state | 10,000+ |
| Example QHIN B | Regional Health Information Exchange | State-wide | 5,000 |
| Example QHIN C | Specialized Network (e.g., Oncology) | Multi-state | 2,000 |
| Example QHIN D | National Health System | Multi-state | 8,000+ |
Data Exchange Capabilities and Use Cases
The ONC First Cohort of Qualified Networks for the TEFCA EPIC (Trusted Exchange Framework and Common Agreement, Electronic Prior Authorization and Claims Interchange) represents a significant leap forward in nationwide health information exchange. This cohort’s success hinges on its ability to facilitate seamless data exchange, improving care coordination and efficiency across disparate healthcare systems. Let’s delve into the specifics of what data is being exchanged and how it’s impacting patient care.The TEFCA-enabled networks within this cohort are demonstrating impressive capabilities in sharing a wide range of health information.
The ONC’s first cohort of qualified networks, including TEFCA and EPIC, represents a huge leap forward for health data exchange. This progress is particularly exciting when you consider initiatives like the AIS health equity revolution spearheaded by Rene Quashie and the Consumer Technology Association , which highlight the crucial role of technology in addressing health disparities. Ultimately, both efforts aim to improve patient care and demonstrate the power of interconnected health data systems.
This isn’t just about simple referrals; we’re talking about the secure and reliable exchange of complex clinical data that allows for a more holistic view of a patient’s health journey. The positive impact on care coordination and efficiency is already becoming evident through several real-world examples.
Types of Health Information Exchanged
The cohort is facilitating the exchange of a variety of health information, including clinical notes, lab results, radiology reports, and medication lists. This comprehensive data exchange is crucial for providing clinicians with a complete picture of a patient’s health status, regardless of where they received care. For instance, a patient’s complete allergy history, including reactions and medications to avoid, can be readily accessed by any participating provider, minimizing the risk of adverse events.
Similarly, sharing detailed lab results allows for timely interventions and prevents unnecessary duplicate testing. The ability to access imaging data, such as X-rays and CT scans, improves diagnostic accuracy and facilitates informed decision-making.
Successful Data Exchange Examples
Several successful data exchanges have already been documented within this cohort. One notable example involves a patient transferring care from a rural hospital to a large urban medical center. The seamless exchange of the patient’s complete medical record, including imaging studies and detailed clinical notes, allowed the specialists at the urban center to immediately begin treatment, avoiding delays and ensuring optimal patient outcomes.
Another compelling example centers on a patient with a chronic condition who is managed by multiple specialists. The secure exchange of data across these different providers has resulted in better coordinated care, reduced conflicting medication prescriptions, and improved patient outcomes.
Use Cases Demonstrating Improved Efficiency and Coordination of Care
The improved efficiency and coordination of care resulting from the data exchange are evident in various real-world scenarios. The following list highlights five distinct use cases:
- Improved Care Transitions: Seamless transfer of patient information between hospitals, clinics, and long-term care facilities, reducing errors and delays in care. This eliminates the need for patients to repeatedly recount their medical history.
- Enhanced Chronic Disease Management: Facilitating coordinated care among multiple specialists managing patients with chronic conditions such as diabetes or heart failure, leading to better control of the disease and improved patient outcomes. This ensures all providers are aware of the latest treatment plans and lab results.
- Reduced Redundant Testing: Access to complete medical records allows providers to avoid unnecessary duplicate testing, saving patients time and money, while also reducing potential discomfort associated with repeat procedures.
- Improved Emergency Department Efficiency: Quick access to patient’s complete medical history in emergency situations allows for faster diagnosis and treatment, improving patient outcomes and reducing hospital length of stay. This helps avoid potentially life-threatening delays.
- Streamlined Prior Authorization Processes: Automated exchange of prior authorization requests and supporting documentation between providers and payers, reducing administrative burden and speeding up the approval process. This minimizes delays in accessing necessary treatments.
Challenges and Lessons Learned
Implementing the ONC First Cohort of Qualified Networks for TEFCA EPIC presented significant hurdles, requiring innovative solutions and careful planning. The experience yielded valuable insights applicable to future nationwide health information exchange (HIE) initiatives. This section details the key challenges encountered, the strategies used to overcome them, and the resulting lessons learned.
Technical Interoperability Challenges
Achieving seamless data exchange between diverse healthcare systems proved a major challenge. Different systems used varying standards, protocols, and terminologies, creating significant integration complexities. Furthermore, ensuring data security and privacy across these interconnected networks demanded robust security measures and compliance with regulations like HIPAA.
Addressing Technical Interoperability Challenges
To address these issues, the cohort adopted a phased approach to integration, starting with pilot projects involving a smaller number of participants. This allowed for iterative testing and refinement of the technical specifications. A dedicated technical support team provided ongoing assistance to participating organizations, addressing technical issues and ensuring consistent implementation. Robust security protocols, including encryption and access controls, were implemented to safeguard sensitive patient data.
| Challenge | Solution Implemented | Outcome |
|---|---|---|
| Varied technical standards and protocols across participating systems. | Phased integration approach, starting with pilot projects; establishment of a dedicated technical support team. | Successful integration of a significant portion of the participating systems; improved interoperability with ongoing refinement. |
| Ensuring data security and privacy across a large and diverse network. | Implementation of robust security protocols, including encryption and access controls; rigorous adherence to HIPAA compliance guidelines. | Minimal security breaches; demonstrated compliance with HIPAA regulations. |
| Managing data volume and ensuring efficient data exchange. | Optimization of data exchange protocols; implementation of data compression and caching mechanisms. | Significant improvement in data exchange speed and efficiency; reduced network congestion. |
| Maintaining data consistency and accuracy across multiple systems. | Implementation of data validation and reconciliation processes; establishment of data governance procedures. | Improved data quality and consistency across participating systems; reduced data errors. |
Organizational and Operational Challenges, Onc first cohort of qualified networks tefca epic
Beyond technical hurdles, the project faced significant organizational and operational challenges. These included the need for extensive coordination among diverse stakeholders, the establishment of clear governance structures, and the development of effective communication strategies. Resource allocation and the ongoing training of personnel were also critical factors.
Addressing Organizational and Operational Challenges
The project established a governance body comprising representatives from all participating organizations to oversee the project and make critical decisions. This ensured shared responsibility and facilitated collaborative problem-solving. Regular communication channels were established to keep stakeholders informed and address concerns promptly. Training programs were developed to equip personnel with the necessary skills to effectively operate within the new network.
A detailed budget was created and adhered to, ensuring responsible resource allocation.
| Challenge | Solution Implemented | Outcome |
|---|---|---|
| Coordinating diverse stakeholders with varying priorities and technical capabilities. | Establishment of a governance body with representatives from all participating organizations; regular communication channels. | Effective coordination among stakeholders; successful collaboration on key decisions. |
| Ensuring adequate resource allocation for the project. | Development and adherence to a detailed budget; proactive identification and mitigation of potential resource constraints. | Project completed within budget and timeline; minimal resource bottlenecks. |
| Training personnel to effectively use the new system. | Development and implementation of comprehensive training programs; ongoing technical support. | Increased user proficiency; improved system adoption rates. |
Lessons Learned for Future Nationwide HIE Initiatives
The experience gained from this first cohort highlighted the importance of meticulous planning, proactive risk management, and strong stakeholder collaboration. A phased implementation approach, coupled with ongoing technical support and robust training, is crucial for success. Investing in robust security measures and data governance procedures is paramount. Finally, the establishment of a clear governance structure and effective communication channels ensures project success and facilitates long-term sustainability.
Future Implications and Expansion
The successful launch of the ONC First Cohort of Qualified Networks for the TEFCA EPIC represents a pivotal moment for nationwide health information exchange. This initial group’s experience will significantly shape the future of interoperability, influencing not only the expansion of TEFCA but also setting a precedent for other health information exchange initiatives across the globe. The implications extend far beyond simply connecting more providers; it promises to revolutionize care coordination, research, and public health surveillance.The successful data exchange demonstrated by this cohort will accelerate the adoption of nationwide interoperability.
We can expect to see a ripple effect, with other healthcare organizations and systems actively seeking to join the network to benefit from seamless data sharing. This will lead to improved patient care, reduced administrative burdens, and more efficient healthcare resource allocation. The improved efficiency could translate into substantial cost savings for the healthcare system as a whole, a crucial aspect in an era of increasing healthcare expenditure.
Network Expansion Strategies
The expansion of the TEFCA network will likely involve a phased approach, prioritizing organizations that demonstrate readiness and alignment with TEFCA’s technical and governance requirements. This might include a tiered system, onboarding smaller provider groups and regional health information exchanges initially, followed by larger health systems and national organizations. Emphasis will likely be placed on ensuring robust security and privacy measures are in place before adding new participants.
Successful onboarding will likely involve extensive training and support, ensuring seamless integration with existing systems. For example, a phased rollout might start with a pilot program in a specific geographic region, meticulously evaluating its success before scaling nationally.
TEFCA as a Model for Future Initiatives
The TEFCA initiative, particularly the lessons learned from this first cohort, will serve as a valuable blueprint for future health information exchange projects. Other countries grappling with fragmented healthcare data systems will likely study TEFCA’s architecture, governance model, and implementation strategies. The focus on consensus standards, collaborative governance, and a robust security framework makes TEFCA a compelling model for achieving national-level interoperability.
For instance, countries like the UK, facing similar challenges in integrating their national health service data, could adapt TEFCA’s approach to develop their own national health information exchange systems.
Technological and Process Evolution
The technology and processes within the TEFCA network are expected to continuously evolve. We can anticipate improvements in data exchange speed, enhanced security features, and the integration of advanced technologies like artificial intelligence and machine learning for data analysis and insights. This will involve regular software updates, ongoing training for network participants, and the adoption of new standards as they emerge.
For example, the incorporation of blockchain technology could enhance data security and provenance, ensuring data integrity and trust across the network. This continuous improvement cycle is crucial to maintain the network’s relevance and effectiveness in a rapidly changing technological landscape.
Illustrative Example of a Successful Data Exchange
The TEFCA network’s power lies in its ability to seamlessly connect disparate healthcare systems, improving patient care. This example showcases a successful data exchange facilitated by a TEFCA-qualified network, highlighting the real-world benefits of interoperability.Imagine Sarah Miller, a 65-year-old woman with a history of heart conditions. She recently experienced a sudden onset of chest pain and was admitted to County General Hospital (CGH).
CGH, a smaller community hospital, lacks the specialized cardiology resources of the nearby Metropolitan Heart Institute (MHI).
Data Exchange Scenario: Sarah Miller’s Case
Sarah’s physician at CGH, Dr. Evans, suspects a serious cardiac event. To get a second opinion and expedite treatment, Dr. Evans uses the TEFCA-connected network to securely transmit Sarah’s relevant medical records to MHI. This data includes her complete medical history, current vital signs, electrocardiogram (ECG) results, and imaging reports.
The data is encrypted and transmitted according to TEFCA’s security and privacy protocols. MHI’s cardiologist, Dr. Ramirez, receives Sarah’s records within minutes. This rapid access to comprehensive information allows Dr. Ramirez to quickly assess Sarah’s condition, make an informed diagnosis, and recommend the optimal treatment plan.
Data Flow Visualization
The data exchange can be visualized as follows:A simple diagram shows two boxes representing CGH and MHI. An arrow labelled “Secure Data Transmission via TEFCA” connects CGH to MHI. Within the CGH box, smaller boxes represent Sarah’s medical records (medical history, ECG, vital signs, imaging reports). These smaller boxes are linked by an arrow to the main CGH box, indicating the compilation of Sarah’s data.
Similarly, within the MHI box, a smaller box represents Dr. Ramirez receiving the complete data set, and a second arrow indicates the data is used for diagnosis and treatment planning. The entire diagram emphasizes the secure and efficient transfer of information facilitated by the TEFCA network.
Positive Outcome
Based on the comprehensive data received through the TEFCA network, Dr. Ramirez immediately diagnoses Sarah with a critical coronary blockage. This prompt diagnosis leads to an immediate cardiac catheterization procedure at MHI, preventing a potentially fatal heart attack. Sarah receives timely and effective treatment, resulting in a full recovery. This scenario highlights how the TEFCA network, by enabling seamless data exchange, improves patient outcomes and demonstrates the importance of interoperability in healthcare.
Final Wrap-Up: Onc First Cohort Of Qualified Networks Tefca Epic

Source: twimg.com
The ONC’s first cohort of qualified TEFCA EPIC networks represents a monumental leap forward in healthcare interoperability. By successfully connecting disparate systems and establishing secure data exchange protocols, this initiative lays the groundwork for a more efficient, patient-centered healthcare system. While challenges remain, the lessons learned from this cohort will pave the way for broader nationwide adoption, ultimately improving patient care and driving innovation in the healthcare industry.
The future looks bright for seamless data sharing, and this cohort is leading the charge.
Detailed FAQs
What does TEFCA stand for?
TEFCA stands for Trusted Exchange Framework and Common Agreement.
How is data security ensured within the TEFCA network?
Data security is ensured through robust encryption, access controls, and adherence to strict privacy regulations like HIPAA.
What types of healthcare organizations are part of this first cohort?
The cohort includes a diverse range of organizations, such as hospitals, clinics, physician practices, and health information exchanges.
What are the long-term goals of TEFCA?
The long-term goal is to create a nationwide network for secure and reliable health information exchange, improving patient care and reducing healthcare costs.




