
Where Are All the Nurses? Hospitals & Advocates Disagree
Where are all the nurses hospitals advocates disagree on crisis – Where Are All the Nurses? Hospitals & Advocates Disagree on the crisis – that’s the burning question facing healthcare today. It’s not just about empty beds and overworked staff; it’s about the future of patient care. This shortage isn’t evenly distributed; rural communities are often hit hardest, grappling with fewer resources and fewer applicants. Meanwhile, urban hospitals face their own unique challenges, from high patient volumes to competitive recruitment battles.
This post dives into the heart of the matter, exploring the perspectives of hospitals, advocacy groups, and the crucial role of education in addressing this critical issue.
We’ll examine the strategies hospitals are employing to attract and retain nurses – from competitive salaries and benefits to innovative work-life balance initiatives. But it’s not just about money; burnout and lack of support are also significant contributors to the problem. We’ll also look at how advocacy groups are pushing for policy changes, advocating for improved working conditions and increased funding for nursing education.
Ultimately, the goal is to find solutions that not only address the immediate crisis but also build a sustainable future for the nursing profession.
The Nursing Shortage: Where Are All The Nurses Hospitals Advocates Disagree On Crisis
Source: werpn.com
The nursing shortage in the United States is a multifaceted crisis impacting patient care, healthcare systems, and the well-being of nurses themselves. This shortage isn’t uniformly distributed; its severity varies significantly across geographical regions and specialties, leading to disparities in access to quality healthcare. Understanding the scope and distribution of this shortage is crucial for developing effective solutions.
Severity and Geographic Distribution of the Nursing Shortage
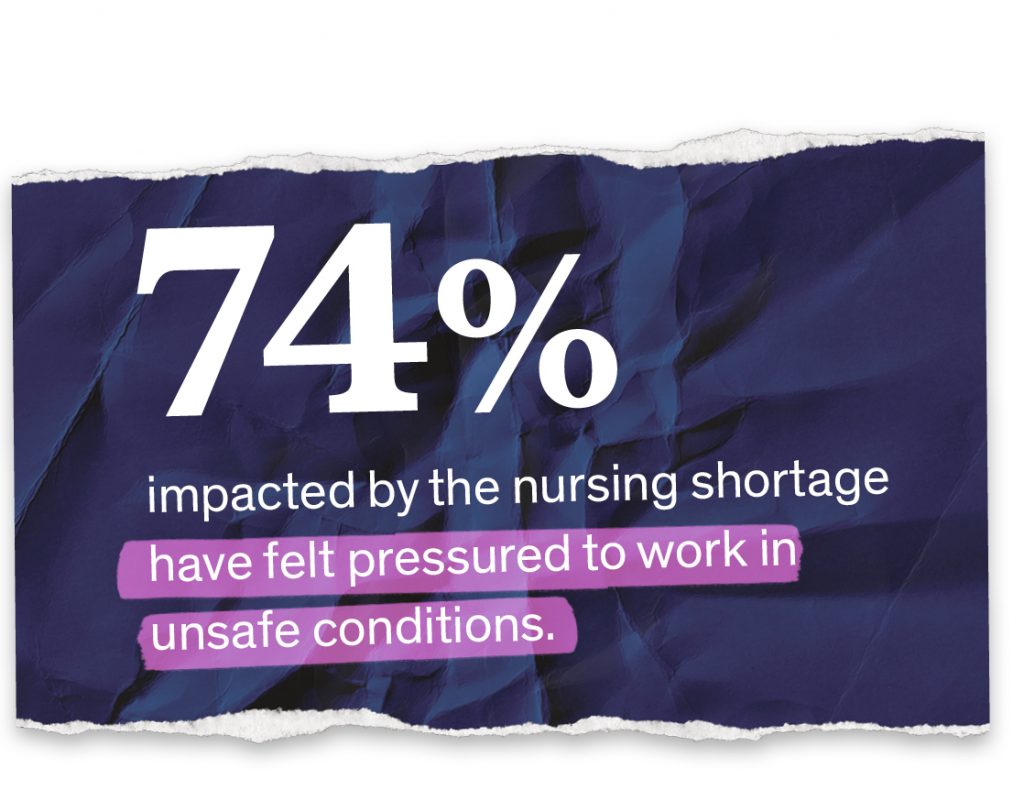
The severity of the nursing shortage is a complex issue, influenced by factors such as population demographics, healthcare system capacity, and economic conditions. Vacancy rates, often used as an indicator of shortage severity, fluctuate widely across states and even within states. For instance, rural areas consistently report higher vacancy rates than urban areas, exacerbating existing healthcare disparities. Nurse-to-patient ratios, another key metric, reflect the workload burden on nurses and the potential for compromised patient safety.
Lower ratios generally indicate a higher risk of burnout and errors. Data from the American Association of Colleges of Nursing (AACN) and the U.S. Bureau of Labor Statistics (BLS) consistently point to a significant and persistent shortfall. However, precise figures are difficult to obtain due to variations in data collection methods and reporting practices across different institutions.
The nursing shortage crisis has hospitals and advocates clashing over solutions; everyone agrees it’s dire, but opinions diverge wildly on the best approach. I was thinking about this, and it made me remember this fascinating article about how technology can actually boost empathy, enhanced human potential how customer service technology increases empathy , which got me wondering if similar tech could improve communication and patient care, potentially easing some of the current strain on the system.
Ultimately, addressing the nurse shortage requires a multi-pronged approach, but maybe technology can play a surprising role.
Urban vs. Rural Nursing Shortages
The nursing shortage manifests differently in urban and rural settings. Urban areas, while facing significant shortages, often have more resources and opportunities for recruitment and retention. However, high costs of living, intense competition for positions, and burnout contribute to high turnover rates. Rural areas, conversely, face a more critical shortage due to a combination of factors: lower pay, limited career advancement opportunities, geographic isolation, and a lack of amenities.
These challenges make it difficult to attract and retain nurses, leaving rural hospitals and clinics understaffed and struggling to provide adequate care. The aging population in many rural areas further exacerbates the problem, increasing the demand for nursing services without a corresponding increase in the supply of nurses.
Regional Breakdown of the Nursing Shortage
The following table provides a simplified overview of the nursing shortage across different regions. The data presented is a generalization and may not accurately reflect the specific situation in every hospital or healthcare facility within each region. Accurate data collection and reporting remain a significant challenge in assessing the true scope of the problem.
| Region | Vacancy Rate (Estimated) | Average Nurse-to-Patient Ratio (Estimated) | Contributing Factors |
|---|---|---|---|
| Northeast | 15-20% | 1:5 – 1:7 (varies widely by specialty and facility) | High cost of living, aging workforce, competition from other industries |
| South | 10-18% | 1:6 – 1:8 (varies widely by specialty and facility) | Growing population, increasing demand, limited number of nursing schools |
| Midwest | 12-17% | 1:5 – 1:7 (varies widely by specialty and facility) | Rural-urban disparity, aging population, lower salaries compared to coastal areas |
| West | 15-22% | 1:5 – 1:8 (varies widely by specialty and facility) | High cost of living, increasing demand, geographic isolation in rural areas |
Hospital Perspectives on the Nursing Crisis
The nursing shortage isn’t just a headline; it’s a daily reality reshaping hospital operations and impacting patient care. Hospitals, facing unprecedented pressure, are implementing a range of strategies to address the crisis, but the financial and operational challenges remain substantial. This section explores the hospital perspective, examining the multifaceted approaches taken and the inherent risks involved.
Recruitment and Retention Initiatives
Hospitals are aggressively pursuing strategies to attract and retain nurses. These initiatives often involve significant financial investments and a shift in organizational culture. Many hospitals are offering competitive salaries and benefits packages, including sign-on bonuses, tuition reimbursement, and flexible scheduling options. Some are also investing in advanced training programs and leadership development opportunities to enhance professional growth and improve job satisfaction.
For example, University Hospital System in a major metropolitan area implemented a comprehensive mentorship program pairing experienced nurses with new hires, resulting in a 15% reduction in new nurse turnover within the first year. Another example includes offering loan forgiveness programs for nurses willing to commit to a certain number of years of service.
Financial Implications of the Nursing Shortage
The financial burden of the nursing shortage is substantial. Increased reliance on expensive temporary staffing agencies to fill vacant positions significantly inflates operational costs. Hospitals are also facing higher overtime expenses due to existing staff working longer hours to compensate for understaffing. The cost of recruitment campaigns, including advertising and travel expenses for candidates, adds further strain to already tight budgets.
For instance, one medium-sized community hospital reported a 20% increase in agency staffing costs within a single year, directly impacting their profitability. This financial strain can lead to reduced investment in other crucial areas, such as equipment upgrades and facility improvements.
Managing Patient Care with Reduced Nursing Staff
The most critical consequence of the nursing shortage is the impact on patient care. Hospitals are forced to implement strategies to manage patient loads with fewer nurses, often resulting in increased workloads and potential compromises in the quality of care. This may involve altering patient assignments, prioritizing urgent cases, and delaying less critical procedures. The risks include increased patient wait times, potential for medical errors due to overworked staff, and compromised patient safety.
For example, some hospitals have implemented “nurse navigators” to help streamline patient flow and ensure efficient allocation of resources. However, this approach, while helpful, cannot fully compensate for the fundamental lack of nursing staff. The potential consequences of inadequate staffing include increased rates of hospital-acquired infections, longer hospital stays, and ultimately, poorer patient outcomes.
Advocacy Groups’ Positions and Proposed Solutions
The nursing shortage is a multifaceted crisis demanding comprehensive solutions. While hospitals grapple with immediate staffing issues, advocacy groups offer crucial perspectives and propose long-term strategies to address the root causes of the problem. Understanding their positions is essential for developing effective policies and fostering a sustainable future for the nursing profession.
Several key nursing advocacy groups are actively working to improve the situation. Their approaches, while sharing some common ground, also highlight differing priorities and proposed solutions. Examining these differences provides a more complete understanding of the challenges and potential pathways forward.
National Nurses United (NNU) Perspectives and Proposed Solutions, Where are all the nurses hospitals advocates disagree on crisis
NNU, the largest union and professional association for registered nurses in the United States, focuses heavily on improving working conditions and advocating for better staffing ratios. They argue that inadequate staffing levels lead to burnout, increased errors, and compromised patient care. Their perspective emphasizes the need for collective bargaining and strong labor protections to empower nurses and improve their working lives.
They believe that improving working conditions will attract and retain nurses, ultimately alleviating the shortage.
American Nurses Association (ANA) Perspectives and Proposed Solutions
The ANA, a professional organization representing registered nurses, takes a broader approach, addressing issues ranging from workforce development to policy advocacy. While also emphasizing safe staffing ratios, the ANA also focuses on improving nurse education, addressing the nursing faculty shortage, and advocating for policies that support nurses’ career development and well-being. Their strategy combines direct advocacy for legislative changes with initiatives aimed at enhancing the profession’s image and attracting new recruits.
AARP Perspectives on Nurses and the Aging Population
AARP, while not solely focused on nursing, recognizes the significant role nurses play in caring for the growing elderly population. Their advocacy centers on ensuring adequate staffing levels in facilities serving older adults, particularly in long-term care settings. They highlight the increasing demand for geriatric nursing expertise and advocate for policies that support the training and retention of nurses specializing in geriatric care.
This perspective underscores the connection between the nursing shortage and the aging population, emphasizing the need for targeted interventions.
Comparison of Proposed Solutions
The proposed solutions from these advocacy groups, while distinct in some aspects, share significant overlap. A comprehensive approach necessitates addressing multiple interconnected issues.
- Improved Staffing Ratios: All three groups advocate for mandated safe staffing ratios, arguing that this is crucial for patient safety and nurse well-being. This often involves lobbying for state and federal legislation to establish minimum nurse-to-patient ratios in various healthcare settings.
- Increased Nurse Education Funding: The ANA and, indirectly, AARP, emphasize the need for increased funding for nursing education, including scholarships, loan forgiveness programs, and support for nursing faculty. This is seen as crucial for expanding the nursing workforce pipeline.
- Addressing Nurse Burnout and Retention: NNU’s focus on collective bargaining and improved working conditions directly addresses nurse burnout and retention. The ANA and AARP support initiatives aimed at improving workplace culture, reducing stress, and promoting work-life balance.
- Targeted Recruitment Campaigns: All groups indirectly support recruitment campaigns aimed at attracting individuals to the nursing profession, especially those from underrepresented groups. These campaigns may focus on highlighting the rewards of the profession and addressing misconceptions about nursing careers.
- Policy Changes to Support Nurses’ Career Development: The ANA specifically advocates for policies that support nurses’ career development, including opportunities for advanced education, leadership roles, and specialized training.
Policy Changes Advocated For
Each group advocates for specific policy changes to improve nurse working conditions and recruitment. These changes are interconnected and crucial for addressing the nursing shortage effectively.
- NNU: Focuses on strengthening labor laws to facilitate collective bargaining, ensuring nurses have a voice in determining their working conditions and advocating for mandated safe staffing ratios through legislation.
- ANA: Advocates for increased funding for nursing education and research, the implementation of safe staffing ratios, and policies that support nurses’ career advancement and professional development.
- AARP: Advocates for policies that support the training and retention of nurses specializing in geriatric care, addressing the increasing demand for geriatric nursing expertise in the context of the aging population and improved staffing in long-term care facilities.
The Role of Education and Training in Addressing the Shortage
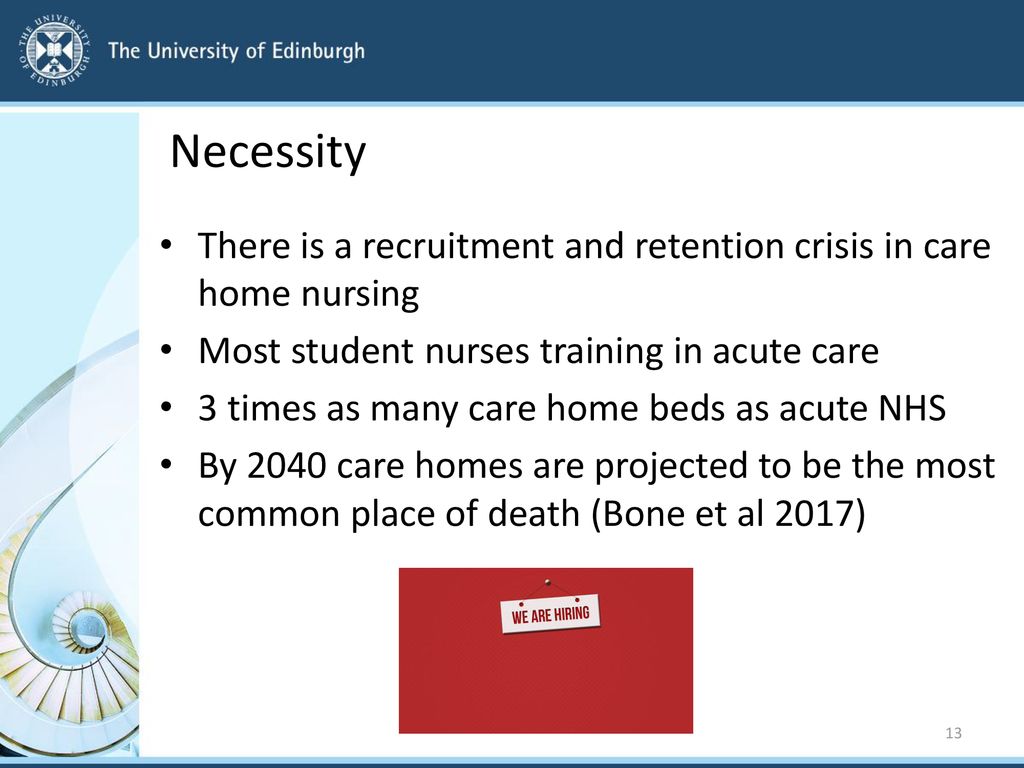
Source: slideplayer.com
The nursing shortage is a complex problem with multifaceted solutions. A critical component, often overlooked amidst discussions of pay and working conditions, is the role of nursing education and training. Improving the pipeline of qualified nurses requires a multi-pronged approach that addresses challenges in both attracting new students and retaining those already in the system.Current nursing education and training programs face significant hurdles.
Many programs are struggling with outdated facilities, limited clinical placement opportunities, and a lack of funding, leading to increased tuition costs and a less-than-ideal learning environment. These factors, coupled with the demanding nature of the profession itself, contribute to a decline in applicants and an increase in attrition rates among students. The perception of nursing as a high-stress, low-reward career further exacerbates the issue.
Challenges in Attracting and Retaining Nursing Students
The challenges in attracting and retaining nursing students are substantial and interconnected. High tuition costs create a significant barrier to entry for many prospective students, particularly those from lower socioeconomic backgrounds. The intense academic rigor and demanding clinical hours often lead to burnout and attrition before graduation. Additionally, a lack of mentorship and support systems within nursing programs can leave students feeling isolated and unsupported.
Finally, the negative perception of the profession—characterized by long hours, high stress levels, and limited work-life balance—discourages many potential candidates from pursuing a career in nursing.
A Hypothetical Program to Increase the Number of Nurses
To effectively address the nursing shortage, a comprehensive program is needed. This program should focus on increased funding for nursing schools, expansion of clinical placement opportunities, and innovative recruitment strategies. Curriculum revisions should prioritize technology integration and simulation training to improve the quality of education and prepare students for the complexities of modern healthcare. Funding could be secured through a combination of government grants, private donations, and partnerships with healthcare organizations.
Recruitment strategies should target diverse populations and highlight the rewarding aspects of the nursing profession, emphasizing career advancement opportunities and work-life balance initiatives. For example, scholarships and loan forgiveness programs could incentivize students from underrepresented groups to pursue nursing careers. Partnerships with hospitals could provide guaranteed employment upon graduation and mentorship opportunities during the clinical experience.
Examples of Innovative Nursing Education Programs
Several innovative programs are already making strides in addressing the nursing shortage. For example, some schools are implementing accelerated nursing programs that allow students to complete their degree in a shorter timeframe, reducing the overall cost and time commitment. Others are incorporating telehealth training into their curriculum, preparing students for the growing demand for remote healthcare services. Simulation-based learning is becoming increasingly common, providing students with realistic clinical experiences in a safe and controlled environment.
These programs, while still requiring increased funding and wider adoption, show promise in attracting and retaining students while preparing them for the realities of modern nursing practice. The University of Pennsylvania’s accelerated BSN program, for example, is known for its high completion rates and strong placement outcomes. Their focus on experiential learning and individualized support is a model for other institutions to emulate.
The Impact on Patient Care and Outcomes
The nursing shortage casts a long shadow over the quality and safety of patient care. Reduced nurse-to-patient ratios, increased workloads, and pervasive burnout among existing staff contribute to a healthcare system struggling to meet the needs of its patients. The consequences are far-reaching, impacting everything from immediate patient safety to long-term health outcomes.The decreased availability of nurses directly affects the quality of care patients receive.
Hospitals facing severe shortages often rely on agency nurses or forced overtime from existing staff, leading to less continuity of care and potentially less experienced personnel caring for patients. This can increase the risk of medical errors, delayed treatment, and a decline in the overall patient experience.
Patient Safety and Quality of Care
Inadequate staffing levels significantly compromise patient safety. For instance, a study published in the American Journal of Nursing found a direct correlation between higher nurse-to-patient ratios and reduced rates of hospital-acquired infections. Conversely, understaffed units are associated with increased medication errors, falls, and pressure ulcers. Patients in understaffed units may experience longer wait times for pain medication, assistance with daily needs, and prompt responses to call bells.
Imagine a scenario where a patient experiences a sudden deterioration in their condition, but the nurse is already overwhelmed with multiple critically ill patients; timely intervention becomes a matter of chance rather than guaranteed care. This scenario highlights the potential for catastrophic outcomes due to inadequate staffing.
Comparison of Patient Experiences
Patients in hospitals with adequate nursing staff generally report higher satisfaction levels and better experiences. They receive more personalized attention, feel more secure and supported, and are more likely to receive timely and effective care. In contrast, patients in understaffed hospitals may feel rushed, neglected, and anxious. They might experience delays in treatment, a lack of responsiveness to their needs, and a general sense of being overwhelmed by the environment.
This difference in experience is not merely anecdotal; studies consistently show a link between nurse staffing levels and patient satisfaction scores. For example, a patient in a well-staffed cardiac unit might receive frequent monitoring and proactive interventions to prevent complications, whereas a patient in an understaffed unit might face delays in receiving essential medications or experiencing inadequate pain management.
The nursing shortage crisis has everyone arguing – hospitals, advocates, and even nurses themselves disagree on the root causes. Understanding the complexities of healthcare data flow is crucial to finding solutions, and that’s where a resource like the podcast inside healthcare apis comes in handy. It sheds light on the technological hurdles impacting efficient staffing and resource allocation, ultimately informing the debate about where all the nurses are and why the system is struggling.
Consequences of Nursing Shortage on Healthcare Outcomes
The nursing shortage has profound consequences for overall healthcare outcomes.
The following points highlight the potential impact:
- Increased hospital readmission rates: Patients discharged from understaffed hospitals may experience a higher risk of complications leading to readmission.
- Longer hospital stays: Inadequate care can delay recovery and prolong the length of hospital stays.
- Higher mortality rates: Studies have linked understaffing to increased mortality rates in certain patient populations.
- Increased healthcare costs: Higher readmission rates and longer hospital stays contribute significantly to increased healthcare costs.
- Increased risk of medical errors: Overworked and stressed nurses are more prone to making mistakes.
- Decreased patient satisfaction: Negative patient experiences can lead to dissatisfaction and complaints.
- Burnout and attrition among nurses: Chronic understaffing contributes to burnout, leading to higher nurse turnover rates and exacerbating the shortage.
The Influence of Healthcare Policy and Funding

Source: yimg.com
The nursing shortage isn’t just a staffing problem; it’s a systemic issue deeply intertwined with healthcare policy and funding decisions. Government policies, reimbursement rates, and overall healthcare spending directly impact the ability of hospitals and healthcare systems to recruit, retain, and adequately compensate nurses. Understanding this complex interplay is crucial to developing effective solutions.Healthcare policies significantly influence the nursing workforce in several ways.
These policies range from regulations governing nursing education and licensing to those impacting hospital reimbursement and staffing ratios.
Key Healthcare Policies Impacting the Nursing Workforce
The Affordable Care Act (ACA), for example, expanded health insurance coverage, leading to increased demand for healthcare services and, consequently, nurses. However, the ACA’s impact on nurse supply has been complex, with some arguing it hasn’t adequately addressed the underlying shortage. Conversely, policies that restrict immigration or limit the number of international nurses allowed to practice in a country can directly constrain the available nursing workforce.
Similarly, policies affecting the scope of practice for nurses, such as allowing nurse practitioners greater autonomy, can impact both the supply and distribution of nursing care. Finally, mandates regarding nurse-to-patient ratios, while aiming to improve patient safety, can place significant financial strain on healthcare providers, potentially hindering recruitment and retention efforts.
The Role of Healthcare Funding in Addressing the Nursing Shortage
Healthcare funding is the lifeblood of the nursing workforce. Insufficient funding directly translates to lower salaries, fewer benefits, and reduced opportunities for professional development, making nursing less attractive to potential recruits and increasing burnout among existing nurses. Conversely, increased funding can allow for higher salaries, better benefits packages, and improved working conditions, thus enhancing recruitment and retention. Funding decisions also influence the capacity of nursing schools to expand their programs and increase the number of graduates entering the workforce.
The nursing shortage crisis has everyone shouting – hospitals, advocates, and nurses themselves are all pointing fingers. It’s a complex issue, and finding solutions requires understanding the bigger picture. This brings to mind the recent appointment of Brian Setzer as executive vice president of Walmart Health, walmart health new executive vice president brian setzer , a move that could significantly impact healthcare access and potentially influence the ongoing debate about where all those nurses are and how to address the crisis effectively.
Ultimately, fixing the crisis needs a multi-pronged approach that considers all aspects of the healthcare system.
For instance, increased funding for nursing scholarships and loan forgiveness programs can incentivize individuals to pursue nursing careers.
Potential Benefits and Drawbacks of Different Healthcare Funding Models
Different healthcare funding models have varying impacts on nurse staffing levels. A single-payer system, for example, could potentially provide more consistent and predictable funding for healthcare, potentially leading to better nurse salaries and improved working conditions. However, a single-payer system might also face challenges in controlling costs, potentially limiting the overall amount of funding available for healthcare. Alternatively, a market-based system, while potentially incentivizing efficiency and competition, could lead to disparities in nurse staffing levels and compensation depending on market forces and the financial viability of different healthcare providers.
For instance, hospitals in underserved rural areas may struggle to attract and retain nurses due to lower reimbursement rates compared to urban areas in a market-based system. A well-designed hybrid system might aim to balance the advantages of both models, offering some level of universal access while still allowing for market-based incentives to improve efficiency and quality of care.
The optimal model is likely context-specific and requires careful consideration of the specific healthcare landscape.
Visual Representation of Key Data
Data visualization is crucial for understanding the complex issue of nursing shortages. By presenting the information visually, we can readily grasp the scope and geographic distribution of the problem, as well as compare nurse-to-patient ratios across different healthcare systems. This allows for a more effective identification of areas needing immediate attention and the development of targeted solutions.
Geographic Distribution of Nursing Shortages
A choropleth map would effectively illustrate the geographic distribution of nursing shortages across the country. The map would use a color scale to represent the severity of the shortage in each state. For example, states with the most severe shortages could be depicted in dark red, while those with less severe shortages would be shown in lighter shades of red, progressing to yellow and then green for states with adequate staffing.
A legend would clearly define the color scale, providing specific numerical ranges (e.g., Dark Red: > 20% shortage, Red: 10-20% shortage, Yellow: 5-10% shortage, Green: <5% shortage). The map would utilize state boundaries for clear demarcation and potentially include county-level data for a more granular view if available. This visual would instantly highlight areas experiencing the most significant challenges.
Nurse-to-Patient Ratios Across Different Hospital Systems
A bar chart would effectively compare nurse-to-patient ratios across various hospital systems. The horizontal axis (x-axis) would list the names of different hospital systems (e.g., System A, System B, System C).
The vertical axis (y-axis) would represent the nurse-to-patient ratio, with the scale clearly labeled (e.g., 1:4, 1:5, 1:6, etc., indicating one nurse for every four, five, or six patients). Each bar would represent a specific hospital system, with its height corresponding to its nurse-to-patient ratio. Data labels would be placed on top of each bar, clearly indicating the exact ratio for each system.
This allows for immediate comparison and highlights disparities in staffing levels across different healthcare providers. For example, a bar significantly shorter than others would immediately indicate a system with a lower nurse-to-patient ratio and therefore potentially a higher patient-to-nurse burden.
Final Review
The nursing shortage is a complex issue with no easy fixes. While hospitals scramble to implement short-term solutions, the long-term answer lies in a multi-pronged approach. We need to invest heavily in nursing education, create more supportive work environments, and advocate for policies that value and protect nurses. The consequences of inaction are far-reaching – impacting patient safety, healthcare costs, and the overall well-being of our communities.
It’s time to listen to the voices of nurses, hospitals, and advocates and work together to find a sustainable solution to this critical crisis.
FAQ Guide
What are the most common reasons nurses leave their jobs?
Burnout, inadequate staffing levels, lack of support from management, and low pay are frequently cited reasons.
How does the nursing shortage affect patient outcomes?
It can lead to increased medical errors, longer wait times, and decreased patient satisfaction.
Are there any innovative solutions being implemented to address the shortage?
Yes, some hospitals are exploring telehealth, using technology to improve efficiency, and offering flexible work arrangements to attract and retain nurses.
What role does the government play in addressing the nursing shortage?
Government funding for nursing education, loan forgiveness programs, and policies to improve working conditions all play a significant role.


