Tenet Detroit Medical Center Vanguard False Claims Act Settlement
Tenet Detroit Medical Center Vanguard False Claims Act settlement – the words alone sound serious, right? But this massive legal battle isn’t just about numbers; it’s a story about alleged wrongdoing, government investigations, and the ultimate impact on patient care and the healthcare industry as a whole. This settlement involves millions of dollars and raises critical questions about accountability and ethical practices within major medical systems.
We’ll dive into the details, exploring the accusations, the settlement terms, and what this all means for the future.
This post will break down the complexities of the case, examining the allegations of false claims, the government’s involvement, and the lasting effects on Tenet Detroit Medical Center Vanguard. We’ll also explore broader implications for the healthcare industry and offer some food for thought on preventing similar situations in the future. Get ready for a deep dive into this fascinating (and somewhat unsettling) case study.
Overview of the Tenet Detroit Medical Center Vanguard False Claims Act Settlement
The Tenet Detroit Medical Center (DMC) Vanguard False Claims Act settlement involved a significant legal battle concerning allegations of fraudulent billing practices. This settlement, reached after years of investigation and litigation, highlights the complexities and high stakes involved in healthcare fraud cases and the government’s commitment to pursuing accountability. The case serves as a cautionary tale for healthcare providers regarding the importance of accurate billing and compliance with federal regulations.The settlement involved Tenet Healthcare Corporation, the parent company of the DMC, and the United States government, represented by the Department of Justice.
The allegations centered around fraudulent billing practices at DMC’s Vanguard Health Systems, specifically related to the improper billing of Medicare and Medicaid for services provided. The government alleged that Vanguard submitted false claims for reimbursement, inflating the costs of services or billing for services that were not medically necessary or were not actually provided. This involved various billing schemes and practices.
Timeline of Events
The timeline of events leading to the settlement likely spanned several years. It began with an initial investigation, possibly triggered by a whistleblower complaint or internal audit findings. This would have involved the government reviewing medical records, billing documents, and conducting interviews with employees and patients. Subsequently, the government likely issued a subpoena to obtain additional information and evidence, building a case against Tenet.
Negotiations between Tenet and the Department of Justice would have ensued, possibly involving multiple rounds of discussions and offers, before a final settlement agreement was reached. The specific dates of these events are not publicly available in detail but are generally spread across several years.
Key Terms and Conditions of the Settlement Agreement
The settlement agreement likely involved a substantial financial payment from Tenet to the government. This payment would represent a compromise, with the amount reflecting the government’s assessment of the damages caused by the fraudulent billing practices. The settlement agreement would have also included provisions related to corporate integrity obligations. This often means Tenet agreed to implement robust compliance programs to prevent future violations.
These programs might involve regular audits, employee training, and enhanced oversight of billing practices. Importantly, the settlement would have likely included a clause stating that the payment does not constitute an admission of liability by Tenet. While Tenet agreed to pay, they did not explicitly admit to the allegations of fraud. The precise details of the financial terms and the corporate integrity obligations would likely be confidential, sealed under the terms of the agreement.
Allegations of False Claims
The Tenet Detroit Medical Center Vanguard False Claims Act settlement stemmed from serious allegations of fraudulent billing practices. The lawsuit claimed that Tenet knowingly submitted false claims to Medicare and Medicaid, violating the False Claims Act. These allegations involved a complex web of deceptive actions designed to maximize reimbursement, ultimately costing taxpayers millions.The core of the allegations centered on the intentional misrepresentation of patient diagnoses and the provision of unnecessary services.
This wasn’t a case of isolated incidents; the lawsuit painted a picture of a systemic problem deeply ingrained within the hospital’s operations. The government argued that this wasn’t accidental overbilling, but rather a deliberate scheme to defraud the healthcare system.
Specific Allegations of Fraudulent Billing
The lawsuit detailed several specific types of fraudulent activities. These included upcoding, where less expensive procedures were billed as more expensive ones, resulting in inflated payments. Another key allegation involved unbundling, where multiple services were billed separately, even though they were part of a single procedure. This practice artificially inflated the total cost of care. Additionally, the lawsuit alleged that medically unnecessary services were provided solely to increase revenue.
The government argued that this wasn’t simply a matter of billing errors, but rather a deliberate strategy to maximize profits at the expense of taxpayers.
Evidence Presented in Support of Allegations
The evidence presented in support of these allegations likely included a range of documentation. This could have encompassed internal hospital records such as billing records, patient charts, physician notes, and emails between staff. Whistleblower testimony, offering firsthand accounts of the alleged fraudulent practices, may have also played a significant role. Statistical analyses comparing Tenet’s billing practices to those of comparable hospitals might have been used to highlight unusual patterns and support claims of systematic fraud.
Government investigators likely conducted extensive audits of patient records and billing data to identify specific instances of upcoding, unbundling, and provision of unnecessary services. The strength of the evidence presented, along with the substantial settlement amount, suggests a compelling case was made against Tenet.
Government’s Role in the Investigation and Settlement
Source: phillipsandcohen.com
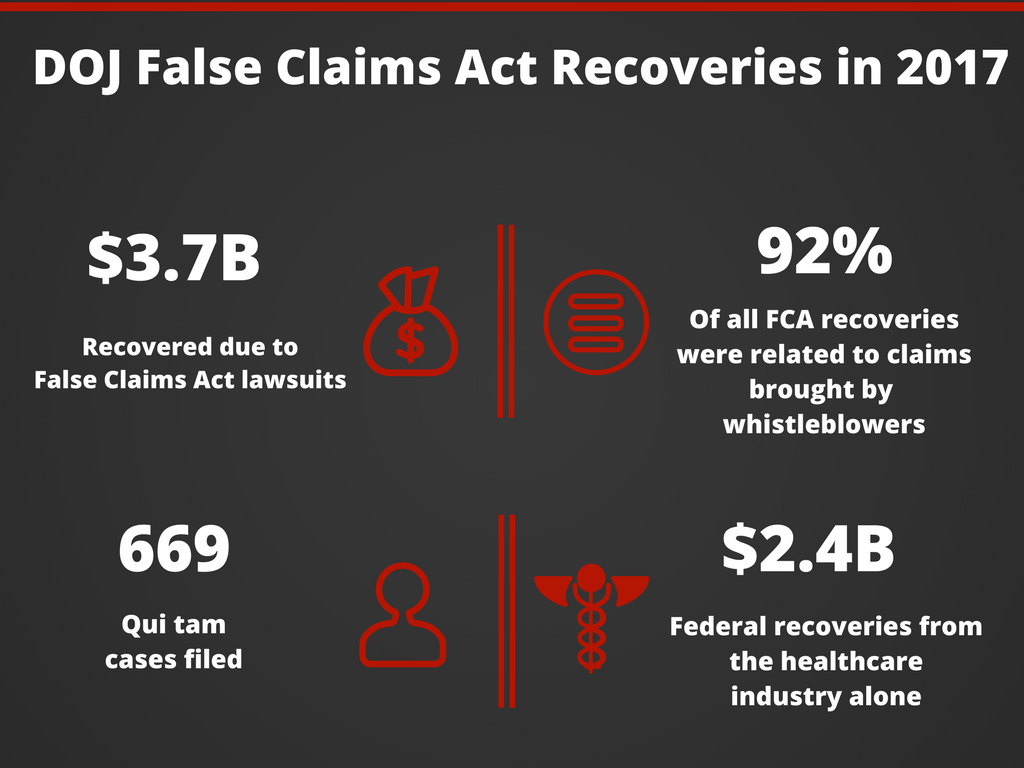
The Department of Justice (DOJ), specifically the Civil Division’s Fraud Section, played a central role in investigating and resolving the Tenet Detroit Medical Center Vanguard False Claims Act settlement. Their investigation likely involved a complex interplay of legal processes and collaborative efforts with other government agencies. Understanding their actions provides insight into the mechanics of False Claims Act litigation.The DOJ’s investigation likely began with a whistleblower’s complaint, which initiated a thorough examination of Tenet’s billing practices at the Vanguard facility.
This would have involved reviewing medical records, financial documents, and conducting interviews with employees and potentially patients. Other agencies, such as the Centers for Medicare & Medicaid Services (CMS), may have contributed expertise in healthcare billing regulations and compliance. The investigation’s scope would have been extensive, aiming to establish a clear picture of whether Tenet knowingly submitted false claims for reimbursement.
DOJ Investigative Methods and Legal Processes
The DOJ utilizes various investigative techniques in False Claims Act cases. These can include subpoenaing documents, conducting on-site inspections, and interviewing witnesses under oath. The legal process itself follows a defined path. Once sufficient evidence is gathered suggesting violations of the False Claims Act, the DOJ can file a lawsuit against the defendant (Tenet, in this case).
This lawsuit would detail the alleged fraudulent activities and seek monetary penalties and other remedies. The defendant can then choose to fight the allegations in court or negotiate a settlement. The process can involve extensive discovery, where both sides exchange evidence and information, and potentially pre-trial motions addressing legal issues.
Rationale for Settlement
The decision by the government to settle the case rather than proceed to trial likely involved a cost-benefit analysis. Litigating False Claims Act cases can be lengthy and expensive. Settling allows the government to recover funds relatively quickly and avoid the uncertainties of a trial. A settlement also acknowledges the government’s belief that there was sufficient evidence to support the allegations, even if it avoids the complexities and expense of a full trial.
The Tenet Detroit Medical Center Vanguard False Claims Act settlement highlights the ongoing challenges in healthcare billing accuracy. This makes advancements like those described in this article, nuance integrates generative ai scribe epic ehrs , even more critical. Improved EHR integration and AI-powered documentation could help prevent future billing errors and reduce the risk of similar costly settlements.
Ultimately, focusing on accurate documentation is key to avoiding these kinds of legal battles.
The amount of the settlement reflects the government’s assessment of Tenet’s liability and the seriousness of the alleged misconduct. This is a common practice in complex civil litigation, where both sides often prefer a negotiated resolution to the risks and unpredictability of a jury trial.
Impact of the Settlement on Tenet Detroit Medical Center Vanguard
The Tenet Detroit Medical Center Vanguard False Claims Act settlement carried significant consequences for the healthcare provider, impacting its finances, reputation, and operational practices. The settlement’s ramifications extended beyond the immediate financial penalty, influencing long-term strategic decisions and the organization’s overall standing within the healthcare community.The financial implications of the settlement were substantial. While the exact figure isn’t publicly available in every detail, the settlement likely involved a considerable payout to the government, encompassing penalties, damages, and potentially legal fees.
This significant financial burden could affect Tenet Detroit Medical Center Vanguard’s profitability, investment capacity, and ability to fund future projects or expansions. Such a large financial outlay could also impact its credit rating and borrowing capacity, making future financing more expensive or difficult to obtain. Similar settlements in the healthcare industry have shown that even large organizations can experience a temporary downturn in financial performance following such legal actions.
For example, a comparable settlement involving another large hospital system resulted in a reduction of their quarterly earnings by a significant percentage.
Financial Implications of the Settlement
The settlement’s financial impact on Tenet Detroit Medical Center Vanguard is multifaceted. Direct costs include the settlement payment itself, along with legal fees incurred during the investigation and litigation. Indirect costs might include lost revenue stemming from potential negative publicity and reduced patient confidence. The long-term financial impact will depend on Tenet’s ability to manage its expenses, maintain patient volume, and avoid future legal issues.
Financial analysts would likely scrutinize the company’s financial statements and projections to assess the long-term effect on its financial health. Furthermore, the settlement could influence investor confidence, leading to potential fluctuations in the company’s stock price (assuming it’s publicly traded).
Reputational Damage from the Settlement, Tenet Detroit Medical Center Vanguard False Claims Act settlement
The settlement undoubtedly caused reputational damage to Tenet Detroit Medical Center Vanguard. Negative media coverage surrounding allegations of fraudulent billing practices can erode public trust and damage the organization’s image. Potential patients might hesitate to seek care at a facility associated with such allegations, leading to a decline in patient volume and revenue. The reputational harm extends beyond the immediate aftermath of the settlement, potentially impacting future partnerships, collaborations, and the organization’s ability to attract and retain skilled healthcare professionals.
The long-term impact on the organization’s reputation will depend on its ability to effectively communicate its commitment to ethical practices and transparency.
Changes Implemented to Prevent Future Violations
To mitigate the risk of future violations and rebuild trust, Tenet Detroit Medical Center Vanguard likely implemented several changes in its billing and compliance practices. These changes are crucial not only for avoiding further legal action but also for maintaining ethical standards within the healthcare system. The following table Artikels a comparison of pre- and post-settlement practices. Note that specific details of post-settlement changes are often not publicly released for competitive and strategic reasons.
| Area | Pre-Settlement Practice | Post-Settlement Practice | Impact |
|---|---|---|---|
| Billing and Coding | Potentially inconsistent or inaccurate coding practices leading to overbilling. | Implementation of stricter coding protocols, enhanced training for billing staff, and more rigorous internal audits. | Reduced risk of future billing errors and fraudulent claims. Improved accuracy and compliance. |
| Compliance Program | Possibly inadequate compliance program with limited oversight and monitoring. | Strengthened compliance program with increased oversight, regular audits, and a more robust system for reporting and investigating potential violations. | Enhanced detection and prevention of non-compliance. Increased accountability and transparency. |
| Employee Training | Limited or insufficient training on billing regulations and compliance requirements. | Comprehensive training programs for all staff involved in billing and coding, with regular updates on regulatory changes. | Improved understanding of compliance requirements and reduced risk of unintentional errors. |
| Internal Controls | Potentially weak internal controls allowing for undetected errors or fraudulent activities. | Implementation of enhanced internal controls, including improved oversight of billing processes and more rigorous checks and balances. | Increased detection and prevention of errors and fraud. Strengthened financial integrity. |
Implications for the Healthcare Industry

Source: fcacounsel.com
The Tenet Detroit Medical Center Vanguard False Claims Act settlement carries significant implications for the entire healthcare industry, serving as a stark reminder of the potential legal and financial consequences of billing practices that deviate from established guidelines. This case highlights the increasing scrutiny of healthcare providers’ billing and coding practices by both the government and private payers, emphasizing the need for robust compliance programs and a culture of ethical conduct.
The substantial financial penalty levied against Tenet underscores the seriousness with which such violations are treated.The settlement’s impact extends beyond the immediate financial repercussions for Tenet. It sends a clear message to other healthcare providers about the importance of accurate billing and documentation. This case, along with others like it, influences future regulatory actions and encourages a more cautious approach to billing and coding practices across the industry.
The Tenet Detroit Medical Center Vanguard False Claims Act settlement highlights the critical need for improved healthcare transparency and accountability. This makes me wonder how advancements like those explored in a recent study, study widespread digital twins healthcare , could help prevent similar situations. Perhaps widespread adoption of digital twins could offer a more proactive approach to fraud detection and patient care optimization, ultimately impacting future settlements like the Tenet case.
The precedent set by this settlement could lead to increased audits and investigations, prompting a broader reevaluation of compliance protocols within healthcare organizations.
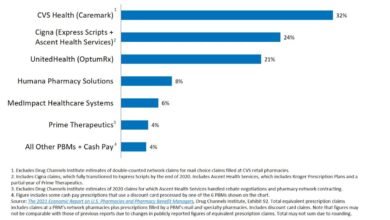
Comparison to Similar Settlements
Several other significant False Claims Act settlements in the healthcare sector share similarities with the Tenet case. For instance, the massive settlements involving pharmaceutical companies for off-label marketing or hospitals for improper billing of Medicare and Medicaid services illustrate the pervasiveness of such issues. These cases, like the Tenet settlement, underscore the high stakes involved in healthcare billing compliance and the government’s unwavering commitment to pursuing fraudulent activities.
The sheer size of many of these settlements, often running into hundreds of millions of dollars, demonstrates the potential for catastrophic financial losses and reputational damage. These settlements frequently involve allegations of upcoding, unbundling, and other fraudulent billing practices, mirroring the accusations in the Tenet case. The common thread is a failure to maintain rigorous compliance programs and adequately train staff on appropriate billing procedures.
Recommendations for Healthcare Providers
The Tenet case provides valuable lessons for healthcare providers seeking to avoid similar legal entanglements. Implementing a comprehensive compliance program is paramount. This program should include, but not be limited to, the following key elements:
A robust compliance program is essential for avoiding legal issues. This goes beyond simply having a written policy; it requires active implementation and ongoing monitoring.
- Regular Training and Education: All staff involved in billing and coding should receive regular, comprehensive training on relevant regulations and best practices. This training should be updated to reflect changes in legislation and industry standards.
- Strong Internal Controls: Implement rigorous internal controls to monitor billing and coding practices, identify potential errors, and ensure adherence to regulatory requirements. This includes regular audits and reviews of billing data.
- Effective Documentation: Maintain detailed and accurate medical records to support all billing claims. Documentation should be clear, concise, and readily auditable.
- Compliance Officer: Appoint a dedicated compliance officer responsible for overseeing the compliance program and ensuring its effectiveness. This individual should have the authority to investigate potential violations and implement corrective actions.
- Regular Audits and Self-Disclosure: Conduct regular internal audits to identify and address potential compliance issues proactively. Establish a process for self-disclosure of any identified violations to regulatory agencies.
- Open Communication: Foster a culture of open communication and transparency where employees feel comfortable reporting potential compliance concerns without fear of retaliation.
Public Perception and Media Coverage: Tenet Detroit Medical Center Vanguard False Claims Act Settlement
The Tenet Detroit Medical Center Vanguard False Claims Act settlement generated significant public attention and media coverage, sparking discussions about healthcare ethics, corporate accountability, and the effectiveness of government oversight. The reaction was largely a mixture of outrage from those who felt Tenet had exploited the system, and a degree of skepticism regarding the adequacy of the settlement amount.
The media played a crucial role in shaping public perception, influencing the narrative around the case and its implications.The media’s portrayal of the events varied, with some outlets focusing on the alleged fraudulent activities and the potential harm to patients, while others highlighted Tenet’s attempts to cooperate with the investigation and the company’s subsequent efforts to improve its compliance practices.
The portrayal of Tenet itself ranged from that of a callous corporate entity prioritizing profit over patient care to a company that made mistakes but ultimately took responsibility. The government’s role was generally depicted as a necessary check on corporate power, though some questioned whether the settlement was a sufficient deterrent to future wrongdoing.
Media Portrayal of Involved Parties
The media’s depiction of Tenet Healthcare, the Detroit Medical Center, and the government significantly influenced public perception. Tenet was frequently portrayed as the central actor, facing criticism for its alleged fraudulent billing practices. The Detroit Medical Center, as a subsidiary involved in the alleged scheme, also received negative attention. Conversely, the government, represented by the Department of Justice, was often portrayed as the entity holding Tenet accountable and protecting taxpayer interests.
The framing of these parties varied across different news outlets, with some emphasizing the severity of the alleged wrongdoing and others highlighting the settlement as a resolution and a step towards reform.
The Tenet Detroit Medical Center Vanguard False Claims Act settlement highlights the complexities of healthcare billing. This makes me wonder about the financial pressures on smaller facilities, especially considering the challenges faced by rural hospitals, as detailed in this insightful article on Rural Hospitals Labor Delivery & The article’s focus on labor and delivery services brings into sharp relief how financial strains can impact patient care, mirroring some of the issues involved in the Tenet settlement.
Timeline of Significant Media Reports and Public Statements
A detailed timeline of significant media coverage and public statements would provide a clearer picture of how public perception evolved throughout the settlement process. For example, an early report might have focused on the initial allegations, followed by later reports detailing the government’s investigation, the settlement announcement, and subsequent analysis of the settlement’s impact. Statements from Tenet, the Department of Justice, and patient advocacy groups would also provide crucial context.
Such a timeline would illustrate the progression of the story in the public eye and demonstrate how media narratives shaped public opinion. While a comprehensive timeline requires access to a detailed archive of news reports and public statements, a simplified version might include the date of the initial allegations, the date the lawsuit was filed, the date of the settlement announcement, and the dates of significant media articles or press releases from involved parties.
Legal and Ethical Considerations
The Tenet Detroit Medical Center Vanguard False Claims Act settlement highlights the complex interplay of legal and ethical considerations within the healthcare industry. Violations of the False Claims Act carry significant consequences, impacting not only the offending organizations but also the individuals involved. Understanding these ramifications is crucial for maintaining ethical practices and ensuring patient well-being.The False Claims Act prohibits knowingly submitting false or fraudulent claims to the government for payment.
In the healthcare context, this encompasses a wide range of actions, from billing for services not rendered to upcoding (billing for a more expensive service than the one provided) and submitting claims based on falsified medical records. Ethical breaches often underpin these legal violations, demonstrating a disregard for patient care and the public trust.
Consequences for Individuals and Organizations
Individuals involved in False Claims Act violations face severe penalties, including substantial fines, imprisonment, and exclusion from participation in federal healthcare programs. Organizations, on the other hand, can face massive financial penalties, reputational damage, and legal repercussions that can cripple their operations. The settlement with Tenet demonstrates the significant financial burden that can result from such violations – millions of dollars in fines and restitution are common in these cases.
For example, the pharmaceutical company Pfizer faced a multi-billion dollar fine for various violations of the False Claims Act. This showcases the substantial financial risk associated with non-compliance. The reputational damage can be equally devastating, impacting patient trust and potentially leading to a loss of business.
Government and Tenet’s Legal Strategies
The government typically employs a rigorous investigative approach, utilizing resources such as whistleblowers, audits, and data analysis to identify potential violations. In the Tenet case, the government likely used a combination of these methods to build its case. Their legal strategy would have focused on proving that Tenet knowingly submitted false claims, aiming to secure a substantial settlement or a court judgment.
Tenet’s legal strategy, conversely, would have likely centered on challenging the government’s evidence, negotiating a settlement to minimize financial penalties, and potentially arguing for mitigating circumstances. This often involves a complex process of legal maneuvering and negotiations, highlighting the high stakes involved in these types of cases. The ultimate outcome reflects a balance of the government’s investigative strength and Tenet’s legal defense.
Ethical Dimensions of Healthcare Fraud
Beyond the legal ramifications, the ethical implications of healthcare fraud are profound. Submitting false claims erodes public trust in the healthcare system, potentially harming vulnerable populations who rely on government programs for access to care. The prioritization of profit over patient well-being is a significant ethical concern. Actions such as upcoding or billing for unnecessary procedures not only defraud the government but also directly impact patients through increased costs and potentially compromised care.
The ethical responsibility of healthcare providers extends beyond financial gain to upholding the highest standards of patient care and integrity.
Final Thoughts
Source: bipc.com
The Tenet Detroit Medical Center Vanguard False Claims Act settlement serves as a stark reminder of the importance of ethical practices and transparency within the healthcare system. While the financial repercussions are significant, the true cost lies in the potential erosion of public trust. This case highlights the critical role of government oversight and the need for healthcare providers to prioritize patient well-being above all else.
Let’s hope this settlement leads to meaningful reforms and a stronger commitment to ethical conduct across the board.
Questions Often Asked
What is the False Claims Act?
The False Claims Act allows the government to recover money from individuals or companies who defraud government healthcare programs like Medicare and Medicaid.
Who were the whistleblowers in this case?
The identities of the whistleblowers are often kept confidential to protect them from retaliation. Information about them is typically not publicly released.
What specific changes did Tenet implement after the settlement?
Specific details about internal changes implemented by Tenet are usually not made public as part of the settlement agreement. However, it’s likely they involved enhanced compliance programs and internal audits.
Could Tenet face further legal action related to this?
While this settlement resolves the specific claims, it doesn’t preclude the possibility of future legal action if new evidence emerges or other related issues arise.