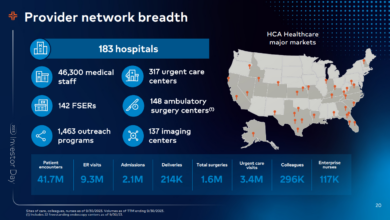
Protect Revenues, Enhance Patient Satisfaction, Improve Access to Care
Protect revenues enhance patient satisfaction and improve access to care w – Protect revenues, enhance patient satisfaction, and improve access to care: it sounds like a juggling act, right? But the truth is, these three goals are incredibly interconnected. Improving one area often has a ripple effect on the others. Think about it: happy patients are more likely to return, leading to better revenue. And easier access to care means more people can get the help they need, leading to both better health outcomes and a more financially stable practice.
This post dives into practical strategies to make this ambitious trifecta a reality.
We’ll explore proven methods for optimizing pricing, implementing effective revenue cycle management, and boosting patient engagement. We’ll also tackle the challenges of improving access, especially for underserved communities, and discuss how to balance financial sustainability with ethical considerations. Get ready to learn how to build a thriving practice that prioritizes both patient well-being and financial health!
Protecting Revenues

Source: pinimg.com
Maintaining financial stability in healthcare is crucial for providing quality care. Optimizing pricing models, implementing effective revenue cycle management, and diversifying revenue streams are key strategies to ensure long-term sustainability while prioritizing patient access. This involves a delicate balance between profitability and accessibility, requiring a strategic and multifaceted approach.
Optimizing Pricing Models for Financial Stability and Accessibility
Effective pricing models must balance the need for financial stability with the imperative of maintaining accessibility for all patients. This requires a nuanced understanding of both the cost of care and the patient’s ability to pay. Strategies include tiered pricing based on income levels, negotiating favorable contracts with insurance providers, and implementing transparent pricing structures to foster trust and understanding.
Analyzing payer mix and adjusting pricing to reflect the reimbursement rates of different payers is also vital. For example, a hospital might offer a sliding scale discount for uninsured patients based on their income, while simultaneously negotiating higher reimbursement rates with major insurance companies for specific high-demand procedures.
The Impact of Preventative Care Programs on Reducing Long-Term Healthcare Costs
Preventative care significantly reduces long-term healthcare costs by preventing costly hospitalizations and chronic disease management. Investing in programs such as annual check-ups, vaccinations, and screenings for common diseases like cancer and heart disease leads to early detection and intervention, minimizing the need for expensive treatments later on. For instance, a comprehensive diabetes prevention program can reduce the incidence of type 2 diabetes, thus lowering the long-term costs associated with managing the disease, including medication, hospital stays, and complications.
The return on investment in preventative care is substantial, both in terms of cost savings and improved patient outcomes.
Successful Revenue Cycle Management Systems and Their Implementation
Efficient revenue cycle management (RCM) systems are essential for optimizing revenue collection and minimizing financial losses. These systems streamline the entire billing process, from patient registration and insurance verification to claims submission and payment collection. Successful implementations involve integrating electronic health records (EHRs) with billing systems, automating claims processing, and employing robust analytics to identify and address billing errors and delays.
For example, a hospital implementing a cloud-based RCM system saw a 15% reduction in days in accounts receivable and a 5% increase in overall revenue collection within six months. This improvement resulted from streamlined workflows, automated claims submission, and improved data analytics.
Revenue Diversification Strategies
The following table compares different revenue diversification strategies:
| Strategy | Description | Advantages | Disadvantages |
|---|---|---|---|
| Telehealth | Providing virtual healthcare services. | Increased accessibility, reduced overhead costs, expanded reach. | Requires technological infrastructure, potential for technical issues, regulatory complexities. |
| Value-Based Care | Focusing on quality outcomes rather than volume of services. | Improved patient outcomes, potential for higher reimbursement, enhanced provider satisfaction. | Requires robust data analytics, potential for financial risk, requires strong provider collaboration. |
| Outpatient Services | Expanding outpatient clinics and services. | Increased revenue streams, reduced hospital inpatient costs, improved patient convenience. | Requires significant investment in facilities and equipment, potential for competition. |
| Retail Clinics | Establishing clinics in convenient locations like pharmacies or retail stores. | Increased accessibility, convenience for patients, potential for higher patient volume. | Limited scope of services, potential for lower reimbursement rates, competition from other retail clinics. |
Enhancing Patient Satisfaction: Protect Revenues Enhance Patient Satisfaction And Improve Access To Care W
Improving patient satisfaction is crucial for any healthcare provider. It’s not just about happy patients; it directly impacts loyalty, positive word-of-mouth referrals, and ultimately, the financial health of the organization. A satisfied patient is more likely to follow treatment plans, adhere to medication schedules, and return for future care. This section will explore practical strategies to enhance patient satisfaction across the entire care journey.
Improving Patient Communication and Engagement
Effective communication is the cornerstone of a positive patient experience. This goes beyond simply providing information; it’s about actively listening, understanding individual needs, and ensuring patients feel heard and respected. Clear, concise explanations of diagnoses, treatment plans, and potential risks are essential. Using plain language, avoiding medical jargon, and checking for understanding are key components. Furthermore, providing patients with multiple communication channels, such as phone calls, email, secure messaging portals, and even video conferencing, empowers them to choose the method that best suits their preferences and needs.
This proactive approach to communication fosters a sense of partnership and trust between the patient and the healthcare team. For example, a hospital implementing a patient portal that allows for secure messaging with their physicians and access to lab results significantly improves communication and patient engagement.
Creating a Positive and Supportive Healthcare Environment
The physical environment plays a significant role in patient satisfaction. A clean, comfortable, and aesthetically pleasing space can significantly reduce patient anxiety and improve their overall experience. Consider factors such as comfortable waiting areas, adequate lighting, noise levels, and the availability of amenities like Wi-Fi. Beyond the physical aspects, fostering a culture of empathy and respect among staff members is equally important.
Staff who are friendly, approachable, and responsive to patient needs create a welcoming and supportive atmosphere. For instance, a clinic with a dedicated play area for children waiting for appointments creates a more relaxed and positive environment for families. Similarly, a hospital implementing a calming music program in waiting areas can help reduce patient anxiety.
Protecting revenues, enhancing patient satisfaction, and improving access to care are all interconnected goals. A recent study, which you can check out here: study widespread digital twins healthcare , suggests that widespread adoption of digital twins could significantly impact these areas. By creating more efficient and personalized care models, we can ultimately achieve better outcomes for both patients and providers, strengthening the financial health of the system while simultaneously improving the patient experience.
Utilizing Patient Feedback Mechanisms
Regularly soliciting and acting upon patient feedback is essential for continuous improvement. Implementing structured feedback mechanisms, such as surveys, comment cards, and suggestion boxes, provides valuable insights into areas where the healthcare organization excels and where improvements are needed. This feedback should be actively analyzed and used to inform changes in processes, policies, and staff training. For example, a consistently negative comment about long wait times can prompt the clinic to re-evaluate its scheduling system or staffing levels.
Open communication channels for addressing concerns and complaints are also critical to showing patients that their feedback is valued.
Designing a Patient Satisfaction Survey
A well-designed patient satisfaction survey is a powerful tool for gathering valuable data. The survey should focus on key aspects of the patient experience, including: ease of scheduling appointments, wait times, communication with staff, clarity of explanations, treatment effectiveness, and overall satisfaction. Using a combination of rating scales (e.g., Likert scales) and open-ended questions allows for both quantitative and qualitative data collection.
A sample question could be: “On a scale of 1 to 5, with 1 being very dissatisfied and 5 being very satisfied, how satisfied were you with the communication you received from your doctor?” Another question could be: “Is there anything else you would like to share about your experience?” Analyzing the results allows for the identification of specific areas for improvement, leading to targeted interventions to enhance patient satisfaction.
Improving Access to Care

Source: twentyoverten.com
Improving access to healthcare is crucial for ensuring a healthy population. Numerous barriers prevent individuals and communities from receiving the care they need, leading to poorer health outcomes and increased healthcare disparities. Addressing these barriers requires a multi-faceted approach encompassing innovative solutions, community engagement, and policy changes.Access to healthcare is not simply about having a hospital nearby; it’s about affordability, convenience, and culturally competent care.
This section will explore the key barriers to accessing healthcare services, effective strategies to overcome them, and successful models for delivering care to underserved populations.
Barriers to Healthcare Access and Proposed Solutions
Many factors contribute to limited healthcare access. Financial constraints are a major obstacle, with high costs of insurance premiums, deductibles, and co-pays preventing many from seeking necessary care. Geographic location also plays a significant role, particularly in rural and underserved areas where healthcare facilities are scarce. Lack of transportation, language barriers, and cultural differences further complicate access.
Protecting revenues, enhancing patient satisfaction, and improving access to care are crucial for any healthcare provider. A key area impacting these goals, especially in underserved communities, is the availability of vital services like labor and delivery. Understanding the challenges faced by rural hospitals in this regard is essential, as highlighted in this insightful article on Rural Hospitals Labor Delivery &.
Ultimately, addressing these challenges directly contributes to a healthier financial picture and better patient outcomes, solidifying our commitment to protect revenues, enhance patient satisfaction, and improve access to care.
A shortage of healthcare professionals, particularly in specialized areas, also contributes to long wait times and limited availability of services.To overcome these barriers, several solutions are necessary. Expanding access to affordable health insurance, such as through government subsidies or employer-sponsored programs, is critical. Investing in telehealth infrastructure and expanding mobile health clinics can extend healthcare services to remote areas.
Implementing multilingual services and culturally sensitive programs can improve access for diverse populations. Furthermore, increasing funding for medical education and training programs can help address the shortage of healthcare professionals. Finally, simplifying the appointment scheduling process and improving communication with patients can make the system more user-friendly and accessible.
Examples of Successful Initiatives in Underserved Communities
Several successful initiatives demonstrate how to expand access to care in underserved communities. The mobile health clinic model, for instance, brings healthcare directly to communities lacking access to traditional facilities. These clinics offer a range of services, from basic check-ups and vaccinations to chronic disease management and mental health support. One example is the “Health Wagon” in Appalachia, which provides free medical, dental, and vision care to low-income residents in rural areas.
Their efforts have demonstrably improved the health outcomes of this underserved population. Another successful approach is community health worker programs. These programs employ individuals from the community to act as liaisons between healthcare providers and patients, overcoming language and cultural barriers and improving patient engagement. These workers often provide education on health promotion and disease prevention, helping to improve overall health literacy within the community.
Comparison of Care Delivery Models: Telehealth and Mobile Clinics
Telehealth and mobile clinics represent innovative approaches to expanding access to care, each with its own strengths and limitations. Telehealth utilizes technology to deliver healthcare remotely, including virtual consultations, remote monitoring, and online education. This model is particularly effective in overcoming geographic barriers, providing access to specialists and reducing travel time for patients. However, telehealth requires reliable internet access and technological literacy, potentially excluding certain populations.Mobile clinics, on the other hand, directly bring healthcare services to underserved communities.
This model is particularly effective in reaching individuals without transportation or who are hesitant to travel to traditional healthcare facilities. However, mobile clinics have limited capacity and may not offer the full range of services available in a traditional clinic setting. The ideal approach may involve a combination of both models, leveraging the strengths of each to maximize reach and effectiveness.
For example, a mobile clinic could offer initial assessments and then use telehealth for follow-up care or specialist consultations.
Improving Appointment Scheduling and Reducing Wait Times
Streamlining the appointment scheduling process is crucial for improving access to care. Implementing an online appointment scheduling system can improve patient convenience and reduce administrative burden on staff. This system should allow patients to easily book, reschedule, and cancel appointments at their convenience. Automated appointment reminders via text or email can reduce missed appointments and improve efficiency.
Optimizing appointment scheduling algorithms can improve clinic workflow and minimize wait times. For example, utilizing shorter appointment slots for routine check-ups and longer slots for complex cases can improve overall efficiency. Investing in additional staff or expanding clinic hours can also help reduce wait times and increase appointment availability. Finally, implementing a robust patient communication system can allow for proactive communication regarding delays or scheduling changes, improving transparency and patient satisfaction.
Integrating Revenue Protection, Patient Satisfaction, and Access to Care
Successfully navigating the healthcare landscape requires a holistic approach that seamlessly integrates revenue protection, patient satisfaction, and access to care. These three elements are not independent but rather interconnected components of a thriving healthcare system. Improving one area positively impacts the others, creating a synergistic effect that strengthens the overall health of the organization.Improvements in patient satisfaction directly translate into increased patient loyalty and, consequently, higher revenue.
Improving healthcare means protecting revenues, enhancing patient satisfaction, and improving access to care – a tough trifecta! One promising approach I’ve been reading about involves streamlining documentation, and that’s where the news about nuance integrates generative ai scribe epic ehrs comes in. This integration could free up valuable time for clinicians, ultimately leading to better patient care and a more efficient, financially sound system.
Ultimately, it all boils down to achieving that crucial balance of protecting revenues while simultaneously boosting patient satisfaction and access.
Happy patients are more likely to return for future care and recommend the facility to others, organically expanding the patient base. This increased volume of patients, coupled with positive word-of-mouth referrals, contributes significantly to revenue growth. Conversely, negative experiences can lead to patient attrition and damage the facility’s reputation, ultimately impacting revenue.
The Relationship Between Accessible Care and Positive Patient Outcomes
Accessible care, characterized by convenient appointment scheduling, streamlined processes, and readily available services, is intrinsically linked to positive patient outcomes. When patients can easily access the care they need, they are more likely to receive timely treatment, leading to better health outcomes and reduced complications. Improved health outcomes, in turn, translate into fewer readmissions and lower overall healthcare costs, thus positively impacting revenue.
For instance, a clinic with extended hours and online appointment scheduling may experience a higher patient volume and improved patient satisfaction due to increased accessibility, which directly translates into better financial performance.
Visual Representation of Interconnectedness, Protect revenues enhance patient satisfaction and improve access to care w
Imagine a three-circle Venn diagram. Each circle represents one of the three key areas: Revenue Protection, Patient Satisfaction, and Access to Care. The area where all three circles overlap represents the ideal scenario where all three elements work synergistically. In this overlapping area, we see improved patient outcomes, increased patient loyalty, reduced costs, and enhanced revenue generation. The areas where only two circles overlap highlight the positive effects of focusing on any two of these areas simultaneously.
For example, the overlap between Revenue Protection and Patient Satisfaction might showcase how positive patient experiences lead to repeat business and thus higher revenue. The individual circles illustrate the benefits of focusing on each area individually, although the greatest benefits are achieved through the integration of all three.
Strategies for Measuring and Tracking Progress
Effective measurement is crucial for demonstrating the impact of initiatives focused on integrating revenue protection, patient satisfaction, and access to care. Several key performance indicators (KPIs) can be used to track progress. These include:Patient Satisfaction Scores: Regularly collect patient feedback through surveys, online reviews, and comment cards to measure satisfaction levels. Track changes in these scores over time to assess the effectiveness of initiatives aimed at improving the patient experience.Patient Loyalty Metrics: Measure patient retention rates and the number of repeat visits to gauge patient loyalty.
High retention rates indicate a strong patient base and a positive impact on revenue.Access to Care Metrics: Track metrics such as appointment wait times, patient wait times in the facility, and the percentage of patients who receive timely care. These metrics demonstrate improvements in accessibility.Revenue Cycle Performance: Monitor key revenue cycle metrics such as accounts receivable days, denial rates, and collection rates.
Improvements in these areas indicate enhanced revenue protection.By regularly monitoring these KPIs and analyzing trends, healthcare organizations can gain valuable insights into the effectiveness of their strategies and make data-driven decisions to further optimize the integration of revenue protection, patient satisfaction, and access to care.
Addressing Specific Challenges
Balancing the competing demands of revenue maximization and patient care access presents a significant challenge for healthcare organizations. The inherent tension arises from the need to maintain financial stability while simultaneously upholding ethical obligations to provide quality care to all patients, regardless of their ability to pay. This requires a nuanced approach that integrates financial considerations with a patient-centered philosophy.Successfully navigating this requires a strategic approach that prioritizes ethical considerations alongside financial goals.
Ignoring one for the other can lead to unsustainable practices or ethical lapses. Finding the equilibrium point involves careful planning, transparent communication, and a commitment to continuous improvement.
Conflicts Between Revenue Maximization and Patient Access
Maximizing revenue often involves strategies that can inadvertently limit patient access. For example, focusing solely on high-reimbursement procedures might lead to neglecting preventative care or services for low-income populations. Similarly, prioritizing profitable patients over those with complex or chronic conditions can create disparities in access to quality care. These conflicts necessitate a holistic strategy that considers the long-term implications of financial decisions on the overall health of the community served.
The ultimate goal should be a sustainable model that serves all patients effectively.
Solutions for Balancing Financial Sustainability and Ethical Considerations
A key solution lies in implementing a value-based care model. This approach shifts the focus from fee-for-service to rewarding providers for improved patient outcomes and overall population health. This incentivizes providers to focus on preventative care, disease management, and improving the overall health of their patient population, rather than simply maximizing the number of procedures performed. Another crucial aspect is investing in robust financial assistance programs and negotiating favorable payment arrangements with insurance providers to ensure affordability for patients.
Transparency in pricing and billing practices further enhances trust and patient satisfaction.
Successful Collaborations Between Healthcare Providers and Community Organizations
Several successful examples demonstrate the power of collaboration. For instance, partnerships between hospitals and community health centers can expand access to primary care, particularly in underserved areas. These collaborations often involve shared resources, joint programs, and coordinated care plans to improve patient outcomes and reduce healthcare disparities. Another successful strategy involves working with local non-profit organizations that offer transportation assistance, health education, and social support services, thus addressing barriers to access beyond the clinical setting.
These partnerships demonstrate that a community-based approach to healthcare can significantly improve access and patient outcomes.
Managing Patient Expectations and Addressing Complaints Effectively
Effective communication is crucial for managing patient expectations. Clear explanations of treatment plans, costs, and potential outcomes can prevent misunderstandings and reduce the likelihood of complaints. Establishing a robust system for addressing complaints, including prompt responses, thorough investigations, and fair resolutions, is essential for maintaining patient trust. Regular patient satisfaction surveys provide valuable feedback that can be used to identify areas for improvement and refine processes to better meet patient needs.
A proactive approach to addressing concerns fosters a positive patient experience and strengthens the healthcare provider-patient relationship.
Final Thoughts

Source: gannett-cdn.com
Ultimately, the key to success lies in recognizing the inherent synergy between protecting revenues, enhancing patient satisfaction, and improving access to care. By strategically addressing each area, healthcare providers can create a virtuous cycle of growth and improved patient outcomes. It’s not about choosing one over the other; it’s about finding the sweet spot where all three thrive together.
Implementing these strategies might require some initial effort, but the long-term benefits – a healthier practice and happier patients – are well worth it. So, let’s get started on building a better healthcare future, one satisfied patient at a time!
User Queries
What are some common barriers to improving patient satisfaction?
Long wait times, poor communication, impersonal interactions, and lack of clear information are common culprits.
How can telehealth improve access to care?
Telehealth eliminates geographical barriers, allowing patients in remote areas or with mobility issues to access specialists and routine care more easily.
How do I measure the success of these initiatives?
Track key metrics like patient satisfaction scores, revenue growth, appointment wait times, and the number of patients served in underserved areas.
What if my budget is limited?
Start with small, manageable changes. Focus on improving communication, streamlining processes, and leveraging free or low-cost resources like online patient portals.