Credentialing is More Than Compliance Provider Experience & Your Bottom Line
Credentialing is more than compliance its provider experience and your bo – Credentialing is more than compliance; it’s provider experience and your bottom line. Think of it this way: a smooth, efficient credentialing process isn’t just about ticking boxes; it’s about attracting top talent, keeping them happy, and ultimately, boosting your organization’s success. This post dives deep into how a well-oiled credentialing machine can transform your healthcare practice, impacting everything from provider satisfaction to your bottom line.
We’ll explore strategies for streamlining the process, uncovering common pain points, and leveraging technology to create a system that’s both user-friendly and highly efficient. We’ll also look at how to measure the success of your credentialing initiatives and what the future holds for this critical aspect of healthcare operations.
Defining Credentialing Beyond Compliance
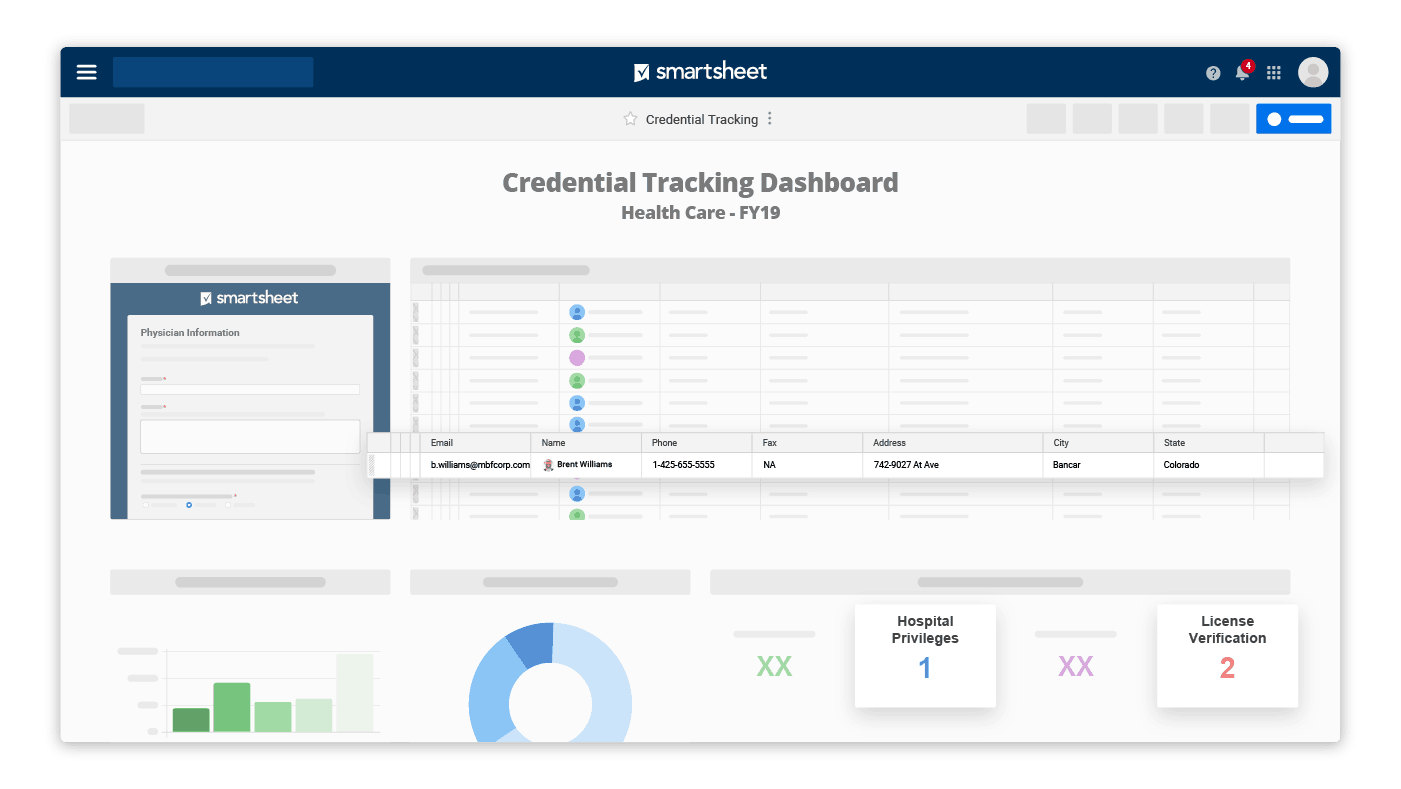
Source: smartsheet.com
Credentialing, often viewed solely as a necessary hurdle to meet regulatory requirements, is far more impactful than simple compliance. A narrow focus on compliance overlooks the significant influence credentialing has on both provider experience and the overall efficiency of a healthcare organization’s operations. Understanding the broader implications of a well-structured credentialing process unlocks substantial benefits beyond avoiding penalties.Viewing credentialing solely as a compliance exercise limits its potential.
Streamlining provider workflows is key to successful credentialing; it’s not just about meeting compliance requirements, but enhancing the overall provider experience and boosting your bottom line. This is why advancements like those detailed in this article, nuance integrates generative ai scribe epic ehrs , are so important. Such tech reduces administrative burden, freeing up providers to focus on patient care, ultimately improving both efficiency and satisfaction, thus making credentialing a smoother, more effective process.
It transforms a strategic opportunity into a burdensome administrative task, potentially leading to delays in provider onboarding, increased administrative costs, and decreased provider satisfaction. This reactive approach fails to leverage credentialing as a tool to enhance the entire healthcare ecosystem. Instead of proactively managing the process to improve efficiency and relationships, organizations may find themselves perpetually playing catch-up, reacting to audits and potential issues rather than strategically optimizing the flow of providers into their network.
Credentialing’s Impact on Provider Experience
A streamlined, efficient credentialing process significantly enhances the provider experience. Positive impacts include reduced administrative burden for providers, allowing them to focus on patient care rather than paperwork. Clear communication, timely updates, and a user-friendly application process can significantly reduce frustration and improve overall satisfaction. Conversely, a cumbersome, opaque, and slow credentialing process can lead to significant delays in onboarding, impacting a provider’s ability to see patients and generate revenue.
This can also create negative perceptions of the organization, potentially deterring qualified providers from joining the network. For example, a lengthy application process with multiple revisions and unclear requirements can lead to frustration and even cause a provider to withdraw their application, impacting the organization’s ability to meet patient demand.
Business Operational Benefits of Robust Credentialing
A robust credentialing process offers significant business operational benefits. Efficient processes reduce administrative costs associated with managing applications, tracking documents, and responding to queries. Automation tools and well-defined workflows can streamline the entire process, minimizing manual intervention and potential errors. Furthermore, a well-managed credentialing system reduces the risk of compliance violations and associated penalties. By proactively managing provider data and ensuring compliance with all relevant regulations, organizations can minimize their exposure to potential legal and financial risks.
For example, a healthcare system that implemented a centralized credentialing database saw a 20% reduction in processing time and a 15% decrease in administrative costs within the first year. This allowed them to onboard new providers more quickly, expanding their service capacity and improving access to care for patients.
Provider Experience and Credentialing
Let’s face it: credentialing is rarely anyone’s favorite process. But it doesn’t have to be a grueling, frustrating experience for providers. By focusing on provider experience, we can transform credentialing from a compliance burden into a strategic advantage, fostering stronger relationships and ultimately improving healthcare delivery. A smooth, efficient credentialing process contributes significantly to a provider’s overall satisfaction and loyalty to a healthcare organization.Streamlining the Credentialing Process to Enhance Provider SatisfactionImproving provider satisfaction hinges on making the credentialing process as efficient and transparent as possible.
This involves leveraging technology and optimizing workflows. A well-designed system minimizes paperwork, reduces manual data entry, and provides real-time updates and communication. Proactive communication is key; providers should be kept informed at every stage of the process, receiving clear instructions and timely responses to their inquiries.
Impact of Positive Credentialing Experience on Provider Retention
A positive credentialing experience significantly influences provider retention. Providers who feel valued and supported throughout the onboarding process are more likely to remain with an organization long-term. Conversely, a negative experience can lead to dissatisfaction and potentially drive providers to seek opportunities elsewhere. Reduced administrative burden and a streamlined process free up providers to focus on patient care, increasing job satisfaction and loyalty.
For example, a large hospital system that implemented an automated credentialing system saw a 15% increase in provider retention within two years, attributing the improvement directly to the reduced administrative burden on its physicians.
Common Pain Points in the Credentialing Process from a Provider’s Perspective
Providers frequently encounter several pain points during the credentialing process. These include excessive paperwork and complex forms, lengthy processing times, unclear instructions, and a lack of communication. The need to repeatedly submit the same information to different payers or facilities adds to the frustration. Inconsistent requirements across different organizations also pose a significant challenge, leading to confusion and delays.
The lack of a centralized, easily accessible portal to track progress and manage documents adds further to the administrative burden.
Design of a User-Friendly Credentialing System
A user-friendly credentialing system should prioritize ease of use and transparency. Key features include a centralized online portal with secure access for providers to upload documents, track their application status, and communicate with credentialing staff. The system should employ automated workflows to reduce manual processing, incorporate data validation to minimize errors, and provide real-time notifications and updates. Integration with existing electronic health record (EHR) systems can further streamline the process by automating data transfer and reducing duplication of effort.
The benefits of such a system include reduced processing times, improved accuracy, enhanced communication, and increased provider satisfaction. This translates to cost savings, improved efficiency, and a more positive provider experience, ultimately contributing to improved patient care.
Business Operational Benefits (BO) of Effective Credentialing

Source: pinimg.com
Efficient credentialing isn’t just about meeting regulatory requirements; it’s a strategic lever for improving operational efficiency and reducing costs within a healthcare organization. A streamlined credentialing process directly impacts the bottom line, enhancing provider satisfaction and ultimately, patient care.
Cost Savings Through Efficient Credentialing
Effective credentialing processes directly translate into significant cost savings. Reducing the time it takes to onboard new providers minimizes the period of lost revenue generation. Furthermore, a well-managed system minimizes errors and denials, saving money on appeals and administrative rework. Automated systems and standardized workflows can significantly reduce labor costs associated with manual data entry, verification, and tracking.
For example, a large hospital system that reduced its credentialing turnaround time by 50% reported a $250,000 annual savings in temporary staffing costs alone. This cost reduction is amplified when considering the avoided costs of lost revenue due to delayed provider onboarding.
Operational Efficiency Comparison: Well-Managed vs. Poorly Managed Credentialing
The difference between a well-managed and poorly managed credentialing process is stark. A well-managed system utilizes technology to automate tasks, track applications, and manage deadlines. This ensures a smooth, consistent process with minimal delays. In contrast, a poorly managed system relies heavily on manual processes, leading to inefficiencies, delays, and increased risk of errors. This can result in significant delays in provider onboarding, impacting patient access to care and creating a backlog of applications.
Thinking about credentialing? It’s not just about ticking boxes; a smooth provider experience directly impacts your bottom line. The recent new york state nurse strike montefiore richmond university deals highlights how crucial positive relationships are – happy staff equals efficient operations, and efficient operations are easier to manage with streamlined credentialing. Ultimately, focusing on provider experience through effective credentialing processes benefits your entire organization.
The administrative burden increases exponentially, leading to higher costs and decreased morale among staff. For instance, a poorly managed system might experience a 20% application rejection rate due to incomplete documentation, whereas a well-managed system might maintain a rejection rate below 5%.
Reduced Administrative Burden Through Improved Credentialing
Streamlining the credentialing process significantly reduces the administrative burden on staff. Automated systems can handle repetitive tasks, freeing up valuable time for staff to focus on more strategic initiatives. Clear workflows and standardized procedures minimize confusion and reduce the need for clarification and follow-up. Centralized databases ensure easy access to information, eliminating the need for searching through multiple files and systems.
This leads to increased staff productivity, improved job satisfaction, and reduced burnout. A healthcare system that implemented a new credentialing software reported a 30% reduction in staff time spent on administrative tasks related to credentialing, allowing them to dedicate more time to patient care coordination.
Key Performance Indicators (KPIs) for Credentialing: Before and After Improvements
| KPI | Before Improvement | After Improvement | % Change |
|---|---|---|---|
| Application Processing Time (Days) | 90 | 45 | -50% |
| Provider Onboarding Time (Days) | 120 | 60 | -50% |
| Application Rejection Rate (%) | 15 | 5 | -67% |
| Staff Time Spent on Credentialing (Hours/Week) | 40 | 20 | -50% |
Technology’s Role in Enhancing Credentialing

Source: tmsbrokerage.com
The healthcare industry is increasingly reliant on technology to streamline operations, and credentialing is no exception. Automating and optimizing this complex process is crucial for improving efficiency, reducing costs, and ensuring accuracy, ultimately leading to a better provider experience. The right technology can transform credentialing from a laborious, manual task into a strategic advantage.Technology can significantly automate various aspects of the credentialing process, reducing manual effort and improving turnaround times.
For example, applications can be submitted and tracked electronically, reducing reliance on paper forms and physical mail. Automated data extraction from submitted documents minimizes the need for manual data entry, lowering the risk of human error. Workflow automation tools can route applications efficiently to the appropriate reviewers, ensuring timely processing. Furthermore, intelligent systems can perform checks for completeness and compliance, flagging potential issues early in the process.
Technologies Improving Credentialing Efficiency and Accuracy
The effective implementation of several technologies can dramatically enhance the efficiency and accuracy of the credentialing process. These technologies work together to create a robust and streamlined system.
Thinking about credentialing? It’s not just about ticking boxes; a smooth provider experience directly impacts your bottom line. The recent news about the new york nurse strike deal reached Mount Sinai Montefiore highlights how crucial positive relationships with healthcare professionals are. Efficient credentialing processes contribute to a better overall provider experience, which ultimately benefits your organization’s success and reputation.
- Credentialing Software: Dedicated credentialing software provides a centralized platform for managing the entire process, from application intake to verification and reporting. These platforms often include features such as automated workflows, data validation, and reporting dashboards.
- Electronic Data Interchange (EDI): EDI allows for the secure electronic exchange of data between healthcare organizations and other entities involved in credentialing, such as payers and licensing boards. This significantly reduces processing time and eliminates the need for manual data entry.
- Optical Character Recognition (OCR): OCR technology can extract data from scanned documents, such as licenses and certifications, automatically populating fields in the credentialing system. This reduces manual data entry and minimizes errors.
- Automated Verification Systems: These systems can automatically verify information against primary sources, such as state medical boards and national registries, ensuring the accuracy and validity of provider credentials.
- Data Analytics Platforms: Advanced data analytics platforms provide valuable insights into credentialing processes, identifying bottlenecks, areas for improvement, and potential risks.
Data Analytics for Optimizing Credentialing Workflows, Credentialing is more than compliance its provider experience and your bo
Data analytics offers powerful tools for optimizing credentialing workflows. By analyzing data from various sources, organizations can identify trends, predict potential issues, and proactively improve their processes.For instance, analyzing application processing times can reveal bottlenecks in the workflow, allowing for targeted improvements. Identifying common reasons for application denials can lead to proactive measures to reduce errors and improve application quality.
Predictive analytics can forecast future credentialing needs, allowing for more effective resource allocation. For example, a hospital system might use data analytics to predict an increase in physician credentialing requests due to an upcoming expansion, allowing them to proactively hire additional staff or invest in technology to manage the increased workload.
Security Implications and Safeguards in Credentialing Technology
The use of technology in credentialing introduces security considerations that must be addressed. Protecting sensitive provider data is paramount. Appropriate safeguards are crucial to maintain compliance with regulations like HIPAA.Implementing robust security measures is essential, including data encryption both in transit and at rest, access control mechanisms, and regular security audits. Multi-factor authentication should be used to protect access to sensitive data and systems.
Regular security training for staff is vital to ensure they understand and adhere to security protocols. Furthermore, choosing credentialing software vendors with strong security reputations and compliance certifications is crucial. A breach of sensitive provider data can have serious consequences, both legally and reputationally, therefore rigorous security measures are not merely recommended, but absolutely necessary.
Measuring the Success of Credentialing Initiatives
Effective credentialing isn’t just about meeting regulatory requirements; it’s about optimizing provider onboarding, enhancing the patient experience, and driving significant business improvements. Measuring the success of your credentialing program is crucial to ensure these benefits are realized and to identify areas for improvement. This involves establishing clear metrics, tracking performance diligently, and conducting regular audits.Successful credentialing programs are built on a foundation of data-driven decision-making.
Understanding key performance indicators (KPIs) allows you to pinpoint bottlenecks, optimize workflows, and ultimately, improve the overall efficiency and effectiveness of the process. By regularly monitoring these metrics and analyzing trends, organizations can proactively address challenges and ensure the program remains aligned with strategic goals.
Key Metrics for Credentialing Program Effectiveness
Several key metrics provide a comprehensive assessment of credentialing program performance. These metrics should be tailored to reflect specific organizational goals and priorities, but generally include:
- Credentialing Time Cycle: The average time it takes to complete the entire credentialing process for a provider, from application submission to final approval. A shorter cycle time indicates greater efficiency.
- Application Completion Rate: The percentage of applications submitted that are completed accurately and timely. A high completion rate suggests effective provider support and clear application instructions.
- Provider Satisfaction: Measured through surveys or feedback mechanisms, this metric reflects the provider experience during the credentialing process. High satisfaction rates indicate a streamlined and supportive process.
- Error Rate: The percentage of applications containing errors or omissions. A low error rate points to robust quality control measures within the process.
- Cost per Credentialed Provider: This metric reflects the overall efficiency of the credentialing process in terms of resource allocation. Lower costs indicate improved efficiency.
Best Practices for Tracking and Reporting on Credentialing Performance
Effective tracking and reporting are vital for continuous improvement. This involves:
- Centralized Data Management: Utilizing a centralized system to collect and store all credentialing data, enabling efficient analysis and reporting.
- Automated Reporting Tools: Leveraging technology to automate the generation of reports on key metrics, ensuring timely and accurate information.
- Regular Performance Reviews: Conducting regular reviews of credentialing performance, identifying trends, and implementing necessary improvements.
- Data Visualization: Presenting data in clear, concise visuals (such as charts and graphs) to facilitate understanding and communication of performance.
- Benchmarking: Comparing performance against industry benchmarks to identify areas for improvement and best practices to emulate.
The Importance of Regular Audits and Reviews of Credentialing Processes
Regular audits and reviews are essential for maintaining compliance, identifying areas for improvement, and ensuring the credentialing program remains effective and efficient. Audits should encompass all aspects of the process, including application review, data accuracy, and adherence to regulatory requirements. Reviews should focus on identifying bottlenecks, streamlining workflows, and enhancing the overall provider experience.
Visual Representation of Efficient Credentialing and Business Outcomes
Imagine a pyramid. The base represents efficient credentialing processes – characterized by shorter processing times, reduced errors, high provider satisfaction, and low costs. As you move up the pyramid, each level represents a positive business outcome directly resulting from efficient credentialing. The second level might show increased provider network size and improved provider retention. The third level showcases enhanced patient access to care and improved quality of care.
The peak of the pyramid represents increased revenue and profitability, a direct consequence of a smoothly functioning and efficient credentialing process. Each level builds upon the previous one, illustrating the direct link between efficient credentialing and key business success.
Future Trends in Credentialing
The healthcare landscape is constantly evolving, driven by technological advancements, shifting regulatory environments, and a growing emphasis on patient-centered care. These factors are significantly impacting the future of credentialing, pushing the process beyond simple compliance to become a strategic lever for improving provider experience and operational efficiency. We’re moving towards a more streamlined, data-driven, and technologically advanced approach to credentialing.The integration of artificial intelligence (AI) and machine learning (ML) is reshaping credentialing processes.
AI-powered systems can automate tasks like data entry, verification, and primary source verification (PSV), significantly reducing manual effort and processing time. ML algorithms can identify patterns and anomalies in provider data, flagging potential issues for human review and improving accuracy. For example, an AI system could automatically cross-reference a provider’s license information with state databases, instantly flagging any discrepancies or expirations.
This proactive approach minimizes delays and ensures compliance.
Automation and AI in Credentialing
Automation is no longer a futuristic concept; it’s a present-day necessity for efficient credentialing. The implementation of robotic process automation (RPA) and AI-powered tools allows for the automation of repetitive tasks, freeing up credentialing staff to focus on more complex and value-added activities. This includes tasks like data entry, verification of licenses and certifications, and primary source verification. The use of AI in analyzing large datasets allows for the identification of potential risks and areas for improvement in the credentialing process, leading to proactive risk mitigation and improved compliance.
For instance, an RPA bot could automatically extract data from application forms and populate the credentialing database, reducing human error and improving data accuracy.
Blockchain Technology in Credentialing
Blockchain technology offers a secure and transparent platform for managing and verifying provider credentials. By storing credential information on a distributed ledger, blockchain enhances data security and prevents unauthorized access or modification. This secure system improves the integrity of credentialing data and facilitates seamless sharing of information between healthcare organizations. A blockchain-based system could allow providers to securely store and share their credentials with multiple healthcare organizations, eliminating the need for repetitive verification processes.
Imagine a system where a provider’s credentials are verified once and then automatically accessible to any healthcare organization they choose to work with.
Impact of Regulatory Changes
Changes in federal and state regulations significantly impact credentialing practices. For example, new regulations concerning data privacy (like HIPAA and GDPR) necessitate robust security measures and compliance protocols. Changes in provider licensing requirements or Medicare/Medicaid participation rules necessitate updates to credentialing workflows and processes. Staying abreast of these changes and adapting credentialing processes accordingly is crucial for compliance and avoiding potential penalties.
For example, the implementation of new telehealth regulations necessitates changes in the credentialing process to accommodate the specific requirements of telehealth providers.
Last Point
Ultimately, effective credentialing isn’t just about meeting regulatory requirements; it’s a strategic investment in your organization’s future. By focusing on provider experience and leveraging technology to streamline the process, you can unlock significant operational efficiencies, reduce administrative burdens, and ultimately, improve your bottom line. It’s about creating a system that works
-for* you, not against you, leading to a happier workforce and a healthier business.
Q&A: Credentialing Is More Than Compliance Its Provider Experience And Your Bo
What are the biggest risks of a poorly managed credentialing process?
Significant risks include delays in provider onboarding, decreased provider satisfaction and retention, increased administrative costs, potential compliance violations, and reputational damage.
How can I measure the ROI of improving my credentialing process?
Track key metrics like time-to-credentialing, cost per credentialed provider, provider satisfaction scores, and the number of compliance issues. Compare these before and after implementing improvements to quantify the return on your investment.
What are some common provider pain points during credentialing?
Common frustrations include excessive paperwork, unclear requirements, slow turnaround times, lack of communication, and difficulty accessing the system or support.
How often should I audit my credentialing process?
Regular audits, ideally annually or semi-annually, are crucial to ensure compliance, identify areas for improvement, and maintain a smooth, efficient system.