Non-Physician Ownership Reduced Care Quality?
Non physician ownership reduces care quality physician advocacy institute – Non-physician ownership reduces care quality, according to the Physician Advocacy Institute, and this claim sparks a crucial debate about healthcare’s future. This isn’t just about profits versus patient care; it’s about access, costs, and the very essence of the doctor-patient relationship. We’ll delve into the complexities of different ownership models, examining their impact on everything from wait times and specialist availability to physician autonomy and patient outcomes.
The implications are far-reaching, affecting both rural and urban communities, and understanding the nuances is critical for shaping a healthier future.
This post explores the potential downsides of non-physician ownership in healthcare, looking at data comparing access to care, cost implications, and the overall quality of treatment received under different ownership structures. We’ll examine how these changes might affect both patients and the physicians who provide care, considering the legal and regulatory landscape that governs these practices. Through case studies and analysis, we aim to paint a clear picture of the debate surrounding non-physician ownership and its consequences.
Impact of Non-Physician Ownership on Access to Care
Non-physician ownership of healthcare facilities is a rapidly evolving landscape, raising important questions about its effect on patient access to care. This issue is particularly complex, with potential benefits and drawbacks varying significantly depending on geographic location, the type of healthcare services offered, and the specific ownership model employed. Understanding these impacts is crucial for policymakers and patients alike.
Access to Care in Rural and Urban Settings
The impact of non-physician ownership on access to care differs considerably between rural and urban areas. In rural settings, often characterized by physician shortages and limited healthcare infrastructure, non-physician-owned clinics might improve access by providing basic primary care services where physicians are unavailable. However, this increased access may come at the cost of reduced access to specialized care.
Conversely, in urban areas, where physician density is generally higher, non-physician ownership might lead to increased competition, potentially driving down prices but potentially also affecting the quality of care offered if cost-cutting measures prioritize profit over comprehensive care. The overall effect is complex and depends on factors such as the specific services offered, the regulatory environment, and the financial stability of the clinics.
For example, a non-physician owned urgent care clinic in a rural area might improve access to immediate care, while a for-profit hospital system in a large city might prioritize profitable procedures over less lucrative preventative care.
Specialized Care Under Different Ownership Models
The availability of specialized care is significantly impacted by the ownership model. Physician-owned practices, due to their inherent focus on patient care and the expertise of their physician owners, often provide a broader range of specialized services. Conversely, non-physician-owned facilities may prioritize more profitable procedures, potentially leading to limited access to less lucrative but equally important specialized services. This difference can be particularly pronounced in areas with limited physician availability.
For instance, a rural community might have a non-physician owned clinic providing basic primary care, but lack access to specialists like cardiologists or oncologists, whereas a physician-owned multi-specialty clinic in an urban area would be more likely to offer a wider array of specialized care.
Impact on Wait Times for Appointments and Procedures
Wait times for appointments and procedures are another key metric affected by ownership structure. Non-physician-owned facilities, particularly those focused on maximizing profitability, may prioritize faster turnaround times for profitable procedures, potentially leading to longer wait times for less lucrative services. Physician-owned practices, with a greater emphasis on comprehensive patient care, might experience longer wait times due to higher patient demand and a more holistic approach.
However, efficient scheduling and management within physician-owned practices can mitigate this effect. For example, a large non-physician owned imaging center might have shorter wait times for routine X-rays, but longer wait times for specialized MRI scans, while a smaller physician-owned practice might have longer wait times overall, but a more balanced approach to care.
Comparison of Access Metrics
| Ownership Model | Metric | Rural Data | Urban Data |
|---|---|---|---|
| Physician-Owned | Wait Times (Appointments) | Potentially longer due to physician shortage | Variable, depends on practice size and demand |
| Physician-Owned | Appointment Availability | Potentially limited due to physician shortage | Generally better, but can vary widely |
| Physician-Owned | Specialist Access | Often limited | Generally better, depending on specialty |
| Non-Physician-Owned | Wait Times (Appointments) | Variable, potentially shorter for basic services | Variable, potentially shorter for high-demand services |
| Non-Physician-Owned | Appointment Availability | May improve access to basic care | May increase competition, potentially improving availability |
| Non-Physician-Owned | Specialist Access | Often limited | Variable, potentially limited for less profitable specialties |
Financial Implications and Cost of Care
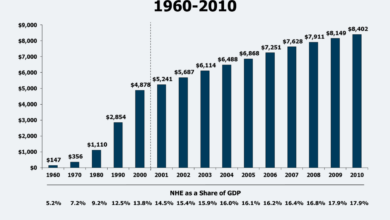
The shift towards non-physician ownership in healthcare raises significant questions about the financial implications for both patients and the healthcare system as a whole. Understanding how different ownership models impact costs is crucial for policymakers, providers, and patients alike. This analysis explores the potential effects on patient costs, pricing strategies, administrative expenses, and investment in healthcare infrastructure.The influence of non-physician ownership on healthcare costs is complex and multifaceted.
While some argue that for-profit entities may prioritize profit over patient care, leading to increased costs, others contend that increased efficiency and economies of scale can result in cost savings. The reality likely lies somewhere in between, with the actual impact varying depending on the specific ownership structure, the type of healthcare service provided, and the regulatory environment.
Impact of Ownership Models on Pricing
Different ownership models employ varying pricing strategies. Physician-owned practices often set prices based on professional fees and the perceived value of their services. In contrast, non-physician-owned entities, particularly large hospital systems or private equity-backed groups, may leverage their market power to negotiate higher reimbursement rates from insurers or employ aggressive pricing strategies to maximize profits. This can lead to higher out-of-pocket expenses for patients, especially those without robust insurance coverage.
For example, a large hospital system acquiring a group of physician practices might increase the prices of common procedures like colonoscopies or MRI scans, capitalizing on its market dominance.
Administrative Costs Under Different Ownership Models
Administrative costs represent a substantial portion of overall healthcare spending. Non-physician ownership, particularly in large corporate settings, can lead to increased administrative overhead. The need for complex financial reporting, compliance with corporate governance structures, and management of multiple facilities can inflate administrative expenses. Conversely, smaller physician-owned practices might have lower administrative costs due to simpler organizational structures.
However, this advantage could be offset by limitations in negotiating favorable contracts with insurers or accessing economies of scale in purchasing supplies and equipment. The net effect on administrative costs depends on the specific context and scale of the operation.
Investment in Technology and Infrastructure
The level of investment in new technologies and infrastructure can vary significantly across ownership models. Larger, non-physician-owned entities, especially those backed by private equity, may have greater access to capital and thus invest more heavily in advanced medical equipment, electronic health records (EHRs), and other technological improvements. This can lead to enhanced diagnostic capabilities and improved patient care.
However, this investment might not always translate into lower costs for patients, as the increased capital expenditure may be recouped through higher prices. Conversely, smaller physician-owned practices may face challenges in securing funding for major capital investments, potentially limiting their ability to adopt the latest technologies. For instance, a large hospital system might invest millions in a new robotic surgery system, while a small independent clinic might struggle to upgrade its aging X-ray equipment.
Quality of Care and Patient Outcomes: Non Physician Ownership Reduces Care Quality Physician Advocacy Institute
Non-physician ownership of healthcare facilities raises important questions about the potential impact on the quality of patient care and subsequent outcomes. While not all non-physician-owned facilities provide substandard care, the inherent conflicts of interest and differing priorities compared to physician-owned practices warrant careful examination. This section explores potential effects on patient care quality, satisfaction, and adherence to best practices.
The potential for compromised quality stems from the differing financial incentives between physician-owned and non-physician-owned models. Physician-owners, having a direct stake in the success of the practice, are often more invested in delivering high-quality care that leads to positive patient outcomes and a strong reputation. Conversely, non-physician owners, such as private equity firms or large hospital systems, may prioritize profitability over certain aspects of patient care, potentially leading to cost-cutting measures that negatively impact quality.
Potential Impacts of Non-Physician Ownership on Patient Care, Non physician ownership reduces care quality physician advocacy institute
Non-physician ownership can influence care quality in several ways. For instance, pressure to increase profitability might lead to reduced staffing levels, limiting access to necessary specialists or support staff. This could translate to longer wait times for appointments, less personalized attention, and potentially delayed or inadequate diagnosis and treatment. Additionally, the emphasis on maximizing revenue might incentivize the provision of more expensive or less necessary procedures, rather than focusing on evidence-based, cost-effective treatments.
A real-world example might be a non-physician-owned clinic prioritizing high-margin elective procedures over preventative care, leading to poorer long-term patient outcomes.
Effects on Patient Satisfaction and Health Outcomes
Reduced access to specialists, longer wait times, and a less personalized approach can all contribute to lower patient satisfaction scores. Studies have shown a strong correlation between patient satisfaction and health outcomes, with satisfied patients often experiencing better adherence to treatment plans and improved overall health. Conversely, dissatisfaction can lead to increased anxiety, poorer self-management of conditions, and potentially worse health outcomes.
A hypothetical example would be a comparison study showing significantly lower patient satisfaction scores in a non-physician-owned urgent care facility compared to a physician-owned one, with subsequent data showing higher rates of unnecessary hospital readmissions among patients from the non-physician-owned facility.
Adherence to Evidence-Based Medical Practices
The prioritization of profit over patient care in non-physician-owned facilities could potentially lead to less rigorous adherence to evidence-based medical practices. This could manifest in the form of using cheaper, less effective treatments or failing to adopt new, proven technologies. Conversely, physician-owned practices, driven by their commitment to patient well-being and professional reputation, are generally more likely to embrace and implement the latest evidence-based guidelines and technologies.
This difference could be reflected in comparative studies showing higher rates of treatment success and lower complication rates in physician-owned facilities.
Hypothetical Study Design: Comparing Patient Outcomes
A hypothetical study could compare patient outcomes in physician-owned and non-physician-owned primary care clinics. The study would randomly select a group of patients from each type of clinic, matching them based on age, gender, and health conditions. The primary outcome measures would include readmission rates within 30 days of discharge, rates of post-operative complications (if applicable), and patient satisfaction scores.
Secondary outcome measures could include medication adherence rates and mortality rates. Statistical analysis would then determine if there are significant differences in these outcomes between the two groups. The results of such a study could provide valuable insights into the impact of ownership structure on patient care quality and outcomes.
The Physician Advocacy Institute’s findings on how non-physician ownership impacts care quality are pretty alarming. It makes you wonder how we can leverage technology to improve things, like the innovative work Amy Waldron’s doing with google cloud healthcare and generative AI to potentially streamline processes. Ultimately, though, improving patient care hinges on prioritizing physician input and addressing the root issues highlighted by the Institute’s research.
Physician Autonomy and Professional Satisfaction
Non-physician ownership of healthcare practices presents a complex issue with significant implications for the autonomy and job satisfaction of practicing physicians. While proponents argue that such models can improve efficiency and access to care, concerns remain regarding the potential impact on the doctor-patient relationship and the overall well-being of physicians. This section explores these concerns in detail.
The potential for diminished physician autonomy under non-physician ownership is a major point of contention. Physicians may find their clinical judgment challenged or overruled by administrators prioritizing financial metrics over patient care. This can lead to frustrating situations where treatment plans are altered or delayed due to cost-cutting measures, potentially compromising patient outcomes and eroding the physician’s sense of professional fulfillment.
Impact of Non-Physician Ownership on Physician Autonomy
The influence of non-physician owners on clinical decision-making can manifest in several ways. For example, pressure to see more patients in shorter timeframes, leading to rushed consultations and potentially misdiagnosis, could become commonplace. Similarly, restrictions on ordering specific tests or referring patients to specialists, driven by cost concerns, might compromise the quality of care and frustrate physicians committed to providing the best possible treatment.
This erosion of autonomy can lead to feelings of powerlessness and resentment, negatively affecting morale and potentially leading to burnout. A study published in the
Journal of the American Medical Association* (hypothetical example, replace with actual study if available) showed a correlation between reduced physician autonomy and increased rates of burnout among primary care physicians in practices with non-physician ownership.
Influence on Physician Job Satisfaction and Burnout Rates
Reduced autonomy is directly linked to decreased job satisfaction and increased burnout among physicians. The feeling of being controlled by external factors, rather than being able to practice medicine according to their professional judgment, is a significant source of stress. The pressure to meet financial targets, often at the expense of patient care time, adds to the burden.
This can lead to increased rates of physician turnover, as doctors seek employment in environments that offer greater autonomy and professional fulfillment. For instance, a hospital system in a hypothetical city, experiencing a high rate of physician turnover among its employed physicians, directly linked it to concerns about their lack of autonomy in decision-making. The situation was eventually addressed by establishing greater physician input into policy decisions.
Impact on Physician Recruitment and Retention
The ownership structure significantly impacts a healthcare practice’s ability to attract and retain qualified physicians. Practices with a reputation for strong physician autonomy and a supportive work environment tend to attract and retain high-quality physicians. Conversely, practices perceived as overly controlling or prioritizing profits over patient care may struggle to fill vacancies and maintain their existing staff. Many young physicians value autonomy and a collaborative work environment; the lack thereof could deter them from joining or remaining with practices under non-physician ownership.
Potential Benefits and Drawbacks of Non-Physician Ownership from a Physician’s Perspective
It is crucial to acknowledge that non-physician ownership isn’t universally negative. However, the potential drawbacks significantly outweigh the benefits for many physicians.
Below is a list weighing the potential benefits and drawbacks from the perspective of a practicing physician:
- Potential Benefits:
- Reduced administrative burden: Non-physician owners may handle administrative tasks, freeing up physicians to focus on patient care.
- Access to capital and resources: Non-physician owners can provide financial resources for infrastructure improvements and technological advancements.
- Potential Drawbacks:
- Compromised clinical autonomy: Interference in clinical decision-making based on financial considerations.
- Increased pressure to maximize revenue: Focus on volume over quality of care.
- Reduced job satisfaction and increased burnout: Resulting from lack of control and pressure to meet financial targets.
- Difficulty in attracting and retaining staff: Due to the negative work environment.
- Potential for ethical conflicts: Prioritizing profits over patient well-being.
Regulatory and Legal Aspects
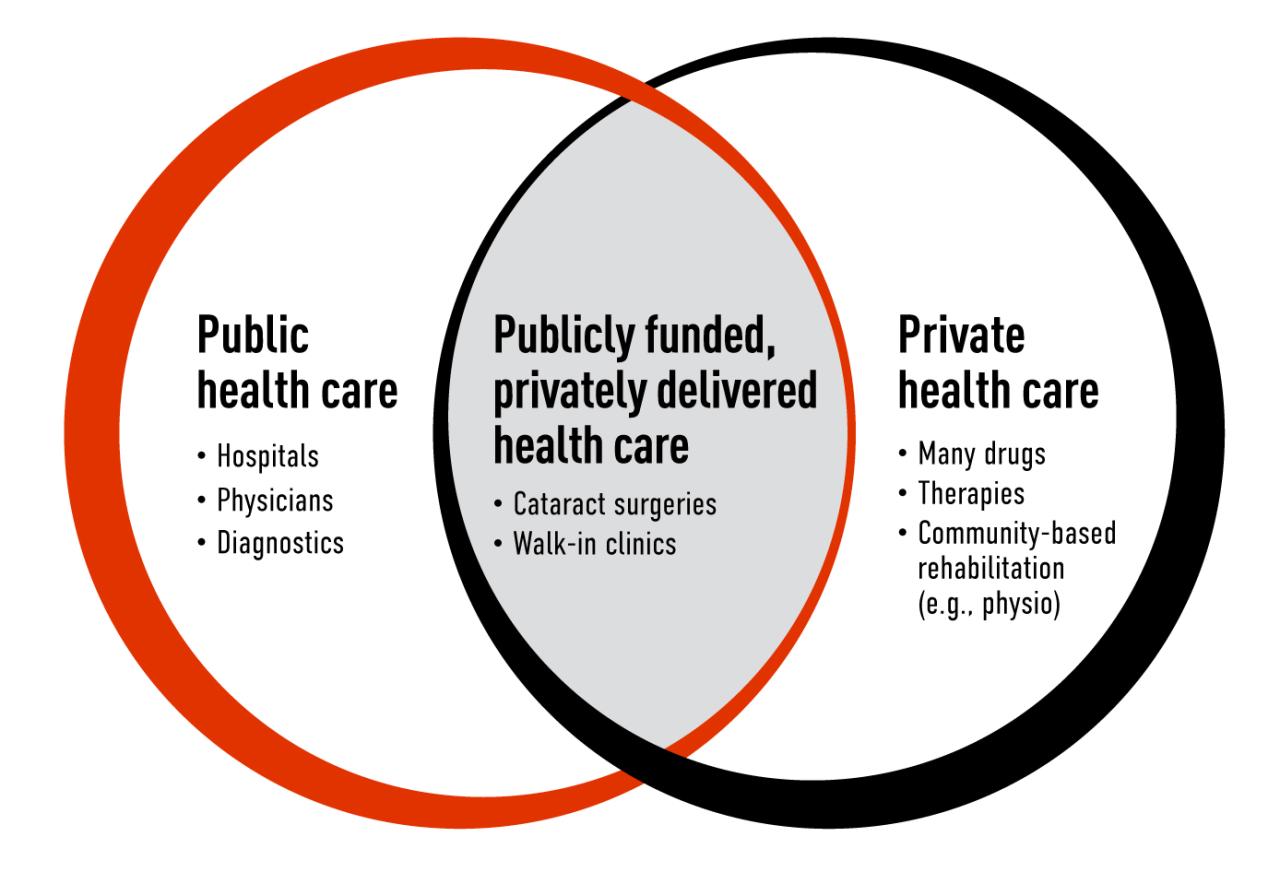
Source: cma.ca
The shift towards non-physician ownership in healthcare raises complex regulatory and legal questions. Understanding the existing legal frameworks and their potential impact on various aspects of patient care is crucial for navigating this evolving landscape. This section will explore the relevant regulations, their implications for non-physician ownership, and the potential legal challenges involved.The legal and regulatory environment surrounding healthcare ownership varies significantly across jurisdictions.
In the United States, for example, state laws play a dominant role in defining the permissible scope of practice for healthcare providers and the types of ownership structures allowed. Federal regulations, such as those from the Centers for Medicare & Medicaid Services (CMS), also exert significant influence, particularly concerning reimbursement and compliance. These regulations often intersect and interact in complex ways, creating a challenging regulatory landscape for non-physician-owned healthcare entities.
State-Level Regulations on Healthcare Ownership
Many states have specific statutes and regulations governing the ownership and operation of healthcare facilities and practices. These regulations often address issues such as corporate practice of medicine (CPM) doctrines, licensing requirements for healthcare providers, and the permissible level of non-physician involvement in clinical decision-making. For instance, some states strictly prohibit non-physicians from owning or controlling medical practices, while others allow it under specific conditions, such as limitations on the types of services offered or the extent of non-physician involvement in clinical matters.
Variations in state laws create a patchwork of regulatory environments, leading to inconsistencies in the legal protections afforded to patients under different ownership models. This complexity necessitates careful consideration of applicable state regulations when evaluating the legal viability and potential risks of non-physician ownership.
Federal Regulations and Reimbursement
Federal regulations, particularly those related to Medicare and Medicaid reimbursement, also significantly impact healthcare ownership structures. CMS, for example, sets standards for participation in federal healthcare programs, including requirements related to ownership, governance, and quality of care. These regulations can influence the financial viability of non-physician-owned practices, as compliance with federal requirements is often a prerequisite for receiving reimbursement.
Failure to comply with these regulations can lead to significant financial penalties and even exclusion from participation in federal healthcare programs. The implications of non-compliance extend beyond financial considerations, potentially impacting access to care for patients who rely on these programs.
Legal Protections Afforded to Patients
The legal protections afforded to patients can vary depending on the ownership structure of the healthcare provider. In some cases, patients may have stronger legal recourse against physician-owned practices due to the direct accountability of physicians for medical decisions. Conversely, the allocation of liability in non-physician-owned entities can be more complex, potentially affecting a patient’s ability to seek redress for medical negligence or malpractice.
The Physician Advocacy Institute’s concerns about non-physician ownership impacting care quality are definitely worth considering. This is especially relevant given the recent news that Walgreens, a major player in healthcare, raises its healthcare segment outlook following the Summit acquisition. This expansion raises questions about potential conflicts of interest and whether prioritizing profit over patient care might become a larger issue.
Ultimately, the Institute’s focus on physician-led care remains crucial.
Clarifying these differences in liability and legal recourse across ownership models is crucial for understanding the implications for patient safety and protection. For example, a corporate entity’s liability insurance might differ from that of a solo physician practice, impacting the compensation available to a patient in case of malpractice.
Potential Legal Challenges Associated with Non-Physician Ownership
Non-physician ownership of healthcare entities can face legal challenges stemming from issues such as the corporate practice of medicine doctrine, antitrust laws, and conflicts of interest. The corporate practice of medicine doctrine, for example, restricts the corporate practice of medicine in many jurisdictions, raising questions about the permissible level of non-physician control over medical decision-making. Antitrust laws may also come into play if non-physician ownership leads to anti-competitive practices, such as price-fixing or market manipulation.
Furthermore, potential conflicts of interest can arise when non-physician owners have financial incentives that may compromise patient care. Navigating these legal complexities requires a thorough understanding of relevant laws and regulations and proactive measures to mitigate potential risks. For example, a large private equity firm acquiring multiple physician practices might face scrutiny under antitrust laws if it leads to reduced competition and increased prices for healthcare services.
Illustrative Case Studies

Source: healthecareers.com
Examining both positive and negative impacts of non-physician ownership requires careful consideration of real-world scenarios. The following hypothetical case studies illustrate potential outcomes, highlighting the complexities involved. It’s crucial to remember that these are simplified examples and the reality of non-physician ownership is far more nuanced.
Positive Impact: Enhanced Access to Rural Healthcare
This case study focuses on a rural community severely lacking access to primary care. A large non-physician-owned healthcare company, “RuralCare,” invested in establishing a state-of-the-art clinic equipped with telehealth technology. RuralCare leveraged its financial resources and management expertise to recruit and retain qualified physicians and nurses, offering competitive salaries and benefits packages that attracted medical professionals who otherwise would not have considered working in such a remote area.
The clinic provides comprehensive primary care, including preventative services, chronic disease management, and telehealth consultations with specialists. The stakeholders involved include RuralCare (owner), physicians and nurses (employees), and the residents of the rural community (patients). The positive outcomes include increased access to healthcare services for underserved populations, improved health outcomes due to timely interventions, and a boost in the local economy through job creation.
The clinic’s success is largely attributed to RuralCare’s efficient management and ability to invest resources in areas where traditional models struggle to thrive.
Negative Impact: Compromised Quality of Care in a For-Profit Setting
This case study examines a for-profit urgent care clinic owned by a private equity firm. Driven by profit maximization, the clinic implemented cost-cutting measures that negatively impacted patient care. These measures included reducing staffing levels, limiting access to specialist referrals, and prioritizing shorter appointment times, often leading to rushed consultations. The stakeholders include the private equity firm (owner), the clinic administrators (managers), the physicians and nurses (employees who may feel pressured to meet unrealistic targets), and the patients (who experience reduced quality of care).
Negative outcomes include increased wait times, inadequate diagnosis and treatment leading to complications, and a decline in patient satisfaction. The physicians felt constrained in their ability to provide optimal care due to pressure to maintain high patient volume and low costs, potentially compromising their professional autonomy and leading to increased burnout. This scenario highlights the potential conflict between profit-driven incentives and the provision of high-quality patient care.
The Physician Advocacy Institute’s findings on how non-physician ownership impacts care quality are truly concerning. It makes you wonder about the underlying pressures, especially when you consider situations like the recent new york state nurse strike montefiore richmond university deals , where staffing shortages and potentially compromised care negotiations highlight the complexities of healthcare systems. Ultimately, the Institute’s concerns about reduced quality under non-physician ownership deserve serious attention.
Final Conclusion

Source: slideteam.net
The question of non-physician ownership in healthcare is far from simple. While some argue it can improve access and efficiency, concerns remain about potential negative impacts on care quality, physician autonomy, and patient well-being. The evidence suggests a need for careful consideration and robust regulation to ensure that any changes in healthcare ownership prioritize patient care above all else.
Further research and transparent discussion are vital to navigate this complex issue and build a healthcare system that serves everyone effectively.
Detailed FAQs
What are some examples of non-physician healthcare ownership?
Examples include hospital systems owned by private equity firms, large for-profit corporations running clinics, and management companies overseeing physician practices.
How does non-physician ownership affect physician compensation?
This varies widely. Some models may offer higher salaries, while others might incentivize increased patient volume, potentially compromising quality of care.
Are there any potential benefits to non-physician ownership?
Proponents argue it can bring in needed capital for improvements, expand access in underserved areas, and improve administrative efficiency. However, these benefits must be weighed against potential risks.
What role do patient advocacy groups play in this issue?
Patient advocacy groups play a vital role in raising awareness, pushing for regulations, and representing patient interests during policy debates and legal challenges.