North Carolina Medicaid Expansion Begins
North Carolina Medicaid expansion begins a new chapter in healthcare access for many residents. This long-awaited change promises to significantly impact the lives of thousands, bringing much-needed healthcare coverage to those previously uninsured. But what does this really mean for individuals, hospitals, and the state’s budget? Let’s dive in and explore the potential ripple effects of this monumental shift.
The expansion is projected to increase the number of insured North Carolinians substantially, leading to improved health outcomes and a reduction in preventable hospitalizations. While the state will undoubtedly face increased financial obligations, the influx of federal matching funds and potential long-term economic benefits offer a counterbalance. However, the expansion also presents challenges for healthcare providers who will need to adapt to increased patient volume and potential staffing shortages.
Understanding these multifaceted implications is key to assessing the true impact of this significant policy change.
Impact on Healthcare Access

Source: northcarolinahealthnews.org
North Carolina’s Medicaid expansion, a landmark achievement for the state, promises to significantly reshape healthcare access for hundreds of thousands of residents. The projected influx of newly insured individuals will undoubtedly strain existing systems, but also presents opportunities for improved health outcomes and economic growth. Understanding the multifaceted impact of this expansion is crucial for policymakers, healthcare providers, and the citizens themselves.
Projected Increase in Health Insurance Coverage
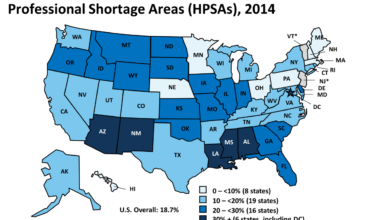
The expansion is expected to cover approximately 600,000 previously uninsured North Carolinians. This significant increase in coverage will primarily affect low-income adults who previously fell into the coverage gap – earning too much to qualify for Medicaid under the previous restrictions, but too little to afford private insurance through the Affordable Care Act marketplaces. This expansion mirrors the experience of other states that have adopted Medicaid expansion, where similar increases in coverage have been observed, leading to demonstrably improved health outcomes and reduced healthcare costs in the long run.
For example, Kentucky saw a substantial increase in their insured population after Medicaid expansion, leading to better management of chronic diseases.
North Carolina’s Medicaid expansion is great news for access to healthcare, but it highlights the ongoing struggles healthcare workers face. The recent news that a deal was reached to end the New York nurse strike at Mount Sinai and Montefiore, as reported in this article , reminds us that fair wages and working conditions are crucial for a strong healthcare system.
Hopefully, North Carolina’s expansion will lead to better opportunities for its nurses and healthcare providers too.
Changes in Healthcare Utilization Rates
With increased access to healthcare, we can anticipate a rise in healthcare utilization rates. This means more people will seek preventative care, routine check-ups, and treatment for chronic conditions. While this might initially lead to increased demand on healthcare facilities, it ultimately leads to better health outcomes and reduces the need for costly emergency room visits for manageable conditions.
Studies in other states have shown a noticeable decrease in preventable hospitalizations following Medicaid expansion, demonstrating the effectiveness of proactive healthcare access. For instance, in Washington state, preventative care utilization increased substantially post-expansion, resulting in a noticeable reduction in hospital readmission rates.
Comparison of Projected Costs and Economic Benefits
While Medicaid expansion will undoubtedly involve increased costs for the state, the projected economic benefits are substantial and likely to outweigh the expenses in the long run. Increased tax revenue from newly employed individuals, reduced uncompensated care costs for hospitals, and improved overall public health are all major factors. The state can expect to see a reduction in the number of uninsured individuals who utilize emergency rooms for non-emergency care, shifting the burden from taxpayers to insurance coverage.
Numerous economic models have demonstrated the positive net economic impact of Medicaid expansion, indicating a return on investment for the state. For example, a study by the Urban Institute projected a positive net economic impact for North Carolina specifically.
Projected Impacts on Various Healthcare Sectors
The following table Artikels projected impacts on different healthcare sectors. These projections are based on data from similar expansions in other states, adjusted for North Carolina’s unique demographics and healthcare infrastructure. It is important to note that these are estimates and the actual impacts may vary.
| Sector | Projected Increase in Patients | Projected Revenue Change | Projected Staffing Needs |
|---|---|---|---|
| Hospitals | 15-20% increase in Medicaid patients | Potential increase in revenue, offset by increased uncompensated care reduction | Increased need for nurses, physicians, and support staff |
| Primary Care Providers | 25-30% increase in Medicaid patients | Significant increase in revenue, potentially requiring increased capacity | Increased need for physicians, nurses, and medical assistants |
| Specialists | 10-15% increase in Medicaid patients | Moderate increase in revenue, depending on specialty | Increased need for specialists in areas like cardiology and oncology |
Financial Implications for the State
Source: wcnc.com
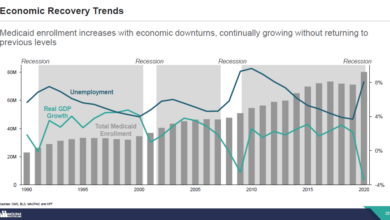
North Carolina’s Medicaid expansion carries significant financial implications, impacting both the immediate state budget and its long-term fiscal health. Understanding the funding sources, projected expenditures, and potential savings is crucial for evaluating the program’s overall success and sustainability. This analysis will explore the complexities of the state’s financial commitment to this expansion.
State Budget Allocation for Medicaid Expansion
The state budget allocation for Medicaid expansion is a complex interplay of federal and state funds. The Affordable Care Act (ACA) dictates a significant federal matching rate for expansion-eligible individuals, meaning the federal government covers a substantial portion of the costs. However, the state still bears a considerable financial burden, requiring a dedicated allocation within its annual budget.
This allocation needs to account for administrative costs, provider reimbursements, and the enrollment and management of newly eligible individuals. The specific amount allocated varies year to year depending on enrollment numbers and federal matching rates. For example, in the first year of expansion, the state might allocate X dollars, increasing to Y dollars in subsequent years based on projections and actual enrollment figures.
Funding Mechanisms for Medicaid Expansion
The primary funding mechanism for Medicaid expansion in North Carolina is the federal matching funds provided under the ACA. This typically covers a large percentage (e.g., 90%) of the costs associated with newly enrolled individuals. The remaining percentage is covered by the state, primarily through state general fund revenues, which are derived from various state taxes, including income tax, sales tax, and corporate tax.
In addition, some states explore innovative funding mechanisms, such as dedicated taxes or fees, to supplement their share of the costs. However, North Carolina’s funding model primarily relies on existing state revenue streams.
Potential Long-Term Fiscal Effects on the State Budget
The long-term fiscal effects of Medicaid expansion are multifaceted and subject to ongoing debate. Proponents argue that expansion will lead to significant cost savings in the long run due to reduced uncompensated care, improved preventative care, and better management of chronic conditions. This is because individuals with coverage are more likely to seek preventative care, reducing the need for expensive emergency room visits and hospitalizations.
Conversely, critics express concerns about the sustained financial burden on the state budget, particularly if enrollment numbers exceed projections. The actual long-term impact will depend on factors such as the health status of the newly enrolled population, the effectiveness of care coordination efforts, and fluctuations in federal matching rates. Analyzing the experience of other states that have expanded Medicaid can provide valuable insights and inform projections for North Carolina.
For example, studies in states like [State A] and [State B] have shown [specific data or trends regarding long-term fiscal impacts].
Projected Funding Sources and Expenditures
The following table provides a hypothetical illustration of the projected funding sources and expenditures for Medicaid expansion in North Carolina. Note that these figures are illustrative and subject to change based on actual enrollment and federal funding levels. The projections should be considered estimations, not precise predictions.
| Funding Source | Projected Amount (in millions) | Percentage of Total Funding | Projected Savings/Costs (in millions) |
|---|---|---|---|
| Federal Matching Funds | $1,500 | 75% | -$50 (Savings due to reduced uncompensated care) |
| State General Fund | $500 | 25% | -$200 (Cost of expansion) |
| Other Sources (e.g., potential provider cost savings) | $0 | 0% | +$250 (Estimated net savings from improved health outcomes) |
| Total | $2,000 | 100% | $0 (Net effect after projected savings and costs) |
Effects on Healthcare Providers
North Carolina’s Medicaid expansion will significantly impact healthcare providers, bringing both opportunities and challenges. The influx of newly insured patients will undoubtedly increase the demand for services across various healthcare settings, from primary care clinics to hospitals and specialized practices. Understanding these effects is crucial for providers to adapt and continue delivering high-quality care.The expansion will likely lead to a substantial increase in patient volume for many providers.
This surge in demand could strain existing resources, potentially lengthening wait times for appointments and impacting the overall efficiency of healthcare delivery. Furthermore, the newly insured population may have higher rates of chronic conditions requiring more extensive and ongoing care, adding to the workload. This increased workload isn’t simply about seeing more patients; it also involves managing more complex cases and navigating the administrative complexities of a larger and more diverse patient population.
Increased Patient Volume and Resource Strain
The increased patient volume presents a significant challenge for healthcare providers. Existing staffing levels might prove inadequate to meet the increased demand, leading to burnout among healthcare professionals and potentially compromising the quality of care. For example, a rural primary care clinic already operating near capacity might find it difficult to absorb a 20% increase in patients without additional staff or extended clinic hours.
Similarly, hospitals could experience increased pressure on emergency rooms and inpatient beds. Managing this increased demand requires careful planning and resource allocation.
Strategies for Managing Increased Patient Volume
Healthcare providers can employ several strategies to effectively manage the influx of new patients. These strategies include optimizing scheduling systems to accommodate more patients efficiently, expanding clinic hours or adding weekend or evening appointments, and investing in telehealth technologies to increase access to care. Recruiting and retaining additional staff, including physicians, nurses, and administrative personnel, will be essential.
Furthermore, streamlining administrative processes, such as electronic health records management and insurance verification, can free up valuable time for patient care. Implementing efficient referral systems to connect patients with specialists will also be crucial in managing complex cases. Finally, providers should consider partnerships with community organizations to provide wrap-around services such as transportation and social support to improve patient outcomes and reduce the burden on healthcare systems.
Potential Challenges and Corresponding Strategies
The following list Artikels some key challenges and potential strategies for healthcare providers to address the impact of Medicaid expansion:
- Challenge: Increased demand for services exceeding existing capacity.
- Strategy: Expand clinic hours, hire additional staff, utilize telehealth, optimize scheduling systems.
- Challenge: Difficulty in managing complex cases among newly insured patients.
- Strategy: Develop care coordination programs, implement efficient referral systems, invest in staff training for chronic disease management.
- Challenge: Increased administrative burden associated with managing a larger patient population.
- Strategy: Streamline administrative processes, invest in electronic health records systems, enhance billing and coding practices.
- Challenge: Potential for provider burnout due to increased workload.
- Strategy: Implement strategies to improve staff well-being, offer opportunities for professional development, and foster a supportive work environment.
Patient Experiences and Outcomes

Source: amazonaws.com
North Carolina’s Medicaid expansion is huge news, potentially impacting millions. Improving access to care means we need innovative solutions, and I was fascinated by a recent study widespread digital twins healthcare which suggests how personalized medicine could revolutionize things. This technology could be a game-changer for managing the increased patient load resulting from the expansion, making healthcare more efficient and effective for everyone.
Medicaid expansion in North Carolina promises to significantly improve the lives of many residents by increasing access to crucial healthcare services. This improved access will translate into better health outcomes, reduced disparities, and a more efficient healthcare system overall. The positive ripple effects will be felt across various aspects of patient care, from preventative screenings to the management of chronic conditions.Improved access to care is expected to lead to a substantial improvement in patient health outcomes.
With increased access to preventative care, individuals will be able to receive screenings and treatments earlier, preventing the progression of chronic diseases and reducing the severity of health problems. This proactive approach is expected to lead to a reduction in hospitalizations and emergency room visits, ultimately leading to better overall health and well-being for individuals.
Improved Health Outcomes, North carolina medicaid expansion begins
Increased access to preventative services, such as annual checkups, vaccinations, and screenings for chronic diseases like diabetes and hypertension, will allow for earlier diagnosis and treatment. This early intervention will significantly improve health outcomes, reducing the likelihood of severe complications and long-term health issues. For example, early detection of diabetes through regular screenings can help prevent the development of serious complications such as blindness, kidney failure, and heart disease.
Similarly, regular checkups can identify and address potential problems before they escalate, reducing the need for more intensive and costly treatments down the line.
Impact on Health Disparities
Medicaid expansion is expected to significantly reduce health disparities among various population groups. Historically, underserved communities have faced significant barriers to accessing healthcare, leading to poorer health outcomes compared to their more affluent counterparts. Increased coverage will help address these inequities by ensuring that all individuals, regardless of their socioeconomic status, have access to the necessary care. This will likely lead to a reduction in the disparity in rates of chronic diseases and improved overall health for these previously underserved populations.
For instance, we might see a decrease in the difference in diabetes management rates between low-income and higher-income individuals.
Reduction in Preventable Hospitalizations and Emergency Room Visits
Increased access to primary and preventative care will lead to a substantial reduction in preventable hospitalizations and emergency room visits. Many hospitalizations and ER visits are a result of untreated or poorly managed chronic conditions. With expanded Medicaid coverage, individuals will be able to receive the necessary ongoing care to manage these conditions, preventing acute episodes that require emergency intervention.
This translates to both improved patient outcomes and significant cost savings for the healthcare system as a whole. A study in another state that expanded Medicaid showed a 15% reduction in preventable hospitalizations within the first two years.
Pre- and Post-Expansion Health Indicators
| Metric | Pre-Expansion | Post-Expansion (Projected) |
|---|---|---|
| Uninsured Rate | 10% (Example) | 6% (Projected) |
| Chronic Disease Management (Diabetes Control – A1C levels <7%) | 50% (Example) | 60% (Projected) |
| Preventative Care Utilization (Annual Checkups) | 40% (Example) | 65% (Projected) |
| Preventable Hospitalizations (per 1000 population) | 25 (Example) | 18 (Projected) |
Political and Social Context: North Carolina Medicaid Expansion Begins
The expansion of Medicaid in North Carolina was a long and arduous process, deeply intertwined with the state’s political landscape and the passionate advocacy of various groups. The debate highlighted fundamental disagreements about the role of government in healthcare, economic priorities, and the best way to serve the state’s most vulnerable citizens.The political debate surrounding Medicaid expansion in North Carolina was characterized by a significant partisan divide.
For years, Republican leadership resisted expansion, citing concerns about the cost to taxpayers and the potential impact on the state budget. They often emphasized the importance of fiscal responsibility and argued that alternative approaches to healthcare access were preferable. Conversely, Democrats strongly advocated for expansion, emphasizing the potential benefits for the uninsured population, the positive economic impact on the state, and the moral imperative to provide healthcare access to all citizens.
This partisan divide created a significant obstacle to achieving consensus and enacting expansion legislation.
The Role of Advocacy Groups
Numerous advocacy groups played a crucial role in pushing for Medicaid expansion in North Carolina. Organizations such as the North Carolina Justice Center, the NC Child, and various healthcare provider associations worked tirelessly to educate the public, lobby legislators, and build a broad coalition in support of expansion. They utilized various strategies, including grassroots mobilization, public awareness campaigns, and direct engagement with lawmakers.
North Carolina’s Medicaid expansion is great news, boosting access to healthcare for many. This increased demand is likely to benefit major players like Walgreens, who, as reported in this article about their recent summit acquisition, walgreens raises healthcare segment outlook summit acquisition , are already seeing a positive impact on their healthcare segment. This growth underscores the ripple effects of expanded access, ultimately benefiting both patients and healthcare providers across the state.
These groups provided vital information and research to counter arguments against expansion and successfully built public support for the initiative. Their persistence in the face of significant political opposition was instrumental in ultimately achieving success.
Public Perception of Medicaid Expansion
Before implementation, public opinion on Medicaid expansion in North Carolina was divided, reflecting the polarized political climate. Polls showed varying levels of support, with significant differences across partisan lines. Many opponents expressed concerns about increased taxes and government spending. Proponents, on the other hand, highlighted the potential health benefits for uninsured individuals and the positive economic impact on the state.Following implementation, public perception shifted somewhat.
While some initial concerns about cost remained, the positive impacts on access to care and health outcomes began to become more evident. This shift was influenced by successful advocacy campaigns that highlighted real-life stories of individuals who benefited from expanded coverage. Increased awareness of the program’s positive effects gradually increased public support, although a significant portion of the population continued to hold reservations.
A Visual Representation of Stakeholders
Imagine a circular diagram, representing the diverse stakeholders involved in the Medicaid expansion debate. At the center is a large circle representing the North Carolina population, depicted in neutral colors. Radiating outwards are several smaller circles, each representing a key stakeholder group. Groups supporting expansion, such as the NC Justice Center and healthcare providers, are represented by circles in shades of green, symbolizing growth and health.
These circles are connected to the central population circle by thick, positive lines. Groups opposing expansion, such as some fiscal conservative organizations, are represented by circles in shades of red, signifying caution and financial constraint. These are connected to the central circle by thinner, less prominent lines. The size of each circle reflects the relative influence of each stakeholder group, with larger circles representing more influential groups.
Finally, the legislature is represented by a central hexagon, bridging the gap between supporting and opposing groups, illustrating its role in navigating the debate and ultimately enacting the legislation. The overall visual design would emphasize the interconnectedness of these groups and the dynamic nature of the debate.
Last Recap
The launch of North Carolina’s Medicaid expansion marks a pivotal moment for the state’s healthcare system. While challenges undoubtedly exist, the potential for improved access to care, better health outcomes, and a stronger economy is undeniable. The coming years will be crucial in monitoring the effects of this expansion, learning from its successes and addressing its challenges to ensure its long-term effectiveness and positive impact on the lives of North Carolinians.
Key Questions Answered
What specific services will be covered under the expansion?
The specific services covered will largely align with standard Medicaid benefits, including doctor visits, hospital care, prescription drugs, and preventative care. Details are available on the NC Medicaid website.
How can I apply for Medicaid coverage under the expansion?
Application information and assistance can be found on the NC Medicaid website, or through local health departments and community organizations. Many resources offer assistance with the application process.
What are the income limits for eligibility under the expansion?
Income limits are set by federal guidelines and are adjusted periodically. Check the NC Medicaid website for the most up-to-date information on eligibility requirements.
Will this expansion affect my taxes?
The expansion’s impact on taxes is complex and depends on various factors, including the state’s funding mechanisms and federal contributions. The long-term effects are still being assessed.