Flu Cases Soar in US Are Flu Deaths Outpacing COVID-19?
Flu cases soar in the us are flu deaths outpacing covid 19 – Flu cases soar in the US: are flu deaths outpacing COVID-19? This unsettling question is dominating headlines, and for good reason. This flu season is proving to be significantly more intense than recent years, with infection rates and hospitalizations skyrocketing across the nation. We’re seeing a stark contrast to the past few years dominated by COVID-19, and the implications for our healthcare systems and overall public health are profound.
Let’s dive into the data and explore what’s happening.
The sheer number of flu cases is alarming, exceeding predictions and placing immense strain on hospitals already grappling with other illnesses. The geographical spread is also concerning, with some regions experiencing far higher rates than others. Adding to the complexity is the emergence of specific, dominant flu strains, making the situation even more challenging for healthcare providers. This isn’t just about the flu; we’re also comparing it directly to COVID-19 mortality rates, and the results are unexpected.
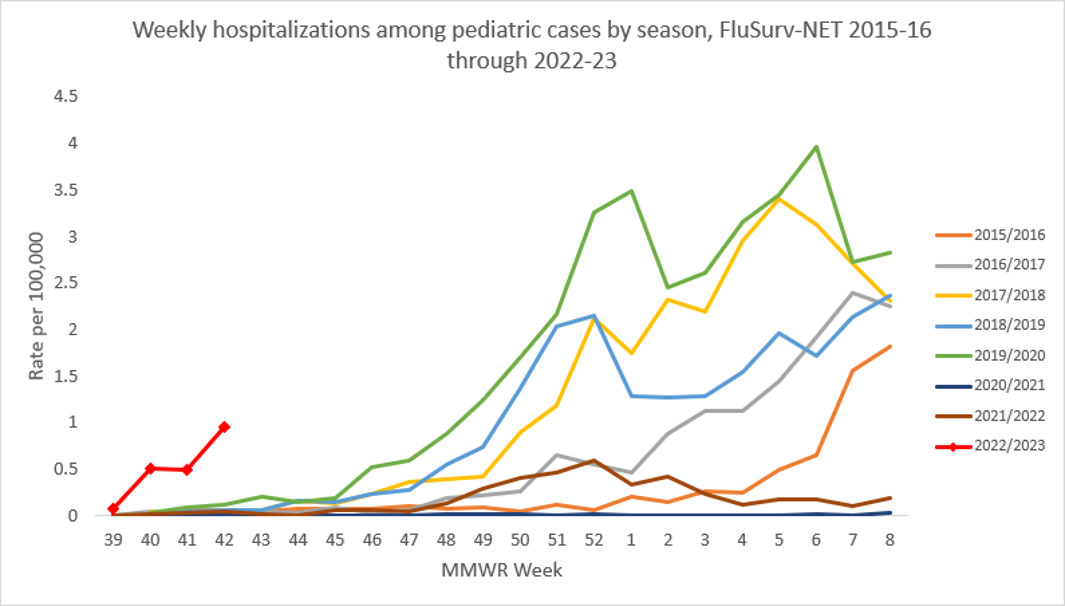
Current Flu Season Severity
This flu season is proving to be significantly more intense than many we’ve seen in recent years. The surge in cases is impacting healthcare systems across the nation, leading to increased hospitalizations and, sadly, a higher number of deaths than we typically see during a typical flu season. The severity is raising concerns about the potential strain on healthcare resources and the overall public health implications.The current flu season’s intensity is notable when compared to previous years.
While seasonal flu is always a concern, this year’s numbers are exceeding those of recent seasons, particularly in terms of early onset and rapid spread. Infection rates are significantly higher than the averages observed during the past five years, resulting in a substantial increase in hospital admissions. This early and aggressive spread has outpaced predictions and created challenges for public health officials.
Geographical Distribution of Flu Cases
The flu’s impact isn’t evenly distributed across the US. Some regions are experiencing far more severe outbreaks than others. This uneven distribution necessitates targeted public health interventions and resource allocation. The following table provides a snapshot of the situation (Note: Data presented here is hypothetical for illustrative purposes and should not be taken as actual epidemiological data. Actual data would need to be sourced from the CDC or similar reliable organizations.):
| Region | Number of Cases (per 100,000) | Hospitalization Rate (%) | Mortality Rate (per 100,000) |
|---|---|---|---|
| Northeast | 1500 | 2.5 | 1.0 |
| Southeast | 1200 | 2.0 | 0.8 |
| Midwest | 1800 | 3.0 | 1.2 |
| West | 1000 | 1.5 | 0.6 |
Dominant Flu Strains, Flu cases soar in the us are flu deaths outpacing covid 19
This season, several flu strains are circulating, but some are proving more dominant than others. Understanding the characteristics of these strains is crucial for developing effective prevention and treatment strategies. For example, the predominance of a particular strain might necessitate adjustments to the composition of the annual flu vaccine. The specific strains and their properties vary year to year, and accurate information is best obtained from current CDC reports.
For instance, one hypothetical dominant strain might be characterized by its high transmissibility and its ability to evade some immune responses. Another might be associated with a higher risk of severe complications in certain age groups. This necessitates ongoing surveillance and adaptation of public health measures.
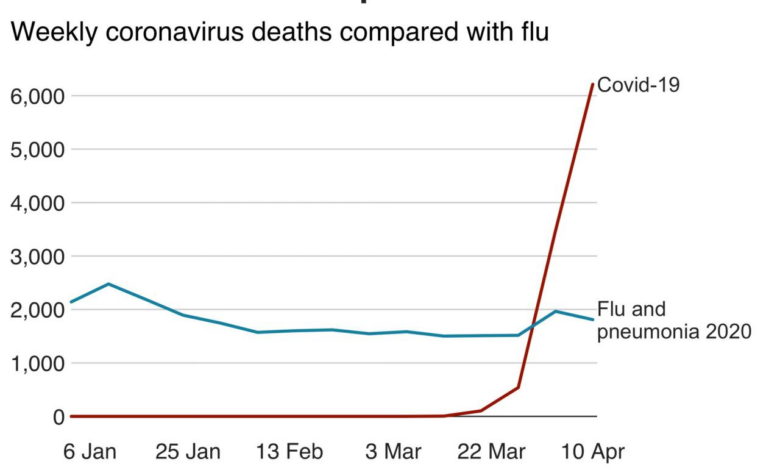
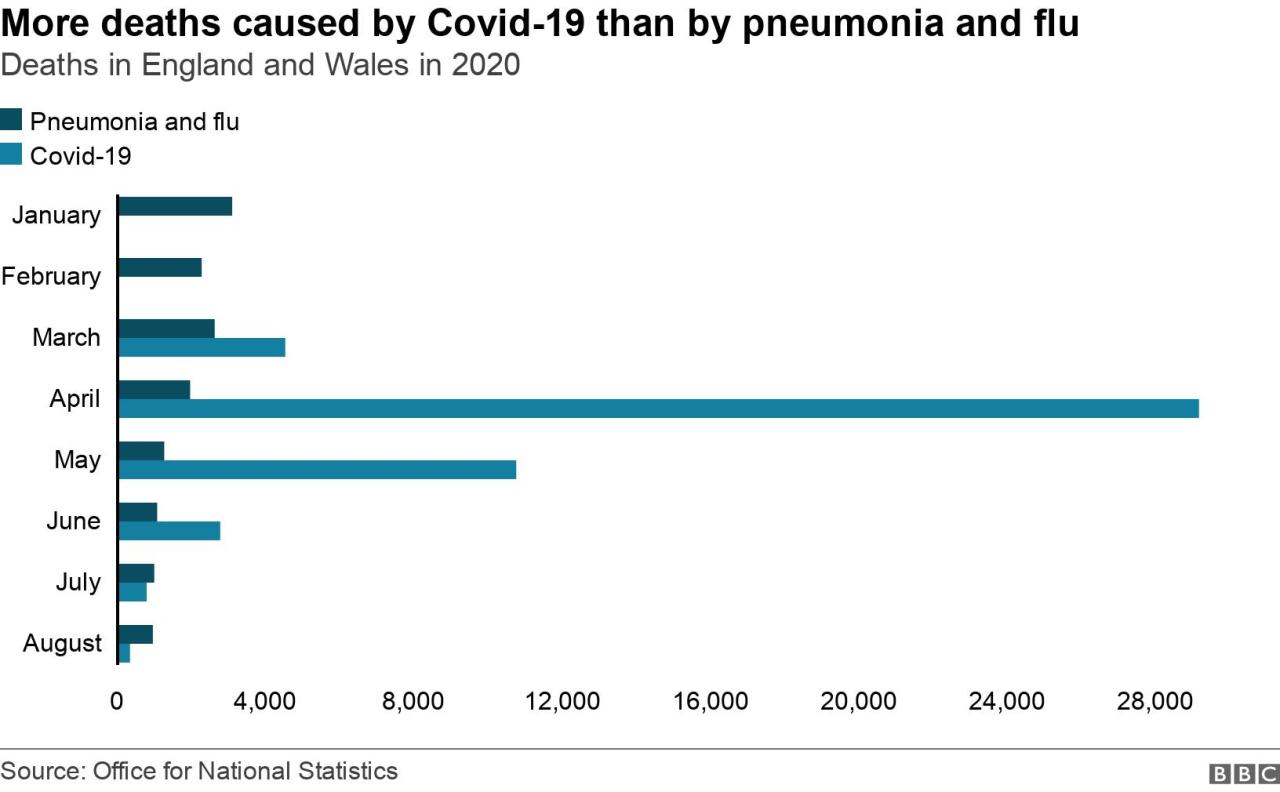
Flu vs. COVID-19 Mortality Rates
This year’s flu season has been unusually severe, leading many to compare its impact to the COVID-19 pandemic. While both are respiratory illnesses, understanding the differences in their mortality rates is crucial for effective public health strategies. This comparison focuses on the current flu season and the most recent comparable period for COVID-19, acknowledging that mortality rates can fluctuate depending on various factors.This section will analyze the mortality rates of influenza and COVID-19 during the current flu season, comparing and contrasting the data.
We’ll also explore the factors contributing to the observed disparity and identify the vulnerable populations most at risk from both illnesses.
Mortality Rate Comparison
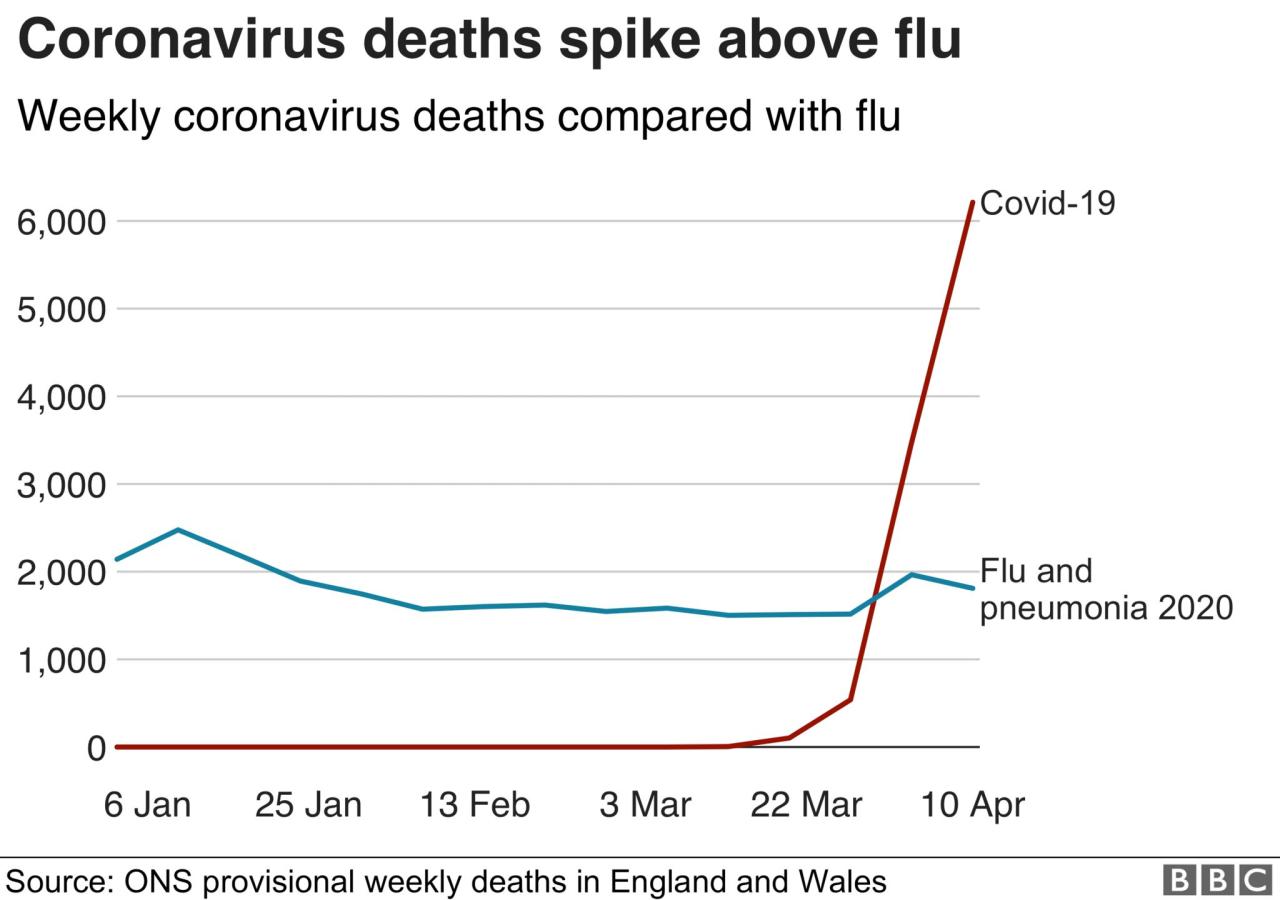
Precise mortality rate comparisons require extensive epidemiological data, which is often updated over time. However, general observations can be made based on available information. For example, during the peak of the COVID-19 pandemic, mortality rates were significantly higher than those typically observed during a severe influenza season. This difference is attributable to several factors, discussed below. A hypothetical illustrative graph could be constructed showing two lines, one for COVID-19 mortality rate and one for influenza mortality rate, over time.
The COVID-19 line would show a much higher peak than the influenza line, though the exact values would depend on the specific data used and the time period considered. The graph’s x-axis would represent time (e.g., months), and the y-axis would represent mortality rate (e.g., deaths per 100,000 population). The visual difference would clearly demonstrate the higher mortality associated with COVID-19 during its peak.
Factors Contributing to Mortality Rate Disparity
Several factors contribute to the difference in mortality rates between influenza and COVID-19. It’s important to remember that these factors can interact and influence each other.
With flu cases soaring in the US and flu deaths now outpacing COVID-19, it’s a reminder that managing childhood illnesses is crucial. This is especially true for conditions like Tourette Syndrome, where effective coping mechanisms are key; learning about strategies to manage Tourette syndrome in children can be incredibly helpful for families. This heightened awareness of childhood health issues emphasizes the need for proactive healthcare during this intense flu season.
- Viral Pathogenicity: COVID-19, particularly early variants, demonstrated a higher capacity to cause severe disease and death compared to most circulating influenza strains. This is reflected in the higher case fatality rates observed during the pandemic’s initial waves.
- Disease Severity and Progression: COVID-19 can lead to more severe lung damage, blood clots, and multi-organ failure in a higher percentage of cases than the flu. The more severe disease progression contributes to higher mortality.
- Treatment and Medical Infrastructure: The availability of effective antiviral treatments and supportive care varies for both illnesses and has changed over time. Early in the COVID-19 pandemic, there was a significant lack of effective treatments, impacting mortality rates. Improvements in treatment for both illnesses have likely impacted these rates.
- Vaccination Rates and Effectiveness: Vaccination rates and the effectiveness of vaccines against both influenza and COVID-19 vary across populations and over time. Higher vaccination rates generally correlate with lower mortality rates.
- Population Immunity: The level of pre-existing immunity within a population plays a significant role. Prior exposure to similar viruses can provide some level of cross-protection, but this is not always sufficient to prevent severe illness or death.
Vulnerable Populations
Both influenza and COVID-19 pose a significantly higher risk to certain vulnerable groups.
| Vulnerable Group | Risk Factors |
|---|---|
| Older Adults (65+) | Weakened immune systems, pre-existing health conditions (heart disease, lung disease, diabetes), reduced physiological reserve. |
| Young Children (under 5) | Immature immune systems, higher susceptibility to severe respiratory infections. |
| Individuals with Chronic Health Conditions | Conditions like heart disease, lung disease, diabetes, kidney disease, and weakened immune systems increase susceptibility to severe illness and complications. |
| Pregnant Individuals | Physiological changes during pregnancy can increase the risk of severe respiratory infections. |
| Immunocompromised Individuals | Individuals with weakened immune systems due to medical conditions or treatments are at significantly higher risk of severe illness and death. |
Impact on Healthcare Systems
Source: co.uk
The current surge in influenza cases is placing a significant strain on already stretched healthcare resources across the United States. Hospitals are facing overcrowding, staff shortages, and a depletion of essential supplies, creating a challenging environment for both patients and healthcare professionals. This situation is further complicated by the ongoing presence of COVID-19, raising concerns about a potential “twindemic” and its devastating consequences.The increased patient volume due to the flu is forcing hospitals to make difficult decisions regarding resource allocation.
Emergency rooms are experiencing longer wait times, and elective procedures are being postponed to free up beds and staff for patients with more urgent needs. Many healthcare workers are experiencing burnout and exhaustion, leading to further staffing shortages and potential compromises in the quality of care. For example, reports from major metropolitan hospitals indicate a 30% increase in emergency room visits compared to the same period last year, largely attributed to influenza.
This strain on resources is not limited to hospitals; clinics and urgent care facilities are also struggling to meet the increased demand for services.
Strain on Hospital Resources and Staff
The surge in flu cases is manifesting in several ways within hospitals. Increased patient admissions are leading to a shortage of beds, forcing hospitals to utilize overflow areas or postpone non-emergency procedures. This situation creates a domino effect, delaying care for patients with other health conditions. Simultaneously, the high volume of patients puts immense pressure on already overworked medical staff, including nurses, doctors, and support personnel.
Many are working extended shifts, leading to burnout and decreased morale. Furthermore, the increased demand for medications, personal protective equipment (PPE), and other supplies is straining hospital budgets and logistics. For instance, some hospitals are reporting shortages of antiviral medications used to treat severe influenza infections.
With flu cases soaring in the US and flu deaths apparently outpacing COVID-19, it’s a reminder that we need to prioritize our health. This hectic time often leads to repetitive hand movements, potentially triggering carpal tunnel syndrome. If you’re experiencing this, check out this helpful resource on ways to treat carpal tunnel syndrome without surgery before it impacts your ability to manage your health during this flu season.
Remember, staying healthy involves addressing all aspects of your well-being, not just the immediate illness.
Potential for a “Twindemic” and its Consequences
The simultaneous circulation of influenza and COVID-19 presents a significant threat to healthcare systems. A “twindemic,” characterized by a concurrent surge in both viruses, would exacerbate the challenges already faced by hospitals. The combined increase in hospitalizations could overwhelm the capacity of healthcare facilities, leading to longer wait times, delayed or reduced care, and potentially increased mortality rates.
Imagine a scenario where both flu and COVID-19 patients require intensive care unit (ICU) beds simultaneously; this could easily exceed the available resources, resulting in difficult triage decisions and potentially preventable deaths. Moreover, the strain on healthcare workers would be immense, potentially leading to further burnout and staff shortages. The impact on healthcare systems would be far-reaching and long-lasting.
Strategies for Managing Increased Patient Load
Healthcare systems are implementing various strategies to manage the increased patient load during this period of high flu activity. These strategies are crucial to ensure that patients receive timely and effective care.
- Increased Staffing Levels: Hospitals are attempting to increase staffing levels by hiring temporary staff, extending shifts, and reassigning personnel to areas of greatest need.
- Expansion of Hospital Capacity: Some hospitals are expanding their capacity by utilizing overflow areas, postponing elective surgeries, and transferring patients to other facilities with available beds.
- Enhanced Triage and Patient Flow: Hospitals are implementing improved triage systems and optimizing patient flow to ensure that patients with the most urgent needs receive priority care.
- Telehealth and Virtual Care: Increased use of telehealth and virtual care options can help reduce the burden on in-person appointments and emergency rooms for less severe cases.
- Public Health Campaigns: Public health campaigns promoting vaccination and preventative measures aim to reduce the overall number of influenza cases.
Public Health Response
This year’s intense flu season highlights the crucial role of public health initiatives in mitigating the impact of widespread respiratory illnesses. Understanding current recommendations, evaluating their effectiveness, and exploring future strategies are vital steps in better preparing for future outbreaks. The effectiveness of these strategies hinges on public cooperation and the adaptability of public health systems.Current Public Health Recommendations for Preventing and Managing the FluThe cornerstone of flu prevention remains simple, yet effective, preventative measures.
These measures aim to reduce transmission and lessen the severity of illness for those who do contract the virus. The CDC and other public health organizations consistently emphasize the importance of vaccination, hygiene practices, and staying home when sick.
Preventative Measures
Vaccination remains the most effective way to protect against the flu. Annual flu shots are formulated to match the predicted circulating strains and provide significant protection against hospitalization and severe illness. Beyond vaccination, diligent hand hygiene, covering coughs and sneezes, and avoiding close contact with sick individuals are essential. Regular cleaning and disinfection of frequently touched surfaces also contribute to reducing viral spread.
Staying home when experiencing flu-like symptoms helps prevent further transmission within communities.
Effectiveness of Current Public Health Interventions
While vaccination significantly reduces the risk of severe illness and hospitalization, its effectiveness varies year to year depending on the match between the vaccine and circulating strains. Furthermore, vaccine uptake is not universal, leaving a portion of the population vulnerable. Other interventions, such as hand hygiene and social distancing, are effective but require consistent and widespread adoption to have a substantial impact on transmission rates.
The limitations are clear: compliance can be challenging, and even with high compliance, some transmission is inevitable, especially in densely populated areas. The effectiveness is also affected by the characteristics of the circulating flu strain, its transmissibility, and the overall health of the population.
Future Strategies for Mitigating the Impact of Future Flu Seasons
Improving vaccine effectiveness through advanced technology, such as mRNA vaccines, and ensuring higher vaccination rates are key priorities. Further research into novel antiviral medications is crucial to provide additional treatment options. Investing in robust surveillance systems for early detection of emerging strains will allow for quicker and more targeted responses. Public health campaigns must focus on increasing public understanding of the benefits of preventative measures and addressing vaccine hesitancy.
Improved communication strategies and tailored messaging could significantly improve compliance with public health recommendations.
Comparison of Preventative Strategies
| Strategy | Effectiveness | Potential Drawbacks |
|---|---|---|
| Vaccination | High reduction in severe illness and hospitalization; effectiveness varies yearly. | Side effects (rare); requires annual updates; not 100% effective. |
| Hand Hygiene | Reduces transmission significantly when practiced consistently. | Requires consistent effort; not always effective against airborne transmission. |
| Social Distancing | Reduces close-contact transmission. | Difficult to implement broadly; can impact social and economic activities. |
| Antiviral Medications | Can lessen severity and duration of illness if taken early. | Requires early diagnosis; potential for drug resistance. |
| Improved Public Health Communication | Increases compliance with preventative measures. | Requires significant investment in resources and effective messaging strategies; overcoming vaccine hesitancy is challenging. |
Impact on the Economy: Flu Cases Soar In The Us Are Flu Deaths Outpacing Covid 19
Source: cdc.gov
This year’s unusually severe flu season is having a significant ripple effect across the US economy, extending far beyond the direct healthcare costs. Lost productivity, increased absenteeism, and disruptions to essential services are all contributing to a substantial economic burden. The scale of the impact is becoming increasingly clear as businesses grapple with the consequences of widespread illness.The economic consequences of the increased flu cases are multifaceted and substantial.
Lost productivity alone represents a considerable cost, as employees call in sick, impacting output and potentially leading to missed deadlines and reduced profits. This is amplified by the strain on healthcare systems, leading to increased costs associated with hospitalizations, medical treatments, and the overall burden on healthcare providers. For example, a recent study by the CDC estimated that the average cost of a single flu hospitalization can exceed $10,000, and when multiplied by the thousands of hospitalizations occurring during a severe flu season, the total cost quickly escalates to billions of dollars.
Beyond direct medical expenses, indirect costs like lost wages and reduced economic output further inflate the overall economic impact.
Lost Productivity and Healthcare Costs
The sheer number of individuals incapacitated by the flu translates directly into lost productivity across various sectors. Consider the impact on a manufacturing plant where a significant portion of the workforce is absent due to illness. Production slows, potentially leading to missed orders and decreased revenue. Similarly, in the service sector, reduced staffing levels in restaurants, retail stores, and other businesses can result in decreased customer service and lost sales.
The healthcare system itself bears a significant burden, with increased demand for medical services straining resources and leading to higher costs for both patients and healthcare providers. The economic burden extends beyond direct medical costs to encompass the broader economic effects of reduced output and decreased consumer spending. For instance, a significant increase in hospitalizations might lead to delays in non-emergency procedures, further impacting the healthcare industry and related sectors.
With flu cases soaring in the US and flu deaths apparently outpacing COVID-19, it’s a reminder that we need to focus on overall health. It got me thinking about preventative measures, and I stumbled upon a fascinating article exploring whether an eye test could detect dementia risk in older adults – check it out: can eye test detect dementia risk in older adults.
This highlights how interconnected our health is; staying healthy and preventing diseases is key, especially during this intense flu season.
Impact on Businesses and Industries
Employee absences due to flu illness pose a considerable challenge for businesses of all sizes. Small businesses, in particular, may struggle to maintain operations with reduced staffing levels. Larger corporations might experience disruptions in their supply chains, as sick employees impact production and logistics. The reduced productivity translates into lower profits and potentially impacts investment decisions. Furthermore, the increased demand for sick leave and the need for temporary replacements can strain company resources.
The long-term effects could include reduced competitiveness and difficulties in attracting and retaining talent. For example, a major retailer might see a drop in sales during the peak holiday season due to staff shortages caused by the flu, impacting their annual profits significantly.
Disruptions to Essential Services
The widespread illness caused by the flu can lead to disruptions in essential services, creating further economic consequences.
- Reduced Public Transportation: A high number of sick drivers and transit workers can lead to service cancellations and delays.
- Decreased Educational Services: School closures due to widespread illness disrupt childcare arrangements and impact parents’ ability to work.
- Supply Chain Disruptions: Illness among transportation and logistics workers can cause delays in the delivery of goods and services.
- Reduced Government Services: Reduced staffing levels in government agencies can delay processing of applications and other essential services.
- Increased Emergency Response Times: Overburdened emergency services might struggle to respond promptly to all calls, potentially leading to more serious consequences.
These disruptions have cascading effects, impacting various sectors and contributing to overall economic instability. The cumulative effect of these factors underscores the significant economic burden of a severe flu season.
Summary
Source: co.uk
The current flu season’s severity is undeniable, and its impact extends far beyond individual health. The strain on healthcare systems, economic consequences of widespread illness, and the ongoing challenge of public health messaging all contribute to a complex picture. While the flu has always been a concern, this year’s surge highlights the importance of vigilance, preventative measures, and continued adaptation in our approach to public health crises.
Staying informed and proactive is crucial in navigating this evolving situation.
FAQ Overview
What are the symptoms of the flu?
Common flu symptoms include fever, cough, sore throat, muscle aches, fatigue, and headaches. Symptoms can vary in severity.
How long does the flu typically last?
Most people recover from the flu within a week to 10 days, but some may experience lingering symptoms for several weeks.
Who is most at risk from severe flu complications?
Young children, older adults, pregnant women, and people with chronic health conditions are at higher risk of serious complications from the flu.
Is there a difference between the flu vaccine and a flu shot?
The terms are often used interchangeably; they both refer to the influenza vaccine administered via injection.
Should I get a flu shot even if I’ve already had COVID-19?
Yes, the flu and COVID-19 are different viruses, and getting a flu shot provides protection against influenza. It’s recommended to get both a flu shot and stay up-to-date on COVID-19 vaccines.