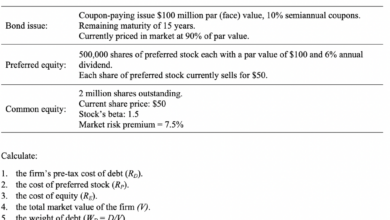
Compliantly Supercharge Your Hospitals Bottom Line
Compliantly supercharge your hospitals bottom line – Compliantly Supercharge Your Hospital’s Bottom Line: It sounds ambitious, right? But boosting your hospital’s profitability isn’t just about cutting costs; it’s about strategic growth, improved patient care, and smart investments. This isn’t about sacrificing quality – it’s about optimizing every aspect of your hospital’s operations to maximize efficiency and, ultimately, improve the lives of your patients and the financial health of your institution.
We’ll explore practical strategies, from streamlining processes and enhancing revenue cycle management to forging strategic partnerships and developing innovative revenue streams. Let’s dive in!
This post is your roadmap to navigating the complexities of healthcare finance and discovering how to sustainably improve your hospital’s bottom line without compromising ethical practices or patient care. We’ll cover everything from optimizing resource allocation and improving patient satisfaction to exploring new revenue streams and ensuring strict regulatory compliance. Get ready to learn how to make your hospital not just profitable, but thriving.
Improving Hospital Efficiency
Boosting a hospital’s bottom line isn’t just about increasing revenue; it’s equally, if not more, about controlling costs and maximizing the efficiency of existing resources. Streamlining operations, optimizing resource allocation, and leveraging technology are key strategies to achieve significant improvements in profitability. This involves a holistic approach, impacting everything from patient flow to administrative processes.
Innovative Strategies to Streamline Hospital Operations
Implementing innovative strategies is crucial for reducing operational costs and improving patient care. Three particularly effective strategies are robotic process automation (RPA), lean methodologies, and predictive analytics. RPA automates repetitive administrative tasks, freeing up staff for more patient-focused work. For example, RPA can automate appointment scheduling, insurance verification, and medical record processing, significantly reducing administrative overhead and human error.
Boosting your hospital’s bottom line ethically requires smart investments. One area ripe for exploration is early detection of conditions like dementia, which can significantly impact long-term care costs. A recent study explored whether a simple eye test could help, check out this fascinating article on whether can eye test detect dementia risk in older adults and how that could lead to proactive interventions.
Early diagnosis translates to better resource allocation, ultimately improving efficiency and your hospital’s financial health.
Lean methodologies focus on eliminating waste in all aspects of hospital operations, from supply chain management to patient flow. This could involve implementing a Kanban system to manage inventory, optimizing patient pathways to reduce wait times, or redesigning workflows to eliminate unnecessary steps. Predictive analytics uses data to anticipate potential problems and proactively address them. This could involve predicting patient readmissions based on historical data, optimizing staffing levels based on anticipated patient volume, or identifying potential equipment failures before they occur.
These predictive capabilities lead to significant cost savings by preventing problems before they escalate.
Optimizing Hospital Resource Allocation
Effective resource allocation is vital for efficient hospital operations. This encompasses the strategic deployment of staff, equipment, and supplies to maximize their utilization and minimize waste. Optimizing staff allocation involves using workforce management software to predict staffing needs based on patient volume and acuity. This ensures adequate staffing levels during peak times while avoiding overstaffing during slower periods.
Equipment optimization involves using a centralized equipment management system to track equipment location, maintenance schedules, and utilization rates. This allows for better maintenance planning, preventing costly downtime and ensuring that equipment is used efficiently. Supply chain optimization involves implementing inventory management systems to track supply levels, predict demand, and minimize waste. This could involve implementing just-in-time inventory management to reduce storage costs and prevent expiration of perishable supplies.
Effective resource allocation ensures that resources are used effectively, minimizing waste and maximizing their impact.
Leveraging Technology to Enhance Efficiency
Technology plays a pivotal role in enhancing hospital efficiency and reducing administrative overhead. Electronic health records (EHRs) are a prime example, providing a centralized, digital repository for patient information, eliminating the need for paper charts and improving information accessibility. This reduces administrative workload, improves care coordination, and minimizes medical errors. Telemedicine offers another avenue for efficiency gains, allowing for remote consultations and monitoring of patients, reducing the need for in-person visits and improving access to care, especially for patients in rural areas.
Furthermore, the use of hospital information systems (HIS) provides a comprehensive view of hospital operations, facilitating better decision-making and resource allocation. These systems integrate various hospital departments, allowing for real-time monitoring of key performance indicators (KPIs) and enabling proactive identification and resolution of operational bottlenecks. The adoption of such technology leads to improved patient outcomes, reduced costs, and increased overall efficiency.
Comparison of Hospital Management Systems
Different hospital management systems offer varying functionalities and impact on profitability. A cloud-based system, for instance, offers scalability and accessibility, reducing the need for significant upfront investment in IT infrastructure. However, reliance on internet connectivity might pose a challenge during outages. On-premise systems offer greater control and security but require substantial investment in hardware and IT personnel.
Integrated systems that combine EHRs, HIS, and other hospital applications offer streamlined workflows and improved data integration, leading to enhanced efficiency and reduced administrative overhead. However, the initial implementation cost and complexity of such systems can be high. The choice of a hospital management system should be based on a thorough assessment of the hospital’s specific needs, budget, and technical capabilities.
Factors like scalability, security, ease of use, and integration capabilities should be carefully considered to ensure the chosen system aligns with the hospital’s long-term goals and contributes to improved profitability.
Enhancing Revenue Cycle Management
Optimizing your hospital’s revenue cycle is crucial for financial health and sustainability. A streamlined and efficient revenue cycle directly impacts your bottom line, ensuring timely reimbursements and minimizing losses from denials and delays. This section explores strategies to supercharge your hospital’s revenue cycle management, focusing on accelerating payments, minimizing denials, and ensuring accurate billing and coding.
Accelerating Payments from Insurance Providers and Patients
Prompt payment is the lifeblood of a healthy revenue cycle. Strategies to achieve this involve leveraging technology and improving communication. Implementing automated payment posting systems reduces manual errors and speeds up processing. Establishing clear and consistent communication channels with both insurers and patients, including online portals and automated reminders, ensures timely payments and reduces outstanding balances. Negotiating shorter payment terms with insurance providers, based on your hospital’s volume and payment history, can also significantly improve cash flow.
For example, a hospital could negotiate a 30-day payment cycle instead of the standard 60-day cycle, freeing up significant capital.
Minimizing Denials and Appeals in the Revenue Cycle
Denials and appeals represent significant revenue loss. A proactive approach is key to minimizing these. This involves rigorous pre-authorization processes to ensure services are covered before they are provided. Investing in robust claims scrubbing software to identify and correct coding errors before submission dramatically reduces the likelihood of denials. Regular audits of claims data to identify patterns of denials can highlight areas needing improvement in coding practices or pre-authorization procedures.
For instance, if a significant number of denials relate to a specific procedure code, a review of that code’s documentation and billing practices is warranted. A well-defined appeals process, with designated personnel responsible for handling denials and appeals, is also crucial. This process should include tracking denial reasons, preparing effective appeals, and monitoring their outcomes.
Best Practices for Accurate and Timely Billing and Coding
Accurate and timely billing and coding are fundamental to a successful revenue cycle. This requires ongoing staff training on the latest coding guidelines and regulatory changes. Implementing electronic health records (EHR) systems with integrated billing and coding functionalities streamlines the process and minimizes errors. Regularly reviewing and updating coding and billing procedures ensures compliance with evolving regulations.
Cross-checking data between the EHR system and the billing system helps identify discrepancies and prevent errors. For example, ensuring accurate capture of patient demographics and insurance information is crucial to avoid delays and denials. Implementing a robust charge capture system, with mechanisms to prevent missed charges, also improves revenue capture.
Implementing a Robust Revenue Cycle Management System: A Step-by-Step Guide
Implementing a robust system involves a phased approach. First, conduct a thorough assessment of the current revenue cycle to identify bottlenecks and areas for improvement. This involves analyzing key performance indicators (KPIs) such as days in accounts receivable (A/R), denial rates, and collection rates. Next, develop a comprehensive plan outlining specific goals and timelines. This plan should include strategies for improving each stage of the revenue cycle, from pre-registration to payment posting.
Third, invest in technology to automate processes and improve efficiency. This could involve implementing new software for claims processing, payment posting, or denial management. Fourth, provide comprehensive training to staff on the new systems and processes. Fifth, monitor key performance indicators (KPIs) regularly to track progress and make adjustments as needed. Sixth, establish a system for continuous improvement, regularly reviewing and updating processes to optimize efficiency and revenue capture.
This iterative approach ensures the system remains effective and adaptable to changing circumstances.
Optimizing Patient Care and Satisfaction
Improving patient care isn’t just ethically sound; it’s a powerful lever for boosting a hospital’s bottom line. Higher patient satisfaction translates directly into increased revenue, improved operational efficiency, and a stronger reputation within the community. This section explores the direct link between exceptional patient care and hospital profitability.
Improved Patient Care’s Impact on Hospital Profitability
Positive patient experiences lead to improved hospital financial performance in several ways. Firstly, satisfied patients are more likely to recommend the hospital to others, generating organic referrals and reducing marketing costs. Secondly, positive word-of-mouth and online reviews enhance the hospital’s reputation, attracting more patients and potentially commanding higher prices. Finally, a culture of excellent patient care fosters a more engaged and motivated staff, leading to reduced turnover and associated recruitment costs.
Conversely, negative experiences can lead to patient complaints, lawsuits, and reputational damage, all of which significantly impact profitability.
Correlation Between Patient Satisfaction Scores and Hospital Revenue
Numerous studies have demonstrated a strong correlation between higher patient satisfaction scores and increased hospital revenue. For example, a study published in theJournal of Healthcare Management* found that hospitals in the top quartile of patient satisfaction scores experienced a significantly higher net revenue per admission compared to those in the bottom quartile. This isn’t simply correlation; improved patient experiences often lead to better health outcomes, reducing the length of stay and the need for costly readmissions.
Examples of Patient-Centered Care Models Improving Financial Outcomes
Several patient-centered care models have proven successful in improving both patient satisfaction and financial outcomes. One example is the implementation of patient portals, which allow patients to access their medical records, schedule appointments, and communicate with their healthcare providers online. This improves convenience and engagement, leading to increased satisfaction and potentially reduced no-show rates. Another example is the use of care coordination programs, which ensure patients receive seamless care across different healthcare settings.
This reduces fragmentation of care, improves patient outcomes, and minimizes costly hospital readmissions. Finally, incorporating patient preferences and values into treatment plans demonstrates respect and empowers patients, boosting their satisfaction and potentially leading to better adherence to treatment plans, resulting in improved outcomes and reduced costs.
Strategies to Reduce Hospital Readmission Rates and Improve Patient Outcomes
Reducing hospital readmission rates is crucial for improving both patient outcomes and hospital finances. Strategies include implementing robust discharge planning processes, providing comprehensive patient education, ensuring patients have access to necessary post-discharge support services, and actively engaging patients and their families in their care. For instance, a post-discharge phone call to check on a patient’s well-being can identify potential problems early, preventing unnecessary readmissions.
Furthermore, proactively addressing social determinants of health, such as housing instability and food insecurity, can significantly impact patient outcomes and reduce readmissions.
Patient Engagement Strategies and Cost-Benefit Analysis
The following table compares different patient engagement strategies and their potential cost-benefit impact. Note that the figures are illustrative and can vary significantly depending on the specific hospital and implementation.
| Strategy | Implementation Cost | Patient Satisfaction Improvement (estimated percentage points) | Revenue Impact (estimated) |
|---|---|---|---|
| Patient Portal Implementation | $50,000 – $100,000 | 5-10% | Increased patient volume, reduced administrative costs, potentially $200,000 – $500,000 annual increase in revenue |
| Care Coordination Program | $100,000 – $250,000 | 10-15% | Reduced readmission rates, improved patient outcomes, potentially $300,000 – $750,000 annual increase in revenue |
| Enhanced Patient Education Programs | $20,000 – $50,000 | 3-7% | Reduced readmission rates, improved patient outcomes, potentially $50,000 – $150,000 annual increase in revenue |
| Proactive Post-Discharge Follow-up | $10,000 – $30,000 | 2-5% | Reduced readmission rates, improved patient outcomes, potentially $30,000 – $100,000 annual increase in revenue |
Strategic Partnerships and Affiliations

Source: mayflax.com
Strategic alliances are crucial for hospitals seeking to bolster their bottom line and enhance their market position. By collaborating with other healthcare providers, hospitals can leverage shared resources, expand their service offerings, and access new patient populations. This approach can lead to significant improvements in efficiency, revenue generation, and overall patient care.The benefits of strategic partnerships extend beyond simple financial gains.
Boosting your hospital’s bottom line ethically requires a multifaceted approach. Understanding and mitigating preventable conditions, like stroke, is key; check out this article on risk factors that make stroke more dangerous to see how proactive care can reduce costly complications. By focusing on preventative care and efficient treatment protocols, you can compliantly supercharge your hospital’s financial health while improving patient outcomes.
They can foster innovation, improve quality of care through shared best practices, and strengthen the overall healthcare ecosystem within a community. However, careful planning and negotiation are essential to ensure a successful and mutually beneficial partnership.
Types of Hospital Collaborations and Their Financial Implications
Different models of hospital collaboration exist, each with unique financial implications. For example, a joint venture involves the creation of a new entity owned by two or more hospitals. This can lead to shared revenue streams from new services or expanded geographic reach. However, it also requires significant upfront investment and a complex governance structure. Alternatively, a management services agreement sees one hospital managing the operations of another, potentially improving efficiency and reducing costs for the managed hospital while generating revenue for the managing partner.
Finally, affiliations can take the form of clinical integration networks, where hospitals and other providers collaborate on specific care pathways to improve coordination and reduce costs, often leading to improved reimbursements from payers through value-based care models. The financial success of each model hinges on careful planning, clear contracts, and effective management.
Potential Partnerships for Increased Revenue and Market Share
Hospitals can explore partnerships with a wide range of organizations to expand their reach and revenue streams. For example, collaborations with physician groups can secure a consistent referral base and expand access to specialized services. Partnerships with home health agencies can streamline post-discharge care, reducing readmission rates and improving patient outcomes, thereby positively impacting reimbursement. Similarly, affiliations with insurance providers can lead to preferred provider status, attracting more insured patients.
Furthermore, collaborations with research institutions can attract grant funding and attract high-skilled medical professionals, enhancing the hospital’s reputation and drawing in more patients. The key is identifying organizations with complementary strengths and shared goals.
Negotiating Favorable Contracts with Partners
Negotiating successful partnerships requires a strategic approach. Hospitals should clearly define their objectives and desired outcomes before entering negotiations. This includes establishing clear metrics for success, such as revenue targets or improved patient satisfaction scores. The contract should detail the responsibilities of each partner, including financial contributions, operational procedures, and dispute resolution mechanisms. It’s crucial to engage legal counsel specializing in healthcare transactions to ensure the contract is legally sound and protects the hospital’s interests.
Furthermore, robust due diligence is vital to assess the financial stability and operational capabilities of potential partners, mitigating potential risks. A transparent and collaborative approach throughout the negotiation process is key to building a strong and lasting partnership.
Exploring New Revenue Streams
Hospitals are constantly seeking ways to improve their financial health while maintaining high-quality patient care. Diversifying revenue streams is crucial for long-term sustainability and allows hospitals to invest in new technologies and services that benefit both patients and the bottom line. Exploring untapped revenue opportunities requires a strategic approach, combining market analysis with a deep understanding of the hospital’s capabilities and the needs of the community it serves.
Three significant untapped revenue streams for hospitals include specialized outpatient services, telehealth expansion, and strategic partnerships with wellness and preventative care organizations.
Boosting your hospital’s bottom line ethically requires smart strategies. News of Steward Healthcare securing financing amidst bankruptcy, as reported in this article , highlights the critical need for robust financial planning. This emphasizes the importance of proactively implementing compliant revenue cycle management to avoid similar situations and ultimately supercharge your hospital’s financial health.
Specialized Outpatient Services
Hospitals can generate substantial revenue by expanding their outpatient services beyond basic offerings. This involves identifying unmet needs in the community and developing specialized programs to address them. For example, a hospital located in a region with a high aging population could establish a dedicated geriatric outpatient clinic offering comprehensive services like fall prevention programs, memory care assessments, and specialized rehabilitation therapies.
Another example would be a hospital creating a specialized center for minimally invasive surgical procedures, attracting patients seeking less-invasive options and faster recovery times. The success of these programs depends on effective marketing, attracting qualified specialists, and providing high-quality care that leads to positive patient outcomes and referrals.
Telehealth Expansion
Telehealth has emerged as a powerful tool for delivering healthcare services remotely. Hospitals can significantly increase their revenue by expanding their telehealth capabilities beyond simple virtual consultations. This could include developing comprehensive remote patient monitoring programs for chronic conditions like heart failure or diabetes, offering virtual therapy sessions for mental health conditions, or providing remote education and support for patients managing their conditions at home.
A successful telehealth program requires a robust technological infrastructure, well-trained staff, and effective patient engagement strategies. For example, a hospital could partner with a technology provider specializing in remote patient monitoring to ensure seamless data integration and secure communication channels. The resulting increase in patient access, convenience, and improved health outcomes translates into increased revenue and improved patient satisfaction.
Strategic Partnerships with Wellness and Preventative Care Organizations
Hospitals can create new revenue streams by collaborating with organizations focused on wellness and preventative care. This could involve joint ventures offering corporate wellness programs, community health screenings, or health education initiatives. For example, a hospital could partner with a local gym or fitness center to offer discounted memberships to patients and staff, while simultaneously providing health screenings and educational workshops on healthy lifestyle choices.
Another example involves collaborating with a local insurance provider to offer bundled preventative care packages that include screenings, vaccinations, and health coaching. These partnerships not only generate revenue but also enhance the hospital’s reputation as a community leader in health and wellness.
Business Plan: Implementing a Comprehensive Remote Patient Monitoring Program
This business plan Artikels the implementation of a comprehensive remote patient monitoring (RPM) program for patients with chronic heart failure. The program leverages wearable technology and telehealth platforms to provide continuous monitoring, early intervention, and improved patient outcomes.
| Phase | Activities | Timeline | Budget | Metrics |
|---|---|---|---|---|
| Phase 1: Planning & Development | Needs assessment, technology selection, staff training, protocol development | 3 months | $50,000 | Number of patients enrolled, staff training completion rate |
| Phase 2: Implementation & Launch | Patient recruitment, technology deployment, data integration | 2 months | $30,000 | Number of patients actively monitored, data accuracy rate |
| Phase 3: Evaluation & Optimization | Data analysis, program refinement, cost-benefit analysis | Ongoing | $10,000/year | Readmission rates, length of stay, patient satisfaction scores, ROI |
Examples of Successful Hospital Diversification Strategies
Many hospitals have successfully diversified their revenue streams by expanding into new service areas or forging strategic partnerships. For instance, the Cleveland Clinic has diversified into various areas, including research, education, and global healthcare initiatives, creating a robust and sustainable revenue model. Similarly, the Mayo Clinic’s emphasis on research and the development of specialized centers has generated significant revenue and established it as a global leader in healthcare.
These examples demonstrate the potential for hospitals to create sustainable growth by exploring new revenue streams and developing strategic partnerships.
Cost-Benefit Analysis of Investing in New Medical Technologies
Investing in new medical technologies presents both opportunities and challenges. A thorough cost-benefit analysis is crucial to ensure that investments align with the hospital’s financial goals and strategic priorities. This analysis should consider factors such as the initial cost of the technology, ongoing maintenance and operating expenses, potential revenue generation through increased patient volume or new service offerings, and the potential for cost savings through improved efficiency or reduced complications.
For example, investing in a new robotic surgery system might require a significant upfront investment, but it could also lead to shorter hospital stays, reduced complications, and increased demand for the hospital’s services, ultimately generating a positive return on investment. A comprehensive cost-benefit analysis, incorporating both quantitative and qualitative data, is essential for making informed decisions about investments in new medical technologies.
Improving Compliance and Reducing Risk: Compliantly Supercharge Your Hospitals Bottom Line
A robust compliance program is not merely a legal necessity; it’s a cornerstone of financial stability and operational excellence for any hospital. By proactively addressing compliance issues and mitigating risks, hospitals can protect their bottom line, enhance their reputation, and ultimately deliver better patient care. This involves a multi-faceted approach encompassing regulatory adherence, error reduction, and the cultivation of a strong compliance culture.
Methods for Ensuring Compliance and Minimizing Legal Risks
Maintaining compliance requires a systematic and ongoing effort. This includes staying abreast of evolving regulations, implementing effective internal controls, and establishing clear lines of accountability. Regular audits, both internal and external, are crucial for identifying potential weaknesses and ensuring adherence to standards. Furthermore, investing in comprehensive compliance training for all staff members is vital to fostering a culture of compliance and minimizing unintentional violations.
A well-defined compliance plan, regularly reviewed and updated, should detail procedures for handling potential violations, including reporting mechanisms and corrective actions. This proactive approach can significantly reduce the risk of costly legal battles and reputational damage.
Strategies for Reducing Medical Errors and Their Associated Costs
Medical errors represent a significant financial burden on hospitals, encompassing malpractice claims, increased length of stay, and the costs associated with corrective actions. Implementing evidence-based practices, such as standardized protocols and checklists, can significantly reduce the incidence of these errors. Investing in advanced technologies, like electronic health records (EHRs) with built-in safety checks, can also play a crucial role.
Furthermore, fostering a culture of safety, where staff members feel empowered to report errors without fear of retribution, is essential. Regularly reviewing near misses and conducting root cause analyses can identify systemic issues and prevent future errors. A robust system for monitoring and analyzing error rates, coupled with continuous improvement initiatives, can help hospitals minimize the financial impact of medical errors.
For example, a hospital implementing a computerized physician order entry (CPOE) system might see a reduction in medication errors, leading to lower costs associated with adverse drug events.
The Protective Role of a Strong Compliance Program in Maintaining Financial Stability
A strong compliance program acts as a shield against significant financial risks. By proactively addressing compliance issues, hospitals can avoid costly fines and penalties associated with regulatory violations. Moreover, a strong compliance program can enhance the hospital’s reputation and attract patients and insurers who value a commitment to safety and quality. This, in turn, can lead to increased patient volume and improved reimbursement rates.
In the long run, the investment in a robust compliance program significantly outweighs the potential costs of non-compliance. For instance, a hospital that successfully avoids a major lawsuit due to its strong compliance program will save millions in legal fees and potential settlements. This financial stability allows for reinvestment in patient care and infrastructure, further enhancing the hospital’s overall performance.
Checklist for Ensuring Compliance with Key Regulations
Prior to creating a comprehensive compliance checklist, it is crucial to identify the specific regulations applicable to the hospital based on its location, services offered, and patient population. This list provides a general framework and should be tailored to the specific needs of each institution.
- HIPAA Compliance: Regular training on patient privacy and data security, implementation of appropriate safeguards for electronic health information, and procedures for handling breaches.
- Medicare and Medicaid Compliance: Accurate billing practices, adherence to coding guidelines, and compliance with anti-kickback and Stark laws.
- Emergency Medical Treatment and Active Labor Act (EMTALA) Compliance: Appropriate screening and stabilization of patients presenting to the emergency department, regardless of their ability to pay.
- Infection Control: Adherence to infection prevention protocols, including hand hygiene, sterilization techniques, and appropriate isolation procedures.
- Patient Safety: Implementation of evidence-based practices to reduce medical errors, such as medication reconciliation and fall prevention protocols.
- Employee Background Checks and Credentialing: Thorough screening of all employees and medical staff to ensure competence and compliance with relevant regulations.
Investing in Staff Development and Training

Source: nuvolo.com
Investing in your staff isn’t just a nice-to-have; it’s a crucial strategy for supercharging your hospital’s bottom line. A well-trained, engaged workforce translates directly into improved patient care, increased efficiency, and ultimately, higher profitability. This isn’t just about cost-cutting; it’s about strategic investment in your most valuable asset: your people.Employee training and development programs offer a significant return on investment (ROI).
Studies consistently show that improved employee skills lead to increased productivity, reduced errors, and enhanced patient satisfaction. This translates to lower operational costs, improved revenue cycle management, and a stronger reputation, attracting more patients and improving referrals. The initial investment in training pales in comparison to the long-term benefits of a highly skilled and motivated team.
Return on Investment of Employee Training and Development, Compliantly supercharge your hospitals bottom line
Calculating the precise ROI of employee training can be complex, but several key metrics demonstrate its value. For example, consider the reduction in medical errors. A study by the Agency for Healthcare Research and Quality (AHRQ) highlighted that medical errors cost billions annually. Investing in training programs focused on safety protocols and best practices directly reduces these errors, resulting in significant cost savings.
Similarly, improved efficiency in tasks such as medication administration, patient discharge procedures, and administrative processes can lead to measurable improvements in productivity and reduced labor costs. By tracking key performance indicators (KPIs) before and after training initiatives, hospitals can quantify the financial impact of these programs. This data can then be used to justify further investment in staff development.
Programs to Improve Employee Retention and Reduce Turnover Costs
High employee turnover is a significant drain on hospital resources. The costs associated with recruitment, hiring, and training new employees are substantial. Implementing programs designed to improve employee retention can significantly reduce these costs. These programs might include mentorship programs pairing experienced staff with newer employees, offering opportunities for career advancement through internal promotion, providing competitive compensation and benefits packages, and creating a positive and supportive work environment.
Regular employee surveys can provide valuable insights into employee satisfaction and identify areas for improvement. A hospital committed to employee well-being and professional growth is far more likely to retain its valuable staff, minimizing the financial burden of high turnover. For instance, a hospital that implemented a comprehensive mentorship program saw a 20% reduction in nurse turnover within a year, leading to substantial savings in recruitment and training costs.
Employee Engagement and Hospital Profitability
Employee engagement is directly correlated with hospital profitability. Engaged employees are more productive, more likely to provide exceptional patient care, and less likely to leave their jobs. This translates to improved patient satisfaction scores, increased revenue, and reduced operational costs. Hospitals can foster employee engagement through various initiatives, such as creating opportunities for employee input and feedback, recognizing and rewarding employee achievements, promoting a culture of teamwork and collaboration, and offering opportunities for professional development.
A study by Gallup found that highly engaged business units outperform their less engaged counterparts by a significant margin. This same principle applies to hospitals: a highly engaged workforce is a profitable workforce.
Examples of Effective Staff Training Programs
Effective staff training programs are tailored to the specific needs of the hospital and its employees. For example, a program focused on improving communication skills among nurses and physicians can lead to fewer medical errors and improved patient outcomes. Similarly, training programs focused on advanced life support (ALS) or basic life support (BLS) can improve the quality of emergency care.
Simulation-based training, where staff practice procedures in a safe and controlled environment, is a particularly effective method for enhancing skills and improving confidence. These programs can include scenarios simulating real-life situations, allowing staff to practice their skills and learn from their mistakes without risking patient safety. For instance, a hospital that implemented a simulation-based training program for its emergency room staff saw a 15% reduction in medication errors and a 10% improvement in patient satisfaction scores.
Closing Notes
Source: fifthavenueagency.com
Supercharging your hospital’s bottom line compliantly isn’t a one-size-fits-all solution, but a strategic journey. By focusing on efficiency, revenue cycle optimization, patient-centric care, strategic partnerships, and continuous compliance, your hospital can achieve sustainable financial growth. Remember, it’s about finding the right balance between financial success and providing exceptional patient care. The strategies discussed here offer a starting point – tailor them to your unique circumstances and watch your hospital flourish.
FAQ Overview
What are some common compliance pitfalls hospitals face?
Common pitfalls include inaccurate billing and coding, HIPAA violations, and failure to meet regulatory standards for patient safety and quality of care.
How can technology help improve hospital efficiency?
Technology like Electronic Health Records (EHRs), telehealth platforms, and data analytics tools can streamline workflows, reduce administrative burden, and improve patient outcomes, leading to cost savings and increased efficiency.
What are some examples of untapped revenue streams for hospitals?
Examples include offering specialized outpatient services, developing partnerships with wellness centers, and expanding into telehealth services.
How can hospitals improve patient satisfaction scores?
Improved patient satisfaction comes from better communication, personalized care, convenient scheduling, and addressing patient concerns promptly and effectively.