
Shared Decision-Making Informed Healthcare Choices
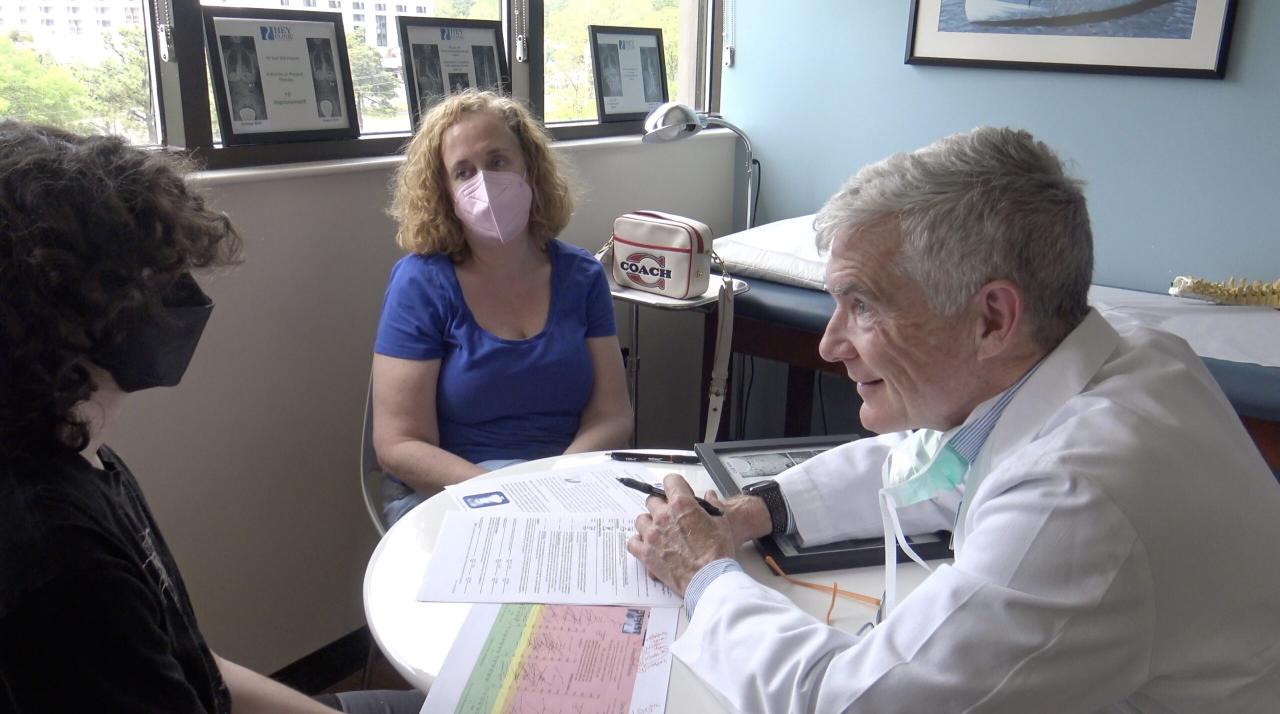
The importance of shared decision making and informed choice in healthcare – The importance of shared decision-making and informed choice in healthcare is paramount. It’s no longer enough for healthcare providers to simply dictate treatment plans; patients deserve a voice in their own care. This approach, which emphasizes collaboration and mutual understanding, leads to better health outcomes, increased patient satisfaction, and a stronger doctor-patient relationship. This post explores the benefits, challenges, and future of this vital shift in healthcare.
We’ll delve into the core principles of shared decision-making (SDM), examining how it differs from traditional paternalistic models. We’ll discuss the practical steps involved, the tools available to facilitate the process, and how to overcome common barriers. Importantly, we’ll also explore the ethical considerations and the crucial role of patient empowerment in achieving truly informed choices.
Defining Shared Decision-Making (SDM) and Informed Choice in Healthcare
Shared decision-making (SDM) and informed choice are cornerstones of modern healthcare, emphasizing patient autonomy and collaboration. They represent a shift away from paternalistic models where the doctor dictates treatment, towards a partnership where patients actively participate in decisions about their health. This approach empowers individuals to make choices that align with their values, preferences, and understanding of their condition.
Shared decision-making, in essence, is a collaborative process where clinicians and patients work together to make healthcare choices. It involves openly discussing the available options, weighing the potential benefits and harms of each, and considering the patient’s values and preferences before arriving at a mutually agreed-upon plan. Informed choice, a crucial component of SDM, ensures that patients have access to the necessary information to understand their condition and the treatment options, enabling them to make a well-considered decision.
Core Principles of Shared Decision-Making in Healthcare
The core principles of SDM revolve around patient autonomy, shared responsibility, and mutual respect. Clinicians provide evidence-based information, explaining the risks and benefits of different options in a clear and understandable way. Patients, in turn, share their preferences, values, and concerns, ensuring that the chosen treatment plan aligns with their overall goals and priorities. Open communication, active listening, and a focus on building a trusting relationship are paramount to successful SDM.
Transparency regarding uncertainties and limitations of available treatments is also essential. A successful SDM process leads to decisions that are not only medically sound but also personally meaningful for the patient.
Key Differences Between Patient-Centered Care and Shared Decision-Making
While both patient-centered care and SDM prioritize the patient’s needs and preferences, there’s a key distinction. Patient-centered care focuses broadly on providing holistic care that considers the individual’s physical, emotional, and social context. SDM, however, is more specific, focusing on the collaborative decision-making process regarding medical interventions and treatments. Patient-centered care might involve a doctor taking time to listen to a patient’s concerns and tailor the treatment plan to their lifestyle, but SDM explicitly involves the patient in choosing from specific treatment options after a thorough discussion of the evidence.
SDM is a subset of patient-centered care, focusing on a specific aspect of the care process.
Situations Where SDM is Particularly Crucial, The importance of shared decision making and informed choice in healthcare
SDM is particularly crucial in situations involving complex medical decisions with multiple treatment options, each carrying different risks and benefits. Examples include:
- Choosing between surgery and non-surgical options for managing a specific condition (e.g., prostate cancer).
- Deciding on the intensity of treatment for chronic illnesses like diabetes or heart failure.
- Selecting among different cancer therapies with varying side effect profiles.
- Making end-of-life care decisions, such as choosing hospice care or aggressive life-sustaining treatment.
- Managing chronic pain, considering various pain management strategies and their potential risks and benefits.
In these scenarios, the patient’s values and preferences play a significant role in determining the optimal course of action. A one-size-fits-all approach is inappropriate; SDM ensures that the chosen path aligns with the individual’s life goals and priorities.
Steps Involved in a Typical SDM Process
A typical SDM process can be broken down into several key steps. The following table Artikels these steps, their descriptions, and potential challenges:
| Step | Description | Potential Challenges |
|---|---|---|
| 1. Defining the Clinical Problem | Clearly outlining the medical condition, its prognosis, and available treatment options. | Difficulties in communicating complex medical information clearly and concisely. |
| 2. Exploring Patient Preferences and Values | Understanding the patient’s goals, priorities, and concerns regarding their health and treatment. | Patients may be unclear about their preferences or have conflicting values. |
| 3. Presenting Treatment Options | Providing evidence-based information on each treatment option, including benefits, risks, and uncertainties. | Information overload, difficulty understanding medical jargon, and differing levels of health literacy. |
| 4. Collaborative Decision-Making | Working together to weigh the benefits and risks of each option, considering the patient’s preferences and values. | Power imbalances between clinician and patient, difficulty reaching consensus. |
| 5. Implementing the Chosen Plan | Putting the agreed-upon treatment plan into action. | Challenges in coordinating care and ensuring adherence to the treatment plan. |
| 6. Monitoring and Evaluation | Regularly assessing the effectiveness of the treatment and making adjustments as needed. | Difficulties in tracking outcomes and adapting the plan based on changes in the patient’s condition. |
Benefits of Shared Decision-Making for Patients

Source: squarespace-cdn.com
Shared decision-making (SDM) offers a wealth of benefits for patients, extending far beyond simply receiving a diagnosis and treatment plan. It fundamentally shifts the power dynamic in the doctor-patient relationship, fostering a collaborative partnership that leads to improved health outcomes and a more positive overall experience. This approach empowers patients to actively participate in their care, leading to increased satisfaction and a stronger commitment to following treatment recommendations.SDM improves patient satisfaction and adherence to treatment plans by actively involving patients in the decision-making process.
When patients feel heard and understood, and when they have a clear understanding of the risks and benefits of different treatment options, they are more likely to feel confident in their choices and more committed to following through with their chosen course of action. This shared responsibility fosters a sense of ownership over their health, leading to better compliance and ultimately, improved health outcomes.
Studies have shown a direct correlation between patient involvement in decision-making and improved adherence to medication regimens and lifestyle changes. For example, a patient choosing between two surgical procedures after thoroughly discussing the pros and cons with their surgeon is more likely to follow post-operative instructions diligently compared to a patient who feels they were simply told what to do.
Impact of SDM on Patient Empowerment and Health Literacy
SDM significantly enhances patient empowerment by fostering a sense of control over their healthcare journey. Instead of passively receiving instructions, patients become active participants, learning about their condition and treatment options, and making informed choices based on their values and preferences. This process inherently improves health literacy, as patients are encouraged to ask questions, seek clarification, and understand the medical information presented to them.
The increased understanding empowers them to make decisions aligned with their personal goals and circumstances. Consider a patient diagnosed with diabetes who actively participates in discussions about managing their blood sugar levels through diet and exercise. This active involvement leads to a greater understanding of the disease and better self-management skills.
Reduction of Anxiety and Improvement of the Overall Patient Experience
The anxiety often associated with serious illnesses and medical procedures can be significantly reduced through SDM. Open communication and a collaborative approach create a sense of security and trust between the patient and healthcare provider. Knowing that their concerns and preferences are valued, and that they have a voice in shaping their treatment plan, can alleviate much of the stress and uncertainty surrounding a diagnosis.
Furthermore, the increased understanding gained through SDM can reduce fear of the unknown and empower patients to navigate their healthcare journey with greater confidence. For instance, a patient facing a complex cancer diagnosis who actively participates in treatment planning alongside their oncologist is likely to experience less anxiety compared to a patient who feels passively informed about their treatment options.
Psychological Benefits of Participating in SDM
The psychological benefits of participating in SDM are substantial. When patients feel empowered and in control of their healthcare decisions, it fosters a sense of:
- Increased self-efficacy: The belief in one’s ability to manage their health effectively.
- Reduced anxiety and stress: A greater sense of control leads to lower levels of anxiety and stress.
- Improved mood and well-being: Active participation and a sense of agency contribute to overall well-being.
- Enhanced satisfaction with care: Feeling heard and valued leads to greater satisfaction with the healthcare experience.
- Greater adherence to treatment plans: A sense of ownership and understanding fosters better compliance.
Benefits of Shared Decision-Making for Healthcare Providers
Shared decision-making (SDM) isn’t just beneficial for patients; it offers significant advantages for healthcare providers as well. By shifting from a paternalistic model to one of collaboration and partnership, providers can experience improvements in efficiency, relationships, and even risk mitigation. This ultimately contributes to a more sustainable and fulfilling healthcare environment for everyone involved.
Improved Efficiency of Healthcare Delivery
SDM can streamline the healthcare process by clarifying patient expectations and preferences upfront. This reduces the likelihood of unnecessary tests, procedures, or consultations driven by misunderstandings or unmet patient needs. For example, a patient fully informed about the risks and benefits of different treatment options for knee arthritis might opt for physical therapy initially, avoiding the immediate need for surgery and its associated costs and recovery time.
This efficient use of resources translates into reduced healthcare spending and improved allocation of provider time. Furthermore, clear communication minimizes the need for follow-up appointments to address misunderstandings or unresolved concerns.
Positive and Collaborative Provider-Patient Relationship
SDM fosters a more trusting and respectful relationship between provider and patient. When patients feel heard and actively involved in their care, they are more likely to adhere to treatment plans, resulting in better health outcomes. This collaborative approach builds rapport and mutual respect, enhancing the overall experience for both parties. For instance, a patient with diabetes who participates in developing a personalized management plan, considering their lifestyle and preferences, is more likely to actively monitor their blood sugar and adhere to dietary recommendations.
This shared responsibility fosters a stronger therapeutic alliance.
Reduction in Medical Errors and Malpractice Claims
By involving patients in decision-making, SDM reduces the potential for misunderstandings and errors. When patients are fully informed and actively participate in choosing their treatment, they are more likely to understand and accept the risks and benefits involved. This shared understanding can significantly reduce the risk of medical errors and subsequent malpractice claims. Consider a scenario where a patient, after discussing various surgical options with their surgeon, understands and accepts the potential complications of a particular procedure.
This shared understanding minimizes the risk of the patient feeling misled or dissatisfied, potentially reducing the likelihood of a malpractice suit.
Workload Implications of SDM versus Traditional Approaches
While SDM may initially seem more time-consuming than a traditional paternalistic approach, the long-term benefits outweigh the initial investment. The upfront time spent in shared decision-making can lead to significant time savings in the long run by reducing the need for follow-up appointments, managing complications from poorly understood treatment plans, and minimizing the administrative burden associated with managing disputes or malpractice claims.
In essence, the initial increase in workload is offset by the improved efficiency and reduced complications associated with better patient understanding and adherence. The shift from a reactive to a proactive approach leads to a more sustainable and ultimately less demanding workload in the long term.
Barriers to Implementing Shared Decision-Making
Implementing shared decision-making (SDM) in healthcare faces significant hurdles. While the benefits are clear, translating the ideal of patient-centered care into everyday practice requires addressing a range of practical and ethical challenges. These barriers often intertwine, making a multifaceted approach necessary for successful implementation.
Time Constraints in Healthcare Settings
The fast-paced nature of many healthcare settings presents a major obstacle to SDM. Providers often feel pressured to see a high volume of patients within limited timeframes, leaving little room for extended discussions about treatment options and preferences. This time constraint can lead to rushed consultations, where patients may not fully understand their choices or feel adequately involved in the decision-making process.
Overcoming this requires systemic changes, such as adjusting appointment scheduling to accommodate longer consultations for complex cases or implementing efficient communication tools that streamline information exchange. For example, pre-visit questionnaires allowing patients to articulate their priorities and concerns could significantly reduce the time spent during the consultation itself. Additionally, training providers in efficient communication techniques, such as motivational interviewing, can optimize the use of available time.
Communication Barriers and Health Literacy
Effective SDM hinges on clear and understandable communication. However, differences in medical jargon, language barriers, and varying levels of health literacy can create significant obstacles. Patients may struggle to understand complex medical information, leading to poor comprehension of treatment options and their potential consequences. This is particularly problematic for patients with low health literacy, who may be more vulnerable to making uninformed choices.
Strategies to overcome this include using plain language materials, providing visual aids, and employing interpreters when necessary. Healthcare providers also benefit from training in effective communication techniques tailored to diverse patient populations, ensuring that information is presented in a way that is accessible and easily understood by all.
Lack of Provider Training and Support
Many healthcare professionals lack the necessary training and support to effectively implement SDM. SDM requires a shift in mindset, moving from a paternalistic model to a collaborative partnership with patients. This requires specific skills in communication, negotiation, and conflict resolution. Furthermore, providers may feel uncertain about their role in SDM, lacking confidence in facilitating patient-centered discussions. Addressing this requires investing in comprehensive training programs for healthcare professionals that focus on SDM principles, techniques, and practical application.
Ongoing mentorship and support are also crucial, creating a culture where SDM is valued and actively promoted.
Healthcare System and Policy Barriers
Systemic factors, such as reimbursement models that prioritize efficiency over patient engagement, can inadvertently discourage SDM. Current payment structures often incentivize quick consultations rather than prolonged discussions necessary for shared decision-making. Policies that support SDM are needed, including the development of standardized tools and resources, integration of SDM into clinical guidelines, and the establishment of performance indicators that reflect the quality of patient-centered care.
Empowering patients through shared decision-making is key to better healthcare outcomes. For conditions like carpal tunnel syndrome, understanding your options is crucial. Check out this helpful resource on ways to treat carpal tunnel syndrome without surgery to make an informed choice alongside your doctor. Ultimately, taking an active role in your treatment plan leads to better results and a more positive healthcare experience.
Furthermore, adequate funding for training programs and ongoing support is essential to facilitate the widespread adoption of SDM across various healthcare settings.
Ethical Considerations in SDM
Ethical considerations are paramount, particularly when dealing with patients who lack decision-making capacity due to cognitive impairments or limited health literacy. Respect for patient autonomy remains a cornerstone of ethical medical practice.
Respect for persons requires that clinicians respect the decisions of competent patients, even if those decisions are not in the patient’s best medical interest.
However, ensuring patient autonomy requires careful consideration when capacity is compromised. In such cases, involving family members or legal guardians in the decision-making process while upholding the patient’s best interests becomes crucial.
Beneficence requires that clinicians act in the best interests of their patients. This includes providing information that is clear, accurate, and relevant to the patient’s needs and preferences.
Balancing beneficence with respect for autonomy in situations of diminished capacity demands a sensitive and nuanced approach, ensuring that decisions are made in a way that reflects the patient’s values and preferences to the greatest extent possible. This may involve utilizing advanced care planning tools and engaging in thoughtful discussions with family members to understand the patient’s wishes and priorities.
Tools and Resources for Facilitating Shared Decision-Making
Effective shared decision-making (SDM) relies heavily on the availability and utilization of appropriate tools and resources. These tools empower both patients and healthcare providers to engage in a more informed and collaborative process, ultimately leading to better health outcomes and increased patient satisfaction. This section will explore various resources, the role of technology, and the importance of provider training in facilitating successful SDM.
Decision Aids and Other Resources
Decision aids are specifically designed to help individuals understand and weigh the options available for a particular health decision. They typically present information about different treatment options, including their benefits, risks, and potential side effects, often in a clear and easily digestible format. Examples include brochures, videos, interactive websites, and mobile applications. Some decision aids even use visual aids like charts and graphs to illustrate complex information.
Beyond decision aids, other resources like patient education materials, support groups, and access to reliable health information websites also play a crucial role in supporting SDM. For example, a patient facing a choice between surgery and medication for a specific condition might benefit from a decision aid comparing the effectiveness, risks, and recovery times associated with each option. This allows the patient to actively participate in the discussion with their physician, rather than passively receiving a recommendation.
Technology’s Role in Enhancing SDM
Technology offers significant potential for enhancing SDM processes. Patient portals, for example, allow patients to access their medical records, communicate with their healthcare providers, and even complete decision aids online at their own pace. Telemedicine platforms can also facilitate SDM, particularly for patients in remote areas or with mobility limitations. Furthermore, the use of artificial intelligence (AI) is emerging as a potential tool to personalize decision aids and provide tailored information to individual patients based on their specific characteristics and preferences.
For instance, an AI-powered system could analyze a patient’s medical history and preferences to recommend the most appropriate decision aid and ensure that the information presented is relevant and understandable. This level of personalization enhances the effectiveness of SDM by addressing the unique needs of each patient.
Training Healthcare Providers in SDM Techniques
Effective implementation of SDM requires adequately trained healthcare providers. Training programs should focus on developing communication skills, such as active listening, empathy, and eliciting patient preferences. Providers also need to learn how to present information clearly and concisely, avoiding medical jargon, and how to facilitate a collaborative discussion that respects patient autonomy. Furthermore, training should include practical experience in using SDM tools and navigating potential challenges, such as dealing with emotional responses or conflicting preferences.
A well-structured training program would incorporate role-playing exercises, case studies, and feedback sessions to equip healthcare providers with the skills and confidence to effectively engage in SDM. This investment in provider training is crucial for the widespread adoption and successful implementation of SDM practices.
Comparison of SDM Tools
It’s important to understand that the effectiveness of different SDM tools varies depending on the specific context and the needs of the patients involved. The following table provides a comparison of some common tools:
| Tool Name | Description | Target Audience | Limitations |
|---|---|---|---|
| Interactive Website Decision Aid | Provides detailed information about treatment options, including benefits, risks, and costs, in an interactive format. | Patients with internet access and some computer literacy. | May require significant time commitment; digital literacy is a barrier for some. |
| Printed Brochure Decision Aid | Offers concise information about treatment options in a readily accessible format. | All patients, regardless of technological access. | Limited interactivity; may not be suitable for complex decisions. |
| Shared Decision-Making Software | Software designed to guide conversations between patients and providers, helping to document preferences and choices. | Healthcare providers and patients. | Requires technological infrastructure and provider training; cost may be a barrier. |
| Video Decision Aid | Presents information through video, which can be engaging and easy to understand. | All patients, particularly those who benefit from visual aids. | May not be suitable for all health literacy levels; requires access to video playback technology. |
Measuring the Effectiveness of Shared Decision-Making
Source: heyclinic.com
Evaluating the impact of shared decision-making (SDM) on patient outcomes requires a multifaceted approach, combining quantitative and qualitative methods to gain a comprehensive understanding of its effectiveness. Successfully measuring the impact goes beyond simply tracking participation rates; it necessitates assessing changes in patient knowledge, satisfaction, and ultimately, health outcomes.
Methods for Evaluating the Impact of SDM on Patient Outcomes
Several methods can be employed to assess the impact of SDM interventions. Quantitative methods often involve measuring changes in patient knowledge using validated questionnaires before and after an SDM intervention. For instance, researchers might use a scale measuring understanding of treatment options or the ability to articulate personal preferences. Furthermore, patient satisfaction can be measured using standardized surveys, focusing on aspects like the perceived quality of the interaction with the healthcare provider, the clarity of information received, and the feeling of being involved in the decision-making process.
Finally, objective health outcomes, such as adherence to treatment plans, symptom reduction, or disease progression, can be tracked and compared between groups receiving SDM and those receiving standard care. The choice of specific outcome measures will depend on the context of the intervention and the specific condition being addressed.
Key Metrics for Assessing the Success of SDM Initiatives
Key metrics for evaluating SDM initiatives include patient activation, measured by scales assessing patients’ knowledge, skills, and confidence in managing their health; treatment adherence, reflecting the extent to which patients follow their agreed-upon treatment plans; patient satisfaction with the decision-making process, gauged through post-intervention surveys; and finally, relevant clinical outcomes, such as improved disease control or reduced hospital readmissions. These metrics provide a balanced assessment, encompassing both the process and the results of SDM.
For example, a successful SDM initiative might demonstrate significant improvements in patient activation scores, higher treatment adherence rates, and ultimately, better clinical outcomes.
Using Qualitative Data to Understand the Patient Experience with SDM
Qualitative data, gathered through methods like semi-structured interviews or focus groups, provides rich insights into the patient experience with SDM. This approach allows researchers to explore patients’ perspectives on the process, including their perceived level of involvement, the clarity of information received, and the overall satisfaction with the decision-making experience. Qualitative data can illuminate aspects of SDM that quantitative measures might miss, such as the emotional impact of participation or the identification of unexpected barriers to effective SDM.
For example, qualitative interviews might reveal that while patients report high satisfaction with the process, they still struggle with understanding complex medical information, highlighting the need for improved communication strategies.
Examples of Research Studies Investigating the Effectiveness of SDM
Several studies have demonstrated the effectiveness of SDM. A meta-analysis published in the
- BMJ* reviewed numerous studies on SDM interventions and found that SDM was associated with improved patient knowledge, satisfaction, and treatment adherence across various health conditions. Another study published in
- Patient Education and Counseling* investigated the impact of a structured SDM intervention on patients’ decisional conflict and quality of life, demonstrating a significant reduction in decisional conflict and an improvement in quality of life among patients who participated in the intervention. These studies, and many others, highlight the positive impact of SDM on various patient-centered outcomes. The specific findings vary depending on the intervention, the patient population, and the health condition being addressed, emphasizing the need for tailored SDM approaches.
Empowering patients through shared decision-making is crucial for better health outcomes. Understanding your personal risks is key, especially for serious conditions like stroke. Learning about the specific risk factors that make stroke more dangerous allows for proactive choices and informed discussions with your doctor. This collaborative approach ensures the best possible treatment plan, tailored to your individual needs and circumstances.
Future Directions in Shared Decision-Making: The Importance Of Shared Decision Making And Informed Choice In Healthcare

Source: withingshealthsolutions.com
Shared decision-making (SDM) is evolving rapidly, driven by technological advancements and a growing recognition of patient autonomy. The future of SDM promises more personalized, efficient, and effective healthcare experiences, but realizing this potential requires continued innovation and research.The integration of technology is reshaping the landscape of SDM, offering exciting possibilities for improving the process and expanding its reach.
Artificial Intelligence and Technology in SDM
AI has the potential to revolutionize SDM in several ways. AI-powered tools can personalize information delivery, tailoring explanations of treatment options to individual patient preferences and health literacy levels. Imagine a system that automatically generates decision aids based on a patient’s specific medical history, values, and risk factors, presented in a format easily understood by the individual. Furthermore, AI chatbots could provide initial support and answer common questions, freeing up clinicians to focus on more complex discussions and relationship-building.
Natural language processing could analyze patient conversations to identify areas of uncertainty or disagreement, alerting clinicians to potential communication barriers. While ethical considerations regarding data privacy and algorithmic bias need careful attention, the potential benefits of AI in enhancing SDM are significant. For example, a recent study showed that an AI-powered chatbot improved patient understanding of treatment options for chronic pain.
Ongoing Research and Development in SDM Methodologies
Further research is crucial to refine existing SDM methods and develop new approaches that address diverse patient populations and healthcare settings. Studies are needed to evaluate the effectiveness of different SDM interventions across various conditions and demographics, including vulnerable populations such as those with limited health literacy or cognitive impairments. Research should also explore innovative methods for measuring the impact of SDM on patient outcomes, beyond simply measuring satisfaction.
Empowering patients through shared decision-making is crucial for better health outcomes. It’s all about informed choices, and sometimes, understanding the financial realities of healthcare systems helps. For instance, the recent news that Steward Health Care secures financing to emerge from bankruptcy highlights the complex financial landscape impacting access to care. Ultimately, shared decision-making ensures patients are actively involved in navigating this complexity to make the best choices for their health.
For example, researchers could explore the use of wearable sensors to track patient adherence to treatment plans, providing objective data on the effectiveness of SDM in improving outcomes. Developing standardized protocols for implementing SDM and measuring its effectiveness across different healthcare settings will be vital for widespread adoption.
Scenario: SDM in a Future Healthcare Setting
Consider a patient, Sarah, diagnosed with early-stage breast cancer. Upon receiving her diagnosis, Sarah is immediately connected to a personalized SDM platform via her smartphone. This platform, powered by AI, provides her with comprehensive information about her treatment options – surgery, chemotherapy, radiation, and hormonal therapy – presented in an accessible and engaging format tailored to her health literacy level and preferences.
An AI-powered chatbot answers her initial questions and concerns, providing immediate support. Later, during a virtual consultation with her oncologist, the platform facilitates a shared decision-making process by displaying Sarah’s preferences, risk factors, and treatment goals in real-time. The oncologist can use this information to tailor the conversation and ensure Sarah fully understands the implications of each choice.
After the consultation, the platform provides Sarah with a personalized action plan, including appointment reminders, medication management tools, and links to support groups. Regular check-ins via the platform ensure ongoing support and allow for adjustments to the treatment plan based on Sarah’s evolving needs and preferences. The platform also automatically collects data on Sarah’s progress, enabling researchers to track the long-term effectiveness of the SDM intervention and identify areas for improvement.
Epilogue
Ultimately, the journey towards shared decision-making in healthcare is a journey towards a more equitable and effective system. By empowering patients to actively participate in their care, we foster trust, improve adherence to treatment plans, and ultimately enhance overall health outcomes. While challenges remain, the benefits of shared decision-making are undeniable, paving the way for a future where patients are not just recipients of care, but active partners in their own well-being.
Quick FAQs
What if I don’t understand the medical jargon my doctor uses?
Don’t hesitate to ask your doctor to explain things in simpler terms. It’s their job to ensure you understand your options and the implications of each.
Can I bring a family member or friend to help me make decisions?
Absolutely! Having a support person present can be very helpful, especially when dealing with complex medical information.
What if I disagree with my doctor’s recommendation?
Open communication is key. Explain your concerns and explore alternative options together. A good doctor will respect your preferences and work with you to find a solution.
Is shared decision-making always the best approach?
While SDM is generally beneficial, there may be exceptions, such as emergencies or situations where a patient lacks decision-making capacity. In these cases, the focus shifts to ensuring the patient’s safety and well-being.
