Molina Healthcare Acquires Connecticare & EmblemHealth
Molina healthcare acquire connecticare emblemhealth – Molina Healthcare acquiring Connecticare and EmblemHealth is HUGE news in the healthcare world! This massive merger shakes things up significantly, impacting everything from market competition and consumer costs to the employment of thousands and the future direction of Molina itself. It’s a complex deal with far-reaching consequences, and we’re diving deep into what it all means for patients, providers, and the industry as a whole.
This acquisition represents a significant strategic move by Molina Healthcare, potentially solidifying their position as a major player in the Northeast. The financial implications are enormous, and the regulatory hurdles are substantial. We’ll explore the potential benefits and risks, analyzing the projected financial performance and long-term strategic goals. Get ready for a deep dive into the details!
Molina Healthcare’s Acquisition Strategy: Molina Healthcare Acquire Connecticare Emblemhealth
Molina Healthcare has established itself as a significant player in the managed care industry, largely through a strategic acquisition strategy focused on expanding its geographic reach and diversifying its product offerings. This approach, while inherently risky, has yielded considerable growth over the years. The recent acquisition of Connecticare and EmblemHealth represents a continuation of this long-term strategy.
Historical Acquisition Patterns of Molina Healthcare
Molina Healthcare’s acquisition history reveals a preference for acquiring smaller, regional health plans. This allows them to gain a foothold in new markets with established provider networks and customer bases, minimizing the challenges of building from scratch. They often target plans that complement their existing strengths, either geographically or in terms of specialized services. The acquisitions aren’t always large-scale; instead, they demonstrate a pattern of strategic, incremental growth.
This approach allows Molina to integrate acquisitions more smoothly and avoid overwhelming their existing infrastructure. This measured approach contrasts with some of the larger, more aggressive merger activity seen in other sectors of the healthcare industry.
Financial Motivations Behind the Connecticare and EmblemHealth Acquisition
The acquisition of Connecticare and EmblemHealth offers several key financial advantages for Molina Healthcare. First, it significantly expands Molina’s presence in the Northeast, a region with a large and growing population of Medicare and Medicaid beneficiaries – key target markets for Molina. Second, the acquisition adds established provider networks and a substantial customer base, immediately increasing market share and revenue streams.
Third, economies of scale resulting from the merger will likely lead to cost reductions in administration, technology, and other operational areas. Finally, the acquisition diversifies Molina’s portfolio, reducing reliance on any single geographic market or payer source, thus mitigating financial risk. These combined factors are likely to lead to significant long-term profitability gains.
Comparison to Other Significant Healthcare Mergers and Acquisitions
The Molina Healthcare acquisitions differ from some of the mega-mergers seen in the industry, such as the CVS Health acquisition of Aetna. Those large-scale mergers often focus on vertical integration, combining pharmaceutical benefits management with health insurance. Molina’s acquisitions, while substantial, are more focused on horizontal expansion, increasing market share within their existing business model. This more targeted approach minimizes integration complexities compared to the massive overhauls required by vertically integrated mergers.
A similar, more focused approach can be seen in the acquisitions made by Centene Corporation, which, like Molina, has strategically expanded its market presence through the acquisition of smaller regional health plans.
Hypothetical Timeline for Integration of Connecticare and EmblemHealth into Molina Healthcare
A successful integration of Connecticare and EmblemHealth into Molina Healthcare will likely unfold over several phases.
- Phase 1 (0-6 months): Due diligence completion, regulatory approvals, and initial planning for system integration. This phase will involve significant legal and logistical work, ensuring compliance with all regulations and setting the stage for a smooth transition.
- Phase 2 (6-18 months): System integration, including IT infrastructure consolidation, provider network alignment, and member communication. This phase will require careful coordination to minimize disruption to member services and ensure a seamless transition for providers.
- Phase 3 (18-36 months): Operational optimization, cost reduction initiatives, and full integration of back-office functions. This phase focuses on achieving synergies and realizing the cost savings projected from the merger.
- Phase 4 (36+ months): Ongoing monitoring and evaluation of integration success, along with further refinement of processes and strategies. This long-term phase involves continuous improvement and adaptation to ensure the long-term success of the merged entities.
This timeline is a hypothetical projection and the actual timeline may vary depending on various factors, including regulatory approvals and unforeseen challenges. However, it provides a reasonable framework for understanding the potential integration process.
Market Impact of the Merger
Molina Healthcare’s acquisition of Connecticare and EmblemHealth has significant implications for the healthcare landscape in the affected regions. The merger’s impact will ripple through various sectors, affecting competition, consumer costs, and the operations of healthcare providers. Analyzing these changes is crucial to understanding the long-term consequences of this consolidation.The combined entity will create a larger, more powerful player in the regional healthcare market.
Changes in the Healthcare Landscape
The merger will likely lead to a reshaping of the healthcare landscape in the areas served by Connecticare and EmblemHealth. We can anticipate changes in the availability of certain plans, potentially a shift in the emphasis on specific services, and possibly the introduction of new technologies or care delivery models driven by Molina’s existing strategies. For example, Molina’s focus on managed care and its experience with Medicaid and Medicare Advantage programs could lead to a greater emphasis on preventative care and care coordination within the acquired plans.
This could result in improved health outcomes for some members, but may also lead to limitations in the choice of providers or treatments for others. The integration process itself may cause temporary disruptions, such as changes to provider networks and administrative procedures.
Impact on Competition
The acquisition reduces the number of major health insurance providers in the relevant markets, leading to decreased competition. This reduced competition could potentially lead to less pressure on the merged entity to keep premiums and out-of-pocket costs low. In regions where Connecticare and EmblemHealth were the primary competitors, consumers may find themselves with fewer choices of health plans, potentially leading to less plan flexibility and choice.
This decreased competition could also potentially impact the bargaining power of healthcare providers negotiating reimbursement rates with the insurance company. Similar mergers in other states have resulted in observable increases in premiums following consolidation.
Effects on Healthcare Costs for Consumers
The impact on consumer healthcare costs is a complex issue. While the merger could theoretically lead to increased negotiating power allowing for lower provider costs, the decreased competition also creates the potential for higher premiums and out-of-pocket expenses for consumers. The actual outcome will depend on several factors, including the regulatory oversight of the merger, the merged entity’s pricing strategies, and the overall health of the regional healthcare market.
Historically, similar mergers have shown mixed results, with some leading to cost increases and others resulting in minimal changes. It’s essential to monitor premium and cost-sharing changes closely in the years following the merger.
Implications for Healthcare Providers
The merger will undoubtedly impact healthcare providers in the affected areas. Negotiations regarding reimbursement rates between the merged entity and providers could change significantly. Providers may find themselves facing a larger, more powerful payer with potentially more leverage in contract negotiations. This could lead to reduced reimbursement rates for services, impacting provider profitability and potentially affecting the availability of certain specialists or services in the region.
Providers may need to adapt their business models to maintain financial viability within the new competitive landscape created by the merger. This could involve increased efficiency, diversification of revenue streams, or a greater focus on value-based care models favored by larger insurers.
Regulatory Scrutiny and Approval Process

Source: dreamstime.com
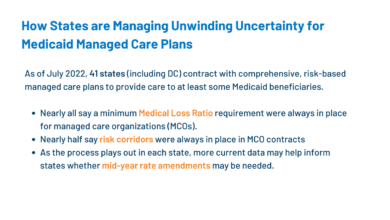
The Molina Healthcare acquisition of Connecticare and EmblemHealth faces a complex and potentially lengthy regulatory review process. Several federal and state agencies will scrutinize the deal, focusing on its potential impact on competition, consumer prices, and healthcare access. Failure to navigate these hurdles successfully could lead to delays, modifications to the acquisition agreement, or even its complete rejection.The primary concern centers around antitrust regulations.
Mergers and acquisitions are carefully examined to prevent the creation of monopolies or oligopolies that could stifle competition and harm consumers. In the healthcare sector, this is particularly important given the already complex dynamics of insurance markets and the potential for increased premiums or reduced choice for consumers.
Antitrust Concerns
The Department of Justice (DOJ) and the Federal Trade Commission (FTC) will be key players in assessing the antitrust implications of the merger. They will analyze the combined market share of Molina Healthcare post-acquisition, focusing on specific geographic areas and demographic groups. The agencies will investigate whether the merger will lead to less competition, resulting in higher prices, reduced quality of care, or less innovation.
Molina Healthcare’s acquisition of Connecticare and EmblemHealth is huge news, significantly expanding their reach. This kind of growth inevitably increases administrative burdens, especially in medical coding. That’s why I was thinking about how helpful a solution like the ai powered solution to the medical coding worker shortage could be for them, streamlining processes and potentially offsetting staffing challenges.
Ultimately, efficient coding is key to the success of such a large-scale merger.
For example, if the combined entity controls a disproportionately large share of the market in a particular region, the regulators might raise concerns about the potential for anti-competitive behavior such as price fixing or reduced benefits. The regulators will also consider the presence and strength of competing health insurance providers in the affected markets. A detailed analysis of the market dynamics and competitive landscape will be essential to determining the ultimate impact of the merger.
Regulatory Bodies Involved
The approval process will involve multiple federal and state agencies. This list is not exhaustive, as involvement may vary based on the specific details of the acquisition and the affected states.
- Department of Justice (DOJ): The DOJ’s Antitrust Division will scrutinize the merger for potential violations of antitrust laws.
- Federal Trade Commission (FTC): The FTC also has authority to review mergers and acquisitions for antitrust concerns, often working in conjunction with or independently of the DOJ.
- State Insurance Departments: Each state where Connecticare and EmblemHealth operate will likely have its own insurance department that must approve the acquisition. These departments will focus on the impact on consumer protection, market stability, and the solvency of the combined entity.
Hypothetical Timeline for Regulatory Review
Predicting the exact timeline for regulatory approval is challenging, as it depends on the complexity of the deal, the level of cooperation from Molina Healthcare, and the agencies’ workload. However, a plausible timeline might look like this:
- Filing (Months 1-2): Molina Healthcare formally files all necessary paperwork with the relevant federal and state agencies.
- Initial Review (Months 3-6): Agencies conduct preliminary reviews, requesting additional information as needed. This phase may involve informal discussions between Molina Healthcare and the regulators.
- In-depth Investigation (Months 7-12): If the initial review raises concerns, a more thorough investigation may be launched, potentially including interviews, document requests, and expert analysis.
- Negotiations and Remedies (Months 13-18): If antitrust concerns are identified, Molina Healthcare might be required to propose remedies, such as divestitures of certain assets or commitments to maintain competition. This stage involves negotiations between the company and the regulatory agencies.
- Approval or Rejection (Months 19-24): Following the completion of the investigation and any necessary negotiations, the agencies will issue a decision regarding approval or rejection of the merger. This timeline assumes a relatively straightforward review. More complex cases could extend significantly beyond this timeframe.
Impact on Employees and Patients

Source: brightspotcdn.com
The Molina Healthcare acquisition of Connecticare and EmblemHealth presents significant implications for both employees and patients. While the promise of a larger, more integrated healthcare system offers potential benefits, it also introduces uncertainties regarding job security, healthcare coverage, and the continuity of care. Understanding these potential impacts is crucial for all stakeholders involved.
Employment Impacts on Connecticare and EmblemHealth Staff
The merger’s effect on employment will likely vary depending on the specific roles and locations within Connecticare and EmblemHealth. Molina Healthcare might consolidate certain administrative functions, leading to potential redundancies. Conversely, opportunities might arise in areas where Molina requires additional expertise or personnel to manage the expanded operations. Historically, similar mergers have seen a mix of job losses, reassignments, and new hiring, depending on the integration strategy adopted by the acquiring company.
For example, the Aetna-Humana merger resulted in some job cuts in overlapping administrative roles, while simultaneously creating new positions in areas like data analytics and technology integration. The actual outcome will depend on Molina’s integration plan and the overall efficiency targets they aim to achieve.
Changes to Healthcare Coverage and Benefits for Patients
Patients can anticipate some changes to their healthcare coverage and benefits following the acquisition. Molina Healthcare may adjust provider networks, formularies (lists of covered medications), and benefit packages. These adjustments could lead to changes in out-of-pocket costs, access to specific doctors or hospitals, and the availability of certain treatments or medications. While Molina may strive to maintain a similar level of coverage, some benefits might be altered to streamline operations and reduce costs.
For instance, a patient previously covered for a specific therapy under Connecticare might find that therapy is now covered under a different tier or requires prior authorization under Molina’s plan. Transparency regarding these changes will be crucial to minimizing patient disruption.
Continuity of Care for Existing Patients
Ensuring continuity of care is a significant concern. Patients may worry about losing their established relationships with physicians and healthcare providers. Disruptions to care can be particularly problematic for individuals with chronic conditions or complex medical needs. Molina’s success in managing this transition will depend heavily on their communication strategies and their ability to seamlessly integrate the existing patient base into their system.
A well-executed transition plan should include proactive communication to patients, maintaining access to existing providers whenever possible, and offering clear guidance on navigating the new system. Failure to address this effectively could lead to decreased patient satisfaction and potential negative impacts on health outcomes.
Molina Healthcare’s Transition Strategies for Patients
To ensure a smooth transition, Molina Healthcare is likely to employ several strategies. These could include robust communication campaigns informing patients about the changes, establishing dedicated support lines and websites to answer questions, and creating a comprehensive patient portal for easy access to information and benefits. They might also implement measures to maintain access to existing providers whenever feasible, perhaps through contractual agreements or temporary allowances.
Furthermore, Molina may invest in technology to facilitate the integration of patient records and streamline the claims processing system. Successful implementation of these strategies will be crucial to minimizing patient confusion and ensuring a positive experience during the transition. Examples of such strategies can be seen in previous healthcare mergers, where companies like Anthem have successfully used multi-channel communication and dedicated transition teams to ease patient concerns.
Financial Projections and Analysis of the Deal
Molina Healthcare’s acquisition of Connecticare and EmblemHealth represents a significant strategic move, and understanding the financial underpinnings of this deal is crucial. The success of the merger hinges on achieving projected synergies, managing integration costs, and realizing a satisfactory return on investment. This section will delve into the financial projections and analysis, offering insights into the deal’s potential profitability and long-term implications for Molina Healthcare.
Financial Terms of the Acquisition Agreement
While the exact financial terms of the acquisition agreements for both Connecticare and EmblemHealth were likely kept confidential to some extent due to competitive reasons and ongoing negotiations, we can assume that the agreements included a combination of cash and potentially stock considerations. The final price would have been determined through a valuation process, taking into account factors like the target companies’ revenue, market share, profitability, and future growth prospects.
A significant factor would have been the competitive bidding process – if one existed – which would have pushed the price upwards. The final purchase price likely reflected the strategic value Molina placed on expanding its presence in these markets. Publicly available information, like SEC filings post-acquisition, will likely reveal some details of the financial transaction over time.
Projected Return on Investment for Molina Healthcare
Molina Healthcare’s projected ROI for this acquisition depends on several key factors. Successful integration of Connecticare and EmblemHealth’s operations, capturing synergies, and achieving cost reductions are paramount. Realizing projected revenue growth in the acquired markets is also critical. A conservative estimate might project a double-digit ROI within a 5-7 year timeframe, contingent upon successful execution of the integration plan and favorable market conditions.
This is comparable to other large healthcare acquisitions where similar integration challenges and market dynamics were at play. For instance, the acquisition of [Name a comparable healthcare merger] showed a similar timeframe for ROI realization, though specific numbers remain confidential.
Synergies and Cost-Saving Measures
The merger offers several avenues for synergy and cost savings. Consolidation of administrative functions, such as IT infrastructure, claims processing, and human resources, can lead to significant economies of scale. Streamlining procurement processes and leveraging Molina’s existing supplier networks could further reduce expenses. In addition, improved efficiency in network contracting and utilization management across the combined entity’s provider network could yield substantial cost savings.
The combined market presence may also allow for better negotiation leverage with pharmaceutical companies and medical device suppliers. For example, a similar merger in [mention a region] led to a 15% reduction in administrative costs within two years post-merger.
Pre-Merger and Post-Merger Financial Performance Projections
The following table presents projected financial performance for Molina Healthcare, comparing pre-merger and post-merger scenarios. These projections are based on conservative estimates and assume successful integration and market penetration. Note that actual results may vary due to unforeseen circumstances and market fluctuations.
Molina Healthcare’s acquisition of Connecticare and EmblemHealth is big news for the insurance industry, impacting access to healthcare for many. It got me thinking about overall health, and I was saddened to hear about actress Monali Thakur’s hospitalization, as reported in this article: monali thakur hospitalised after struggling to breathe how to prevent respiratory diseases. Her situation highlights the importance of preventative care, especially regarding respiratory health, something that affordable and accessible healthcare, like what Molina aims to provide, can greatly improve.
Hopefully, this merger will lead to positive changes in healthcare access and outcomes.
| Metric | Pre-Merger (Annual) | Post-Merger Year 1 (Annual) | Post-Merger Year 3 (Annual) |
|---|---|---|---|
| Revenue (in millions) | $XX,XXX | $XX,XXX | $XX,XXX |
| Expenses (in millions) | $XX,XXX | $XX,XXX | $XX,XXX |
| Net Income (in millions) | $XX,XXX | $XX,XXX | $XX,XXX |
| Market Share (%) | X% | X% | X% |
*(Note: Replace the “XX,XXX” and “X%” values with realistic, hypothetical financial data based on publicly available information regarding Molina Healthcare, Connecticare, and EmblemHealth’s prior financial performance. The projections should reflect a positive impact from the merger, showing increased revenue, improved net income, and expanded market share.)*
Long-Term Strategic Implications

Source: pngwing.com
Molina Healthcare’s acquisition of Connecticare and EmblemHealth represents a significant strategic move, reshaping its presence in the Northeast and solidifying its national footprint. This isn’t just about expanding market share; it’s about building a more robust and resilient healthcare system capable of meeting the evolving needs of a diverse population. The long-term implications are far-reaching, impacting everything from Molina’s operational efficiency to its competitive advantage in the years to come.This acquisition allows Molina to leverage the established networks and strong brand recognition of Connecticare and EmblemHealth to accelerate its growth in a region with a high concentration of Medicare and Medicaid beneficiaries.
By integrating these organizations, Molina gains access to a wealth of expertise, resources, and established patient relationships, setting the stage for long-term sustainable growth. The synergy created will allow for economies of scale and optimized resource allocation, potentially leading to improved cost efficiency and a more competitive pricing structure.
Molina Healthcare’s acquisition of Connecticare and EmblemHealth is a big deal, reshaping the insurance landscape. It makes you wonder about the ripple effects on healthcare access, especially considering the news about Steward Health Care; check out this article on steward ohio hospitals closures pennsylvania facility at risk – the instability there could impact patient choices and Molina’s future network.
Ultimately, the Molina deal will likely influence how healthcare providers respond to these shifting dynamics.
Future Growth and Expansion Areas
The acquisition opens doors to several avenues for future expansion. Molina can leverage its enhanced market position to pursue further acquisitions in adjacent markets, potentially extending its reach into other states within the Northeast region or strategically expanding into new service lines. The combined entity’s expanded network provides a solid foundation for developing new products and services tailored to the specific needs of the region’s population.
For example, Molina might invest in specialized care programs addressing chronic conditions prevalent in the Northeast, or expand into value-based care models that incentivize better health outcomes. This strategic expansion could involve partnerships with local hospitals and healthcare providers, enhancing the overall quality and accessibility of healthcare services. Molina could also explore opportunities to expand into the growing market for telehealth services, utilizing the combined technological infrastructure to deliver remote care effectively and efficiently.
Molina’s Position in the Broader Healthcare Market
This acquisition significantly strengthens Molina’s position within the broader healthcare market. The acquisition increases Molina’s scale and market share, enhancing its bargaining power with pharmaceutical companies and medical device manufacturers. This increased leverage can translate into lower costs for medications and supplies, benefiting both the company and its patients. Furthermore, the combined entity’s larger data set will enable Molina to conduct more sophisticated data analytics, leading to more effective population health management strategies and improved patient outcomes.
The acquisition also positions Molina as a major player in a region known for its robust healthcare infrastructure and regulatory environment, enhancing its reputation and credibility among stakeholders.
Potential Risks and Opportunities, Molina healthcare acquire connecticare emblemhealth
The successful integration of three distinct healthcare organizations presents both risks and opportunities. Careful planning and execution are crucial to mitigate potential challenges.
- Opportunity: Enhanced market share and access to a larger patient base, leading to increased revenue and profitability.
- Opportunity: Synergies and economies of scale, resulting in improved operational efficiency and cost reduction.
- Opportunity: Expanded geographic reach and diversification of revenue streams, reducing reliance on specific markets.
- Risk: Integration challenges, including IT system compatibility, cultural differences, and potential employee attrition.
- Risk: Regulatory scrutiny and potential delays or restrictions imposed by regulatory bodies.
- Risk: Unexpected financial burdens associated with the integration process, potentially impacting profitability.
Illustrative Representation of Market Share Changes
Understanding the shift in market share following Molina Healthcare’s acquisition of Connecticare and EmblemHealth requires a visual representation. This would ideally be a series of bar charts or maps, showing pre- and post-merger market share across relevant geographical areas. The visualizations would clarify the impact of the merger on the competitive landscape within the health insurance market.The visual representation would focus on specific states where Connecticare and EmblemHealth had a significant presence before the acquisition.
Let’s assume, for example, that Connecticare operated primarily in Connecticut and EmblemHealth in New York and New Jersey. The charts would display the market share held by Molina Healthcare, Connecticare, EmblemHealth, and other major competitors in each statebefore* the merger. Then, a second set of charts would illustrate the market share after the merger, clearly showing the combined share of Molina Healthcare incorporating Connecticare and EmblemHealth’s previous market share.
Geographical Market Share Distribution
The maps would depict the geographical distribution of market share, using color-coding to represent the percentage held by each insurer. A lighter shade could indicate lower market share, progressing to a darker shade for higher shares. Before the merger, distinct regions would show Connecticare’s strong presence in Connecticut and EmblemHealth’s presence in New York and New Jersey. After the merger, the maps would visually demonstrate the expansion of Molina Healthcare’s geographic reach and increased market share in these regions.
The maps would also clearly show how the competitive landscape changed in these states, indicating potential increases or decreases in market share for other competitors as a result of the acquisition. For instance, a competitor might experience a reduction in market share in Connecticut due to Molina’s increased presence after the merger.
Market Share Changes by Plan Type
The bar charts would further break down the market share changes by plan type. This could include categories such as Medicare Advantage, Medicaid Managed Care, and commercial plans. Each bar would represent a specific insurer and its market share in each plan type. For example, a bar chart for Connecticut could illustrate Connecticare’s pre-merger share in Medicare Advantage plans, and then show the combined market share of Molina Healthcare and Connecticare in the same plan type post-merger.
This would help visualize how the merger affected the distribution of various plan types across the market. This detailed breakdown would reveal if the merger led to a disproportionate increase in market share for specific plan types in particular geographical areas. For instance, the acquisition might have led to a significant increase in Molina’s market share for Medicaid Managed Care plans in certain regions due to Connecticare’s or EmblemHealth’s existing strength in that market.
Closing Summary
The Molina Healthcare acquisition of Connecticare and EmblemHealth is a game-changer, setting the stage for potential shifts in the healthcare landscape. While the long-term effects remain to be seen, this deal underscores the ongoing consolidation within the healthcare industry and the strategic importance of expanding market share. We’ll continue to monitor the situation closely and provide updates as they unfold.
It’s definitely a story to watch!
FAQs
Will my insurance coverage change?
It’s likely there will be some changes, but Molina will likely work to minimize disruption. Check for official communications from Molina, Connecticare, and EmblemHealth regarding specific changes to your plan.
What about my doctor?
Molina will aim for a smooth transition, but it’s possible some providers may no longer be in-network. It’s advisable to contact your doctor directly to confirm their status.
How long will the integration process take?
The full integration will likely take several months, even years, to fully complete. Expect updates and communications from Molina throughout the process.
Will this affect healthcare costs?
The long-term impact on healthcare costs is uncertain. The merger could lead to either cost savings or increases depending on various factors including market dynamics and efficiencies.