Federal Nurse Staffing Ratios Bill Reintroduced
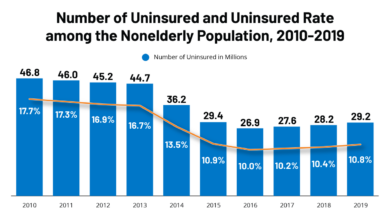
Federal Nurse Staffing Ratios Bill Reintroduced: The fight for better patient care and improved working conditions for nurses is back in the spotlight. This bill, reintroduced after previous attempts, aims to mandate specific nurse-to-patient ratios across the nation. This move has ignited a passionate debate, pitting the potential benefits of improved patient safety and reduced nurse burnout against concerns about the financial burden on hospitals and the challenges of implementation.
Let’s dive into the details and explore the arguments on both sides.
This post will examine the key provisions of the bill, tracing its legislative journey and comparing it to previous versions. We’ll weigh the arguments for and against mandatory ratios, considering their impact on nurses, hospitals, and patients. We’ll also explore international practices and potential alternative solutions to address nurse shortages and improve healthcare quality. Get ready for a comprehensive look at this crucial piece of legislation.
Bill Overview and History
Source: ytimg.com
The reintroduction of the federal nurse staffing ratios bill marks another significant step in the ongoing fight for improved patient care and safer working conditions for nurses. This legislation aims to address the persistent problem of understaffing in hospitals and healthcare facilities across the nation, a problem exacerbated by the recent pandemic and ongoing healthcare worker shortages. The bill’s history is a long and winding road, reflecting the complexities of navigating the legislative process and the powerful lobbying efforts of various stakeholders.The key provisions of the reintroduced bill generally mandate minimum nurse-to-patient ratios in hospitals, varying by unit type (e.g., intensive care units would have stricter ratios than medical-surgical units).
Specific ratios would be determined based on patient acuity and other relevant factors, aiming to ensure adequate nursing care for all patients. The bill also typically includes provisions for enforcement mechanisms, penalties for non-compliance, and funding mechanisms to support hospitals in meeting the mandated ratios. The exact details may vary slightly depending on the specific version of the bill.
Legislative History of the Bill
Previous attempts to pass federal nurse staffing ratios legislation have faced significant hurdles. The bill has been introduced in various forms over the years, often encountering opposition from hospital associations concerned about the potential financial burden of increased staffing costs. While several states have already implemented their own nurse staffing ratio laws, creating a patchwork of regulations across the country, a federal mandate aims for national consistency and equity.
Past versions of the bill often stalled in committee or failed to garner enough support to pass through both chambers of Congress. The reasons for these failures often included concerns about the cost of implementation, the potential impact on hospital budgets, and questions about the feasibility of enforcing such a mandate across the diverse healthcare landscape.
Comparison with Previous Iterations
While the core principle of establishing minimum nurse-to-patient ratios remains consistent across all versions of the bill, there have been notable differences in specific provisions. For example, earlier versions might have had stricter or less flexible ratios, or different enforcement mechanisms. Some iterations may have included provisions for funding assistance to help hospitals adjust to the new staffing requirements, while others may have focused solely on the mandate itself.
The reintroduction of the federal nurse staffing ratios bill is a huge step towards better patient care, but it also highlights the broader issue of healthcare access. Improving nurse-to-patient ratios is directly linked to better health outcomes, and this intersects with the amazing work being done by Rene Quashie and the Consumer Technology Association, as highlighted in this article on the AIS health equity revolution.
Ultimately, both initiatives aim to create a healthier future, one where equitable access to quality care is a reality for everyone. Stronger staffing ratios are key to achieving that goal.
The current version likely reflects compromises made in response to previous criticisms and attempts to build broader support among lawmakers. For instance, it might offer more flexibility in ratio calculations or include more robust funding mechanisms compared to its predecessors.
Timeline of Significant Events
A detailed timeline would require access to specific legislative records, but a general Artikel might look like this:
- [Year]: Initial introduction of a federal nurse staffing ratios bill in Congress.
- [Year]: Bill passes in the [House/Senate], but fails to advance in the other chamber.
- [Year]: Subsequent reintroduction of the bill with modifications.
- [Year]: Hearings and debates on the bill in relevant Congressional committees.
- [Year]: Bill fails to pass due to [reason, e.g., lack of support, procedural issues].
- [Year]: Current reintroduction of the bill.
Arguments for the Bill
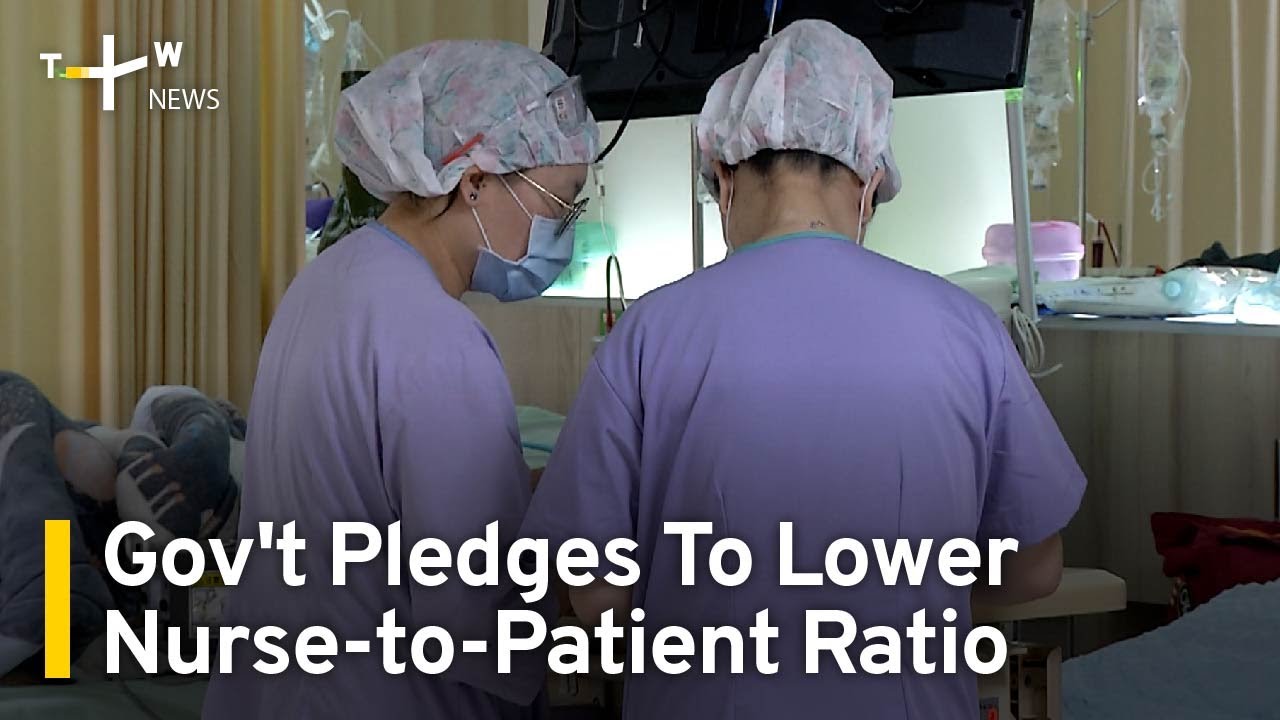
This bill advocating for federally mandated nurse staffing ratios aims to address a critical issue in healthcare: the persistent shortage of nurses and its direct impact on patient safety and well-being. Proponents argue that establishing minimum staffing ratios isn’t just about numbers; it’s about fundamentally improving the quality of care patients receive and the working conditions of nurses themselves.
Improved Patient Care
Numerous studies have demonstrated a strong correlation between lower nurse-to-patient ratios and poorer patient outcomes. Higher ratios are linked to increased rates of medication errors, hospital-acquired infections, and patient mortality. This bill aims to mitigate these risks by ensuring adequate nursing staff is available to provide timely and effective care. For example, a study published in the American Journal of Nursing found that hospitals with lower nurse-to-patient ratios experienced significantly higher rates of patient falls and pressure ulcers.
By mandating safer ratios, we can expect a reduction in these preventable adverse events, leading to improved patient safety and better health outcomes.
Reduced Nurse Burnout and Increased Job Satisfaction
Chronic understaffing forces nurses to work longer hours, handle heavier workloads, and compromise the quality of care they provide. This leads to immense stress, burnout, and high turnover rates. The proposed bill directly addresses this by providing nurses with the support they need to deliver safe and effective care without being overwhelmed. A reduction in workload and improved working conditions can translate to increased job satisfaction, reduced stress, and a more stable nursing workforce.
The reintroduction of the federal nurse staffing ratios bill is a huge step forward for patient care, but it also highlights the broader healthcare spending picture. We need to consider the escalating costs, like those detailed in this insightful KFF report on Medicare GLP-1 spending on weight loss , to ensure sustainable improvements in our healthcare system.
Ultimately, adequate nurse staffing and responsible cost management go hand-in-hand for better patient outcomes.
This, in turn, can lead to improved patient care as experienced and dedicated nurses are less likely to leave the profession. Imagine a scenario where a nurse, instead of rushing between patients, has the time to provide individualized care and build rapport – this is the direct impact of adequate staffing.
Impact on Hospital Finances and Operations
While some argue that mandated staffing ratios will increase hospital costs, proponents counter that the long-term benefits outweigh the initial investment. The cost of preventable medical errors, lawsuits related to negligence, and high staff turnover far exceeds the cost of employing additional nurses. Moreover, improved patient outcomes, reduced hospital readmissions, and a more stable workforce can lead to significant cost savings in the long run.
For instance, reducing hospital-acquired infections alone can generate substantial savings for hospitals. While initial implementation might require adjustments in hospital budgets, the overall financial impact is expected to be positive in the long term, resulting in a more efficient and effective healthcare system.
Projected Benefits vs. Potential Costs
| Benefit | Potential Cost | Example/Real-Life Case | Long-Term Impact |
|---|---|---|---|
| Improved patient safety (reduced medical errors, infections) | Increased staffing costs | Studies showing correlation between lower nurse-to-patient ratios and higher rates of hospital-acquired infections. | Reduced healthcare costs associated with treating preventable complications. |
| Reduced nurse burnout and turnover | Higher initial payroll expenses | Hospitals with better nurse staffing reporting lower turnover rates and improved employee satisfaction. | Reduced recruitment and training costs, increased workforce stability. |
| Shorter hospital stays | Increased labor costs | Research indicating that adequate nurse staffing leads to more efficient patient care and faster recovery times. | Improved hospital bed availability and reduced operational expenses. |
| Increased patient satisfaction | Potential need for facility expansion or renovation (in some cases) | Surveys demonstrating the positive correlation between nurse staffing levels and patient satisfaction scores. | Enhanced hospital reputation and increased patient volume. |
Arguments Against the Bill
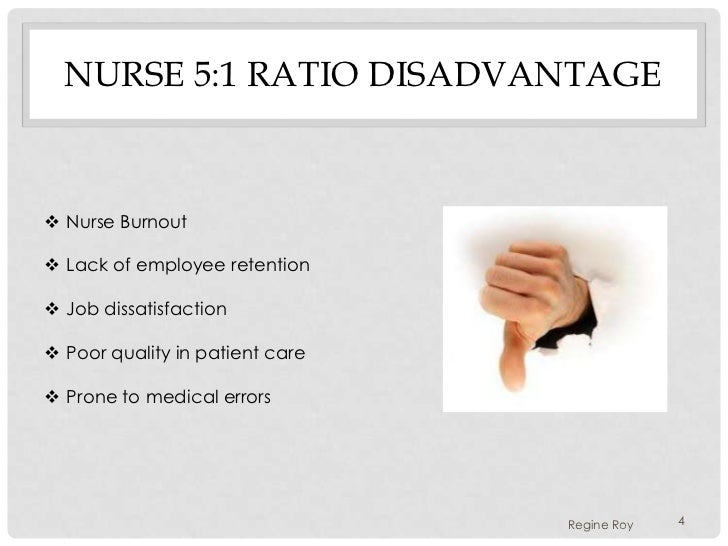
Source: slidesharecdn.com
While the intention behind mandatory nurse-to-patient ratios is laudable – aiming to improve patient safety and quality of care – a closer examination reveals potential drawbacks and unintended consequences that warrant careful consideration. Implementing such a law is a complex undertaking with significant challenges, and its impact may vary considerably depending on the healthcare setting.Implementing mandatory nurse-to-patient ratios presents several significant challenges.
One major concern is the potential for increased healthcare costs, both directly and indirectly. Direct costs include the need to hire significantly more nurses, leading to increased payroll expenses. Indirect costs could arise from potential reductions in other areas of hospital spending due to budgetary constraints. For example, hospitals might postpone investments in new equipment or technology to offset the increased nursing costs.
This could negatively impact the overall quality of care in the long run, despite improved nurse-to-patient ratios.
Increased Healthcare Costs and Budgetary Strain
The financial burden of complying with mandatory ratios could be particularly challenging for smaller hospitals and those in rural areas, potentially forcing some to close or reduce services. Larger, urban hospitals with greater financial resources might be better equipped to absorb these costs, leading to disparities in access to care. For example, a rural hospital with limited patient volume might struggle to justify the added expense of hiring additional nurses to meet a mandated ratio, even if it means potentially compromising patient safety.
The reintroduction of the federal nurse staffing ratios bill is a huge step towards improving patient care, but it also highlights the broader need for medical advancements. This is especially true when you consider groundbreaking news like the FDA’s approval of clinical trials for pig kidney transplants in humans, as reported by this article. Ultimately, both initiatives aim to alleviate suffering and improve health outcomes, underscoring the importance of both legislative action and medical innovation.
In contrast, a large urban hospital with a high patient volume might more easily absorb the increased costs. This could exacerbate existing healthcare disparities between urban and rural communities.
Challenges in Enforcement and Compliance
Effectively enforcing mandatory nurse-to-patient ratios presents a significant challenge. Monitoring compliance across various healthcare facilities would require a robust and extensive oversight system. Determining appropriate ratios for different patient populations and specialties would also be complex and require careful consideration of various factors, such as patient acuity and the complexity of care required. For instance, a surgical unit would require different ratios than a medical unit, and the ratio needed for a patient in critical care would differ from that of a patient recovering from a minor procedure.
Creating a standardized system that accurately accounts for these differences while ensuring equitable enforcement across all facilities would be a monumental task.
Potential for Unintended Consequences
The implementation of mandatory ratios could lead to several unintended consequences. One concern is the potential for increased wait times for patients seeking admission or care. If hospitals are unable to staff according to the mandated ratios, they may have to restrict admissions or delay procedures, leading to longer wait times and potentially impacting patient outcomes. Another potential consequence is the potential for increased nurse burnout.
While the ratios aim to reduce workload per nurse, they could instead lead to increased stress due to the rigid structure and potential difficulty in adjusting to unexpected surges in patient volume or changes in patient acuity. This could result in higher nurse turnover rates, defeating the purpose of improving patient care by leading to staff shortages.
Impact on Rural versus Urban Hospitals
The impact of mandatory nurse-to-patient ratios is likely to differ significantly between rural and urban hospitals. Rural hospitals, often facing challenges with recruitment and retention of nurses, may find it particularly difficult to meet mandated ratios. This could lead to staff shortages, service reductions, or even hospital closures in rural areas, exacerbating existing healthcare disparities. Urban hospitals, with typically larger staffing pools and greater financial resources, might be better positioned to meet the requirements, although they may still face significant cost increases.
This disparity in the ability to comply with the ratios could further widen the gap in access to quality healthcare between rural and urban populations. The potential for rural hospitals to struggle with the increased financial and staffing demands of the law presents a significant concern.
Impact on Different Stakeholders
The reintroduction of the federal nurse staffing ratios bill promises significant changes across the healthcare landscape. Its impact will be felt differently by various stakeholders, each experiencing both potential benefits and drawbacks. A thorough examination of these effects is crucial for a balanced understanding of the bill’s potential consequences.
Impact on Nurses
The proposed legislation aims to directly improve working conditions for nurses. Mandatory staffing ratios would mean fewer patients per nurse, reducing workload and stress levels. This could lead to improved patient care, decreased burnout, and potentially higher job satisfaction. However, the implementation might also lead to increased pressure to meet specific ratios, potentially causing stress in different ways, such as increased pressure to complete tasks within shorter timeframes.
Furthermore, depending on the specifics of the bill, it could also impact nurses’ autonomy in patient assignment, or it might lead to increased competition for positions in hospitals that meet the new staffing standards.
Impact on Hospital Administrators and Management
For hospital administrators, the bill presents a complex challenge. Meeting mandated staffing ratios will require significant financial investment, potentially impacting budgets and profitability. This could necessitate increased healthcare costs, potentially passed on to patients or insurers. However, the improved patient outcomes and reduced nurse burnout could lead to lower turnover rates and reduced recruitment costs in the long run.
Administrators may also need to reassess existing workflow processes and resource allocation to comply with the new regulations. This could necessitate changes to hospital layouts, technology adoption, and management strategies.
Impact on Patients and Their Families
Patients are arguably the most directly affected by nurse staffing levels. The bill aims to improve patient safety and quality of care by reducing nurse workloads and increasing the time nurses can spend with each patient. This could lead to improved patient outcomes, fewer medical errors, and faster recovery times. For families, this translates to peace of mind knowing their loved ones are receiving adequate attention and care.
However, the potential increase in healthcare costs associated with the bill could impact patient access to care, particularly for those with limited insurance coverage or those in underserved communities.
Impact on the Healthcare Industry as a Whole
The bill’s impact on the healthcare industry will be far-reaching. It could set a precedent for other states to adopt similar legislation, leading to a nationwide shift in nurse staffing practices. This could stimulate investment in healthcare technology to improve efficiency and support nurses’ workload. However, the increased costs associated with higher nurse-to-patient ratios could strain the already burdened healthcare system, potentially leading to hospital closures or mergers in some areas.
The long-term effects on the industry’s financial stability and its ability to provide equitable access to care remain to be seen. For example, smaller rural hospitals might face disproportionate challenges in meeting the new requirements compared to larger urban facilities.
Comparable Legislation and International Practices: Federal Nurse Staffing Ratios Bill Reintroduced
The debate surrounding mandated nurse staffing ratios in the United States isn’t isolated. Many other states and countries have grappled with similar issues, implementing various approaches with varying degrees of success. Examining these international and interstate examples provides valuable context for understanding the potential impacts of the proposed federal bill. By comparing different legislative models and their outcomes, we can better predict the likely effects of a nationwide mandate in the US.
Nurse Staffing Ratio Legislation in Other States
California’s landmark legislation, enacted in 1999, stands as a prominent example of state-level nurse staffing ratio mandates. This law specifies minimum nurse-to-patient ratios for various units in hospitals. While the implementation faced challenges, including legal battles and concerns about cost, it has influenced subsequent legislation in other states. For instance, several states have considered or adopted similar, though often less stringent, regulations.
These variations highlight the complexities of implementing such mandates, which depend on factors like hospital size, type of facility, and available resources. The experience of these states offers valuable lessons on effective implementation strategies, potential pitfalls, and the long-term effects on patient outcomes and healthcare costs.
International Approaches to Nurse Staffing
Several countries have implemented national policies or guidelines regarding nurse staffing. Australia, for example, has a national competency framework for nurses, although specific nurse-to-patient ratios are generally determined at the state or hospital level. In contrast, some European countries have adopted more centralized approaches. The UK’s National Health Service (NHS) has implemented national guidelines and standards for nurse staffing, although the specific ratios can vary across different NHS trusts and hospital departments.
These differing approaches reflect the diverse healthcare systems and contexts in various countries. A key consideration is the level of government control and the degree of flexibility afforded to individual hospitals in setting their own staffing levels.
Comparison of International Approaches to Nurse Staffing Ratios
| Country/Region | Approach | Level of Mandate | Key Features |
|---|---|---|---|
| California, USA | Mandated ratios | State-level | Specific ratios for different units; ongoing legal and cost challenges |
| Australia | National competency framework | National, but ratios set locally | Focus on skill and competency, not strict ratios; variations across states and hospitals |
| United Kingdom (NHS) | National guidelines and standards | National, but implementation varies | Recommendations rather than strict mandates; variations across trusts and departments |
| European Union (varies by country) | Mixed approaches | National or regional | Ranges from national mandates to more flexible guidelines; significant variations in implementation |
Potential Solutions and Alternatives

Source: whyy.org
Mandating nurse-to-patient ratios is a complex issue with significant implications. While proponents argue for improved patient safety and nurse well-being, opponents raise concerns about cost, feasibility, and potential unintended consequences. Exploring alternative strategies and potential modifications to the proposed bill is crucial for finding a balanced solution that addresses the core problem: nurse shortages and suboptimal patient care.
Alternative Strategies for Addressing Nurse Shortages, Federal nurse staffing ratios bill reintroduced
Addressing the nurse shortage requires a multi-pronged approach that goes beyond simply mandating ratios. Increasing nursing school capacity, offering loan forgiveness programs, and improving working conditions to reduce burnout are all critical components. For example, increasing the number of clinical training positions in underserved areas could incentivize nurses to work in those locations, directly addressing regional disparities in staffing.
Similarly, a comprehensive loan forgiveness program specifically targeting nurses working in high-demand specialties or underserved communities could significantly boost recruitment and retention.
Potential Compromises and Modifications to the Proposed Bill
A compromise might involve a phased implementation of nurse-to-patient ratios, starting with the most critical care areas and gradually expanding to others as resources allow. This would mitigate the immediate financial burden on healthcare facilities while still prioritizing patient safety in high-risk situations. Another modification could be to establish flexible ratios that adjust based on patient acuity, allowing for more nuanced staffing decisions.
This would acknowledge the varying levels of care required by different patients and avoid a rigid, one-size-fits-all approach. For instance, a surgical unit might require higher ratios post-operation compared to a less acute medical ward.
The Role of Technology in Improving Nurse Efficiency and Patient Outcomes
Technology offers significant potential for improving nurse efficiency and patient outcomes, thereby mitigating some of the pressures driving the need for strict staffing ratios. Telehealth, for example, can extend the reach of nurses, allowing them to monitor patients remotely and provide timely interventions. Electronic health records (EHRs) can streamline documentation, freeing up nurses’ time for direct patient care.
Automated medication dispensing systems can reduce medication errors and improve safety. Imagine a scenario where remote patient monitoring alerts nurses to potential problems before they escalate, enabling proactive intervention and potentially preventing hospital readmissions. This reduces the workload on nurses and improves patient outcomes. Furthermore, robotic assistance for physically demanding tasks could reduce nurse fatigue and injuries.
Conceptual Framework for an Alternative Approach to Nurse Staffing
An alternative approach could focus on a comprehensive system that prioritizes: 1) Increased nursing workforce supply through education and retention initiatives; 2) Improved efficiency and technology integration to optimize workload; 3) Patient-centered care models that prioritize patient acuity and needs; and 4) Data-driven decision-making to assess staffing needs dynamically. This framework moves away from a purely ratio-based approach to a more holistic strategy that addresses the underlying causes of the nurse shortage and aims for optimal patient care through a combination of increased staffing, technological advancements, and efficient care delivery models.
For example, a hospital could utilize predictive analytics to forecast staffing needs based on patient admissions and acuity levels, ensuring optimal staffing levels without resorting to rigid, potentially inflexible ratios.
Illustrative Scenarios
This section presents two contrasting scenarios to highlight the potential impacts of the federal nurse staffing ratios bill – one showcasing positive outcomes and the other illustrating potential negative consequences. These scenarios are fictional but based on real-world hospital challenges and potential solutions.
Positive Impact on Patient Care: County General Hospital
Before the implementation of the mandated nurse-to-patient ratios, County General Hospital, a large public hospital serving a diverse, low-income population, consistently struggled with high patient-to-nurse ratios. Nurses frequently reported feeling overwhelmed, leading to increased burnout and higher turnover rates. Patient care suffered as a result; medication errors increased, and patients experienced longer wait times for basic needs like pain medication and assistance with toileting.
Post-operative care was often rushed, leading to a higher incidence of post-surgical complications. For example, a single nurse might be responsible for six post-operative patients requiring frequent monitoring and medication administration. This often resulted in delays in recognizing and addressing complications.After the implementation of the bill, County General hired additional nurses to meet the mandated ratios. The immediate impact was a noticeable reduction in nurse burnout and an improvement in staff morale.
Patient outcomes also improved significantly. Medication errors decreased by 25%, according to internal hospital data, and patient satisfaction scores rose by 15%, as reported in patient satisfaction surveys. Post-operative complications also dropped by 10%. The improved nurse-patient ratio allowed for more individualized care, timely medication administration, and proactive monitoring, resulting in better patient safety and overall improved health outcomes.
The hospital also saw a decrease in nurse turnover, reducing recruitment and training costs.
Negative Consequences: St. Jude’s Private Hospital
St. Jude’s Private Hospital, a smaller, specialized facility focused on cardiac care, operated with consistently low patient-to-nurse ratios even before the bill’s implementation. They had a highly skilled and experienced nursing staff, and their existing staffing model prioritized individualized care. The hospital’s financial model, however, relied on a delicate balance between high-quality care and profitability.Following the implementation of the bill, St.
Jude’s was forced to significantly increase its nursing staff to meet the mandated ratios, even though their existing staffing levels were already considered optimal. This resulted in a substantial increase in operational costs, impacting the hospital’s bottom line. While patient care remained high-quality, the increased staffing costs led to a reduction in other essential services, such as advanced equipment upgrades and investment in new technologies.
The hospital had to raise patient fees to offset the increased costs, potentially impacting accessibility for some patients. In addition, the hospital had to reduce its investment in research and development activities. This illustrates a potential trade-off between ensuring mandated staffing ratios and maintaining the financial viability of specialized healthcare facilities.
Last Point
The reintroduction of the federal nurse staffing ratios bill is a significant development with far-reaching implications. While the promise of improved patient care and reduced nurse burnout is enticing, the potential challenges of implementation and financial strain on healthcare systems cannot be ignored. The debate highlights the complex interplay between patient safety, healthcare economics, and the well-being of the nursing workforce.
Ultimately, finding a solution that balances these competing interests will require careful consideration and a commitment to collaborative problem-solving. The journey towards a better future for nurses and patients continues.
FAQ Corner
What are the potential penalties for hospitals that fail to meet the mandated nurse-to-patient ratios?
The bill likely Artikels specific penalties, potentially including fines or other sanctions. The exact details would need to be examined within the text of the bill itself.
How might this bill impact rural hospitals differently than urban hospitals?
Rural hospitals, often facing staffing shortages and limited resources, might struggle more to meet the mandated ratios compared to their urban counterparts. The bill might need to include provisions addressing the unique challenges faced by rural healthcare facilities.
Will this bill address the root causes of nurse shortages?
While the bill addresses immediate staffing concerns, it’s unlikely to fully resolve underlying issues like nurse education and training pipelines, competitive salaries, and overall working conditions. Addressing those root causes would require a multifaceted approach.