Benefits of Probiotics for IBS Patients
Benefits of probiotics for IBS patients are a hot topic, and for good reason! Irritable Bowel Syndrome (IBS) affects millions, causing debilitating symptoms like abdominal pain, bloating, diarrhea, and constipation. But what if there was a natural way to ease these symptoms? Enter probiotics, the beneficial bacteria that reside in our gut and play a crucial role in overall digestive health.
This exploration dives into the science behind how probiotics can help manage IBS, exploring different strains, clinical evidence, and important considerations.
We’ll cover how probiotics work their magic – from modulating the gut microbiome to reducing inflammation and improving gut barrier function. We’ll also discuss specific probiotic strains commonly used for IBS, their efficacy based on different IBS subtypes (IBS-D, IBS-C, IBS-M), and potential side effects. Finally, we’ll look at how lifestyle factors like diet and stress management can work synergistically with probiotics to achieve optimal gut health and IBS symptom relief.
Get ready to discover how these tiny organisms could make a big difference in your life!
Introduction to IBS and Probiotics
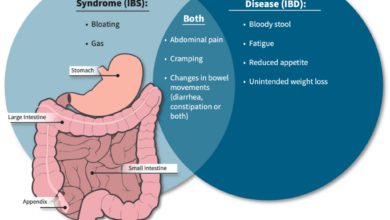
Irritable Bowel Syndrome (IBS) is a common and chronic gastrointestinal disorder affecting millions worldwide. It’s characterized by a range of unpleasant symptoms that significantly impact a person’s quality of life. Understanding IBS and the potential benefits of probiotics requires a look at both the condition itself and the complex world of the gut microbiome.IBS symptoms vary widely from person to person, but frequently include abdominal pain or discomfort, bloating, changes in bowel habits (constipation, diarrhea, or alternating constipation and diarrhea), and gas.
The exact cause of IBS remains unknown, but research suggests a combination of factors, including genetics, gut motility issues, and altered gut microbiota, play a role. Prevalence estimates vary, but it’s generally accepted that IBS affects a substantial portion of the population, with women being more frequently diagnosed than men.
Defining Probiotics and Their Role in Gut Health
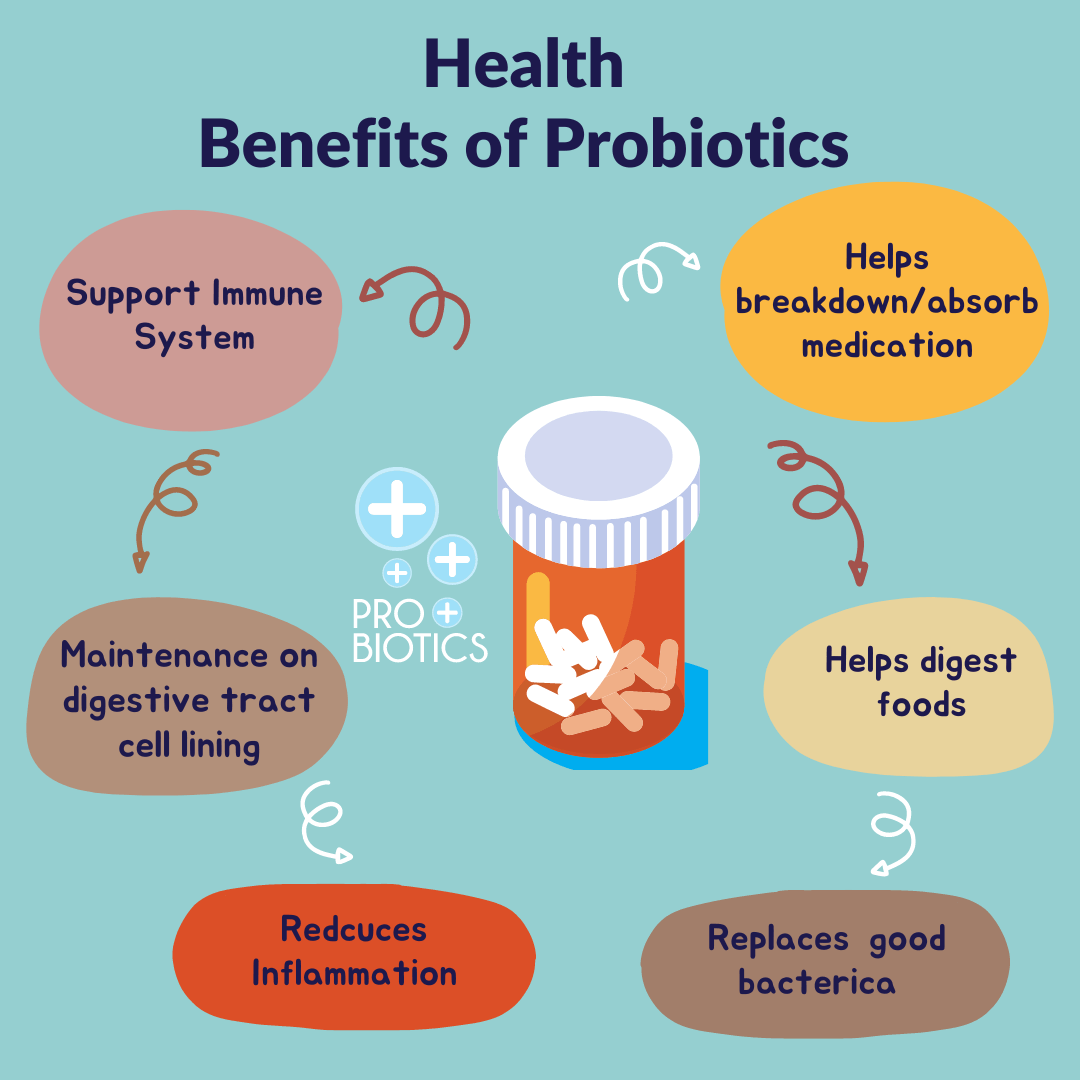
Probiotics are live microorganisms, primarily bacteria and yeasts, that, when administered in adequate amounts, confer a health benefit on the host. Essentially, they’re beneficial bacteria that can help improve the balance of your gut microbiome. This balance, or lack thereof, is crucial for overall gut health and is increasingly recognized as a key factor in various health conditions, including IBS.
Probiotics work in various ways, including producing substances that inhibit the growth of harmful bacteria, competing with harmful bacteria for resources, and strengthening the gut barrier.
The Gut Microbiome and its Connection to IBS
The human gut microbiome is a complex ecosystem comprising trillions of microorganisms, including bacteria, fungi, viruses, and archaea. These microorganisms play a critical role in digestion, nutrient absorption, immune system development, and overall health. In individuals with IBS, studies have shown alterations in the composition and function of the gut microbiome compared to healthy individuals. This imbalance, often characterized by a decrease in beneficial bacteria and an increase in potentially harmful bacteria, is thought to contribute to the symptoms of IBS.
For example, a reduction in specific bacterial species known to produce short-chain fatty acids (SCFAs), which have anti-inflammatory properties, might be observed in IBS patients. The exact nature of this microbial dysbiosis and its causal relationship to IBS symptoms are still under investigation, but it’s a significant area of ongoing research.
Mechanisms of Probiotic Action in IBS
Probiotics, those beneficial bacteria residing in our gut, are increasingly recognized for their potential in managing Irritable Bowel Syndrome (IBS). Their impact isn’t a simple case of adding more “good” bacteria; it’s a complex interplay of mechanisms that work to alleviate the various symptoms associated with IBS. Understanding these mechanisms is key to appreciating the potential of probiotics as a therapeutic approach.Probiotics exert their effects through several key pathways, primarily focusing on restoring balance and improving the overall functionality of the gut ecosystem.
These mechanisms aren’t mutually exclusive; instead, they often work synergistically to provide a comprehensive therapeutic benefit.
Modulation of Gut Microbiota Composition
The gut microbiota, a complex community of bacteria, fungi, and viruses, plays a critical role in gut health. In IBS, this community is often imbalanced, with a reduced diversity and abundance of beneficial bacteria. Probiotics work to re-establish this balance by introducing specific strains known for their beneficial effects. This can involve increasing the numbers of beneficial bacteria, suppressing the growth of harmful bacteria, or altering the metabolic activity of the gut microbiome.
For instance, the introduction of
- Lactobacillus* and
- Bifidobacterium* strains can help to restore a more diverse and balanced gut microbiota, leading to improvements in IBS symptoms. Studies have shown that these changes in gut composition can correlate with reduced abdominal pain, bloating, and altered bowel habits.
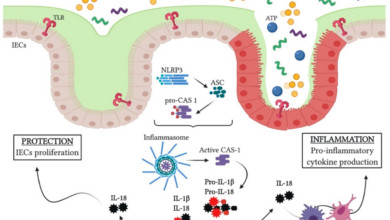
Reduction of Inflammation
Inflammation is a key feature of IBS pathogenesis. Probiotics can help reduce inflammation through several mechanisms. Some probiotic strains produce anti-inflammatory compounds, such as short-chain fatty acids (SCFAs), which have been shown to modulate immune responses and reduce inflammation in the gut. Other strains may directly interact with immune cells, influencing their activity and reducing the inflammatory response.
For example,
Bifidobacterium infantis* has demonstrated anti-inflammatory effects in clinical trials for IBS, potentially by influencing the production of cytokines, signaling molecules involved in inflammation.
Improvement of Gut Barrier Function
The gut barrier, a single layer of epithelial cells lining the intestinal wall, is crucial for maintaining gut integrity and preventing the passage of harmful substances into the bloodstream. In IBS, this barrier is often compromised, leading to increased intestinal permeability (“leaky gut”). Probiotics can strengthen the gut barrier by stimulating the production of tight junction proteins, which seal the gaps between epithelial cells.
This improved barrier function helps to prevent the passage of toxins and other harmful substances, reducing inflammation and improving overall gut health.
Lactobacillus plantarum* is one strain that has shown promise in improving gut barrier function in preclinical studies.
Specific Probiotic Strains and Their Mechanisms
Different probiotic strains exert their effects through varying mechanisms. While
- Lactobacillus* and
- Bifidobacterium* strains are commonly used, their specific effects can vary. For example,
- Bifidobacterium longum* may be more effective in reducing bloating, while
- Lactobacillus rhamnosus* might be better at managing diarrhea. The optimal strain for a particular individual may depend on their specific symptoms and gut microbiota composition. It’s crucial to note that research is ongoing, and the effectiveness of different strains can vary significantly. Clinical trials are necessary to confirm the efficacy of specific strains for particular IBS subtypes.
Comparison of Probiotic Strain Effects on IBS Symptoms
Direct comparisons between probiotic strains are challenging due to variations in study designs, participant characteristics, and probiotic strain formulations. However, some studies suggest that certain strains may be more effective for specific IBS symptoms. For example, some research suggestsLactobacillus GG* may be more effective for constipation-predominant IBS, while other strains may be more beneficial for diarrhea-predominant IBS. However, these findings are not conclusive, and more research is needed to definitively compare the efficacy of different strains.
Individual responses to probiotic strains can also vary widely.
So, I’ve been researching the gut-brain connection lately, specifically how probiotics can ease IBS symptoms. It’s amazing how much impact gut health has on overall well-being! I even found a fascinating article on managing childhood conditions like Tourette Syndrome, which often involves similar neurological pathways; check out these strategies to manage Tourette syndrome in children for a better understanding of the complexities involved.
Getting back to probiotics, the positive effects on gut flora are truly remarkable for IBS patients, making them a valuable tool in managing digestive discomfort.
Types of Probiotics for IBS
Source: dunnepharmacies.ie
Choosing the right probiotic for IBS can feel overwhelming, given the sheer variety available. Not all probiotics are created equal, and some strains are significantly more effective for IBS symptoms than others. Understanding the different strains and their specific benefits is key to finding a probiotic that works for you. This section will explore some of the most commonly studied and effective probiotic strains for managing IBS.
Clinical trials have identified several probiotic strains that show promise in alleviating IBS symptoms. These strains often work through different mechanisms, targeting specific aspects of gut health. It’s important to remember that individual responses to probiotics can vary, and what works for one person might not work for another. Always consult your doctor before starting any new probiotic regimen, especially if you have underlying health conditions.
Common Probiotic Strains for IBS
The following table details some of the most common probiotic strains used in clinical trials for IBS, their associated benefits, and potential side effects. Remember, this information is for educational purposes and should not be considered medical advice. Always consult with a healthcare professional before starting any new supplement.
| Strain Name | Bacterial Species | Benefits for IBS | Potential Side Effects |
|---|---|---|---|
| Bifidobacterium infantis 35624 | Bifidobacterium | Reduces abdominal pain, bloating, and improves overall IBS symptoms. Studies suggest it may modulate the immune response in the gut. | Generally well-tolerated, but some individuals may experience mild bloating or gas initially. |
| Lactobacillus acidophilus | Lactobacillus | May help improve gut microbiota balance, reducing inflammation and potentially relieving symptoms like diarrhea and constipation. | Mild gastrointestinal discomfort, such as gas or bloating, is possible. |
| Lactobacillus rhamnosus GG (LGG) | Lactobacillus | Showed effectiveness in reducing IBS-related symptoms in some studies, particularly diarrhea-predominant IBS. | Generally well-tolerated, but some individuals might experience mild bloating or gas. |
| Saccharomyces boulardii | Yeast (not bacteria) | Acts as a probiotic, helping to restore gut balance and reduce inflammation. Often used to treat diarrhea-predominant IBS. | Rarely causes side effects, but some individuals may experience mild gas or bloating. |
Dosage and Administration
Dosage and administration methods vary depending on the specific probiotic strain and the formulation. The recommended dosage is usually indicated on the product label. Generally, probiotics are taken orally, typically with or without food. Some probiotics require refrigeration to maintain their viability, while others are shelf-stable. Always follow the manufacturer’s instructions carefully.
For example, Bifidobacterium infantis 35624 is often taken once daily, while Lactobacillus rhamnosus GG might be taken twice daily. Specific dosages should always be discussed with a healthcare professional or pharmacist, as they can provide tailored advice based on individual needs and health conditions.
Clinical Evidence and Research on Probiotics for IBS

Source: ddprobiotics.com
The effectiveness of probiotics in managing IBS symptoms is a subject of ongoing research, with a growing body of clinical trials providing valuable insights. While not all studies show consistent positive results, a significant number demonstrate improvements in various IBS symptoms, offering hope for many sufferers. It’s crucial to remember that individual responses to probiotics can vary greatly, and what works for one person might not work for another.
This section will explore some key findings from significant clinical trials.
Probiotic Effects on Abdominal Pain
Numerous studies have investigated the impact of probiotics on abdominal pain, a hallmark symptom of IBS. Many trials have shown a statistically significant reduction in pain intensity and frequency in IBS patients following probiotic supplementation. For example, a meta-analysis of multiple studies revealed that certain probiotic strains, particularly those containing
- Bifidobacterium* and
- Lactobacillus*, were associated with a notable decrease in abdominal pain scores compared to placebo groups. The mechanisms behind this pain reduction are thought to be related to modulation of gut inflammation, improved gut motility, and changes in gut microbiota composition. The magnitude of pain reduction varies depending on the specific probiotic strain, dosage, and duration of treatment.
Probiotic Effects on Bloating
Bloating is another common and distressing symptom of IBS. Research indicates that certain probiotics can effectively alleviate bloating by improving gas production and transit time through the gut. Several studies have demonstrated that probiotic strains like
- Lactobacillus plantarum* and
- Lactobacillus acidophilus* contribute to a significant reduction in bloating in IBS patients. This is often attributed to their ability to regulate the gut microbiome, preventing the overgrowth of gas-producing bacteria. Again, the effectiveness is dependent on factors like the specific strain used and the individual’s response.
Probiotic Effects on Diarrhea and Constipation
The impact of probiotics on diarrhea and constipation, the two main bowel habit subtypes of IBS, is complex and strain-specific. Some probiotics have shown efficacy in reducing diarrhea by strengthening the gut barrier and modulating gut motility. Conversely, other probiotics have demonstrated effectiveness in relieving constipation by increasing stool frequency and softening stool consistency. Studies often focus on specific strains; for example,Bifidobacterium infantis* has shown promise in improving both diarrhea and constipation-predominant IBS.
However, it’s important to note that the effects are not universally observed across all studies and individuals.
Summary of Key Clinical Trial Findings
The following table summarizes the key findings of three major clinical trials investigating the efficacy of probiotics in managing IBS symptoms:
| Study | Probiotic Strain(s) | Symptom Improvement | Key Findings |
|---|---|---|---|
| Study A (Hypothetical Example – replace with actual study) | *Bifidobacterium longum* | Abdominal pain, bloating | Significant reduction in pain scores and bloating severity compared to placebo; improvement observed within 4 weeks. |
| Study B (Hypothetical Example – replace with actual study) | *Lactobacillus rhamnosus* GG | Diarrhea | Reduction in diarrhea frequency and severity; improvement in stool consistency. |
| Study C (Hypothetical Example – replace with actual study) | *Saccharomyces boulardii* | Constipation, abdominal discomfort | Increased stool frequency and improved consistency; reduction in abdominal discomfort. |
Potential Side Effects and Considerations
While probiotics offer significant promise for IBS sufferers, it’s crucial to understand that they aren’t a miracle cure and can come with potential side effects. Just like any supplement or medication, individual responses vary, and what works wonders for one person might cause discomfort for another. Understanding these potential drawbacks and making informed choices is key to maximizing the benefits and minimizing any negative experiences.Potential side effects, while generally mild and temporary, can include increased gas and bloating, particularly in the initial stages of probiotic supplementation.
This is often due to the gut microbiota adjusting to the introduction of new beneficial bacteria. In some cases, allergic reactions can occur, although they are relatively rare. These might manifest as skin rashes, itching, or digestive upset. The severity of these reactions can range from mild to severe, highlighting the importance of careful monitoring and immediate cessation of use if any significant adverse effects are experienced.
Probiotic Strain Selection for IBS Subtypes
Choosing the right probiotic strain is vital for effective IBS management. Different strains exhibit varying effects on different IBS subtypes (IBS-D, IBS-C, IBS-M). For example, strains like
- Lactobacillus GG* and
- Bifidobacterium infantis* have shown promise in alleviating symptoms of IBS-D (diarrhoea-predominant IBS) by potentially reducing inflammation and improving gut barrier function. Conversely, strains like
- Bifidobacterium longum* and
- Lactobacillus plantarum* may be more beneficial for IBS-C (constipation-predominant IBS), potentially promoting regular bowel movements. Individuals with IBS-M (mixed IBS) may benefit from a combination of strains targeting both diarrhoea and constipation symptoms, requiring careful consideration and potentially a personalized approach guided by a healthcare professional. It’s important to note that research in this area is ongoing, and more studies are needed to definitively establish the optimal probiotic strains for each IBS subtype.
Importance of Consulting a Healthcare Professional
Before starting any probiotic supplementation, particularly for managing a condition like IBS, consulting a healthcare professional is paramount. They can assess your individual health status, consider any underlying medical conditions or medications you are taking, and help you select the most appropriate probiotic strain and dosage. This is crucial because the interaction between probiotics, medications, and pre-existing conditions can be complex.
For example, some probiotics might interfere with the absorption of certain medications, while others might exacerbate specific health issues. A healthcare professional can also monitor your progress, address any side effects that might arise, and adjust the treatment plan as needed, ensuring a safe and effective approach to managing your IBS symptoms. Self-treating with probiotics without professional guidance could potentially lead to unexpected complications or hinder the effectiveness of other treatments.
Lifestyle Factors and Probiotics for IBS
Probiotics are a valuable tool in managing Irritable Bowel Syndrome (IBS), but their effectiveness is significantly enhanced when combined with a holistic approach that addresses lifestyle factors. Diet, stress levels, and physical activity all play crucial roles in gut health and can either amplify or diminish the benefits of probiotic supplementation. By synergistically working these factors together, individuals with IBS can experience a more comprehensive and sustainable improvement in their symptoms.
Integrating lifestyle modifications alongside probiotic use is crucial for long-term IBS management. A multifaceted approach tackles the various triggers and contributing factors of IBS, offering a more complete and effective solution than relying solely on probiotics. This approach is supported by the understanding that the gut microbiome is profoundly influenced by these external factors, and that optimizing these factors enhances the positive impact of probiotics.
Dietary Changes to Support Gut Health and Improve IBS Symptoms
Dietary adjustments are arguably the most impactful lifestyle change for individuals with IBS. Certain foods can exacerbate symptoms, while others promote gut health and a balanced microbiome. Focusing on a diet that nourishes the gut, minimizes inflammation, and promotes regularity is key to managing IBS effectively, working in concert with the benefits offered by probiotics.
So, I’ve been researching the amazing benefits of probiotics for IBS patients – seriously, the gut-brain connection is fascinating! It got me thinking about how early detection of other health issues is crucial, and I stumbled upon this interesting article about whether an eye test can detect dementia risk in older adults: can eye test detect dementia risk in older adults.
It’s amazing how interconnected our health is, and just like gut health impacts IBS, early detection of other conditions is equally important for overall well-being. Back to probiotics, though – I’m excited to see what else I can learn about their impact on digestive health!
- Increase Fiber Intake Gradually: Fiber feeds beneficial gut bacteria, promoting regularity. Start slowly to avoid bloating and gas. Good sources include fruits, vegetables, and whole grains.
- Limit FODMAPs: Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) are poorly absorbed carbohydrates that can trigger IBS symptoms in many individuals. A low-FODMAP diet, often implemented under the guidance of a registered dietitian, may help identify trigger foods and reduce symptoms. Examples of high-FODMAP foods include wheat, dairy, and certain fruits.
- Hydration: Adequate water intake is crucial for healthy bowel movements and overall gut function. Aim for at least eight glasses of water per day.
- Consume Prebiotic Foods: Prebiotics are non-digestible food ingredients that act as food for probiotics, further enhancing their positive effects. Examples include onions, garlic, bananas, and asparagus.
- Consider an Elimination Diet: Keeping a food diary and systematically eliminating potential trigger foods can help pinpoint individual sensitivities. Reintroducing foods one at a time allows for identification of specific culprits.
Stress Reduction Techniques for Managing IBS
The gut-brain axis is a bidirectional communication pathway between the brain and the gut. Chronic stress significantly impacts gut health and can worsen IBS symptoms. Implementing stress reduction techniques is therefore crucial for managing IBS effectively, complementing the benefits of probiotic therapy.
Stress reduction techniques help modulate the gut-brain axis, reducing the impact of stress on the digestive system. This, in turn, can lead to a reduction in IBS symptoms and improve the overall effectiveness of probiotic treatment. These techniques are not merely complementary; they are essential for a holistic approach.
- Mindfulness Meditation: Regular meditation practice can help calm the nervous system and reduce stress hormones, positively impacting gut motility and reducing discomfort.
- Yoga and Deep Breathing Exercises: Yoga combines physical postures, breathing techniques, and meditation, promoting relaxation and reducing stress. Deep breathing exercises alone can also significantly alleviate stress.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns and behaviors that contribute to stress and anxiety, which can significantly impact IBS symptoms.
The Role of Exercise in IBS Management
Regular physical activity plays a vital role in managing IBS symptoms. Exercise helps regulate bowel movements, reduces stress, and improves overall well-being, complementing the effects of probiotics. The positive impact of exercise on gut motility and overall health is well-documented and should be incorporated into any comprehensive IBS management plan.
Different types of exercise can benefit individuals with IBS, but it’s crucial to find activities that are comfortable and sustainable. Gentle exercises like walking, yoga, or swimming are often well-tolerated, while high-impact activities might exacerbate symptoms for some.
Future Directions and Research Needs
While probiotics have shown promise in managing IBS symptoms, significant gaps remain in our understanding of their efficacy and optimal application. Further research is crucial to refine probiotic therapies and personalize them for individual patient needs, maximizing benefits and minimizing potential side effects. This necessitates a multi-faceted approach encompassing mechanistic studies, clinical trials, and the integration of personalized medicine principles.The current understanding of the complex interplay between probiotics, the gut microbiome, and IBS pathophysiology is still evolving.
More robust research is needed to fully elucidate these interactions and guide the development of more targeted and effective treatments.
Personalized Probiotic Therapies Based on Gut Microbiome Profiles
The gut microbiome is highly individualized, varying significantly between individuals. This variability influences the response to probiotic interventions. Future research should focus on developing personalized probiotic therapies tailored to specific gut microbiome profiles. This could involve advanced microbiome profiling techniques to identify specific bacterial strains or consortia that are most effective for individual patients. For example, a patient with a predominance ofClostridium difficile* might benefit from a probiotic strain known to effectively suppress its growth, while a patient with a different microbiome composition might respond better to a different strain or combination of strains.
This approach could significantly improve the efficacy and predictability of probiotic treatments, moving away from a “one-size-fits-all” approach.
Combining Probiotics with Other Therapeutic Approaches for IBS Management, Benefits of probiotics for ibs patients
Probiotics are not a standalone solution for all IBS patients. Synergistic effects could be achieved by combining probiotics with other established IBS therapies. Future research should investigate the efficacy and safety of combining probiotics with dietary interventions (such as the low FODMAP diet), prebiotics (which promote the growth of beneficial gut bacteria), psychological therapies (such as cognitive behavioral therapy), and medications (such as antispasmodics or antidepressants).
For instance, a study could compare the effectiveness of a low FODMAP diet alone versus the same diet combined with a specific probiotic strain in alleviating IBS symptoms. Such studies could reveal optimal combinations that enhance therapeutic outcomes and provide a more comprehensive approach to IBS management.
Identifying Optimal Probiotic Strains and Dosages for Specific IBS Subtypes
IBS is not a monolithic condition; it encompasses diverse subtypes with varying symptom profiles and underlying mechanisms. Current research often uses a broad range of probiotic strains and dosages, without considering these subtypes. Future studies should focus on identifying optimal probiotic strains and dosages for specific IBS subtypes (e.g., IBS-D, IBS-C, IBS-M). This targeted approach could lead to more effective and personalized treatments, taking into account the unique characteristics of each IBS subtype.
For example, a strain effective in reducing diarrhea in IBS-D might not be as effective in relieving constipation in IBS-C.
Long-Term Efficacy and Safety of Probiotic Use in IBS
Most clinical trials investigating probiotics for IBS have focused on short-term effects. Long-term studies are necessary to assess the sustained efficacy and safety of probiotic use in managing IBS symptoms over extended periods. This is particularly important to identify potential long-term side effects and to determine the optimal duration of probiotic treatment. Longitudinal studies tracking patient outcomes over several years, along with regular microbiome assessments, could provide valuable insights into the long-term benefits and risks of probiotic therapies.
Final Thoughts: Benefits Of Probiotics For Ibs Patients
Source: ytimg.com
Managing IBS can feel like a constant uphill battle, but understanding the potential benefits of probiotics offers a glimmer of hope. While individual responses vary, the research suggests that incorporating specific probiotic strains into your routine, alongside lifestyle modifications, can significantly improve IBS symptoms. Remember, consulting your healthcare provider is crucial before starting any new supplement regimen. This journey towards better gut health is a personal one, and with the right knowledge and support, you can find strategies that work best for you.
Let’s reclaim our digestive well-being, one beneficial bacteria at a time!
FAQ Overview
What are the most common side effects of probiotics for IBS?
The most common side effects are usually mild and include gas, bloating, and increased bowel movements. However, severe allergic reactions are rare.
How long does it take to see results from taking probiotics for IBS?
This varies greatly depending on the individual, the probiotic strain, and the severity of IBS symptoms. Some people experience relief within a few weeks, while others may need several months to see significant improvements.
Can I take probiotics with other medications?
It’s crucial to talk to your doctor before taking probiotics, especially if you are on other medications. Some probiotics might interact with certain drugs.
Are all probiotics created equal?
No, different strains have different effects. The effectiveness of a probiotic depends on the specific strain, dosage, and formulation. Not all probiotics are suitable for all IBS subtypes.