Clover Exits ACO Reach Medicare Impact
Clover exits ACO reach Medicare – that headline alone sparks a whirlwind of questions, doesn’t it? This post dives into the recent news surrounding Clover Health’s strategic moves within the Medicare Advantage market. We’ll explore the financial implications, analyze their market position, and discuss what this means for both Clover and the future of Medicare Advantage. Get ready for a deep dive into the complexities of healthcare finance and the ever-evolving landscape of Medicare.
We’ll examine Clover Health’s recent financial performance, investor activity, and technological innovations within the context of their decisions regarding Accountable Care Organizations (ACOs) and Medicare. Understanding their strategy requires looking at their market share, competitor analysis, and the impact of regulatory changes. We’ll also consider the patient experience and how Clover’s approach to data analytics plays a crucial role in their overall success (or lack thereof).
Clover Health’s Medicare Advantage (MA) Plans
Clover Health is a relatively new player in the competitive Medicare Advantage market, aiming to disrupt the traditional model with technology-driven solutions. While it hasn’t yet achieved the market dominance of established players, its growth and unique approach warrant examination of its current position and strategies.Clover Health’s market share within the Medicare Advantage space is significantly smaller than industry giants like UnitedHealthcare, Humana, and Aetna.
Precise figures fluctuate, and publicly available data often lags, but reports suggest their market share remains in the low single digits nationally. This smaller market share reflects their later entry into the market and more geographically concentrated operations.
Clover Health’s MA Plan Offerings Compared to Competitors
Clover Health differentiates itself by focusing on technology-driven care coordination and data analytics. Unlike some competitors who primarily offer a broad range of standardized plans, Clover Health emphasizes its use of data and algorithms to personalize care and potentially lower costs. However, major competitors like UnitedHealthcare and Humana offer a much wider variety of plan options, including different levels of coverage, supplemental benefits, and network choices, catering to a broader spectrum of needs and preferences.
Clover Health’s plans may be more limited in their breadth of options at this stage.
Clover Health’s Target Demographic
Clover Health’s target demographic appears to be Medicare beneficiaries who are comfortable with technology and appreciate personalized care approaches. Their focus on data-driven insights suggests they are likely targeting individuals who are more proactive about managing their health and who might benefit from a technology-enabled approach to care coordination. This could include those who are tech-savvy and comfortable using apps and online portals for healthcare management.
However, the exact demographic segmentation remains largely undisclosed publicly.
Geographic Reach of Clover Health’s MA Plans
Clover Health’s Medicare Advantage plans are not available nationwide. Their geographic reach is currently concentrated in specific regions, primarily focusing on select states. This limited geographical presence restricts their overall market penetration compared to national players with extensive network coverage across multiple states. The specific states and counties served by Clover Health’s MA plans can be found on their website and vary from year to year as they expand their operations.
Expansion into new markets is a key component of their growth strategy.
Exits and Investor Activity Surrounding Clover Health
Clover Health, a healthcare technology company focused on Medicare Advantage plans, has experienced a rollercoaster ride in terms of investor activity and market valuation since its inception. Understanding this fluctuating landscape requires examining significant investor moves, mergers and acquisitions, and the resulting financial performance. This analysis will provide a clearer picture of Clover Health’s journey through the complexities of the healthcare investment world.
Significant Investor Activity
Clover Health’s stock price has been highly volatile, reflecting both positive and negative investor sentiment. Early investors, including Chamath Palihapitiya’s Social Capital, initially showed significant confidence in the company’s potential to disrupt the Medicare Advantage market. However, subsequent financial performance and regulatory scrutiny led to significant fluctuations in the stock price and investor confidence. Short sellers have also played a notable role, often betting against the company’s success.
These actions, combined with overall market trends, have created a dynamic and often unpredictable investor environment for Clover Health. A detailed analysis of SEC filings would reveal the precise extent of these activities and their impact on share price.
Mergers, Acquisitions, and Divestitures
To date, Clover Health hasn’t been involved in any major mergers or acquisitions of other significant companies. However, its own history involves acquisitions of smaller companies to bolster its technology platform and expand its service offerings. These acquisitions have been aimed at enhancing Clover Health’s technological capabilities and expanding its reach within the Medicare Advantage market. Information regarding the financial details of these acquisitions is publicly available through SEC filings and press releases.
Further analysis would be required to assess the long-term impact of these strategic moves on the company’s overall financial health.
Financial Performance in Relation to Investor Activity
Clover Health’s financial performance has been closely tied to investor sentiment and market conditions. Periods of positive investor activity have generally coincided with periods of improved financial performance, or at least more optimistic projections. Conversely, periods of negative investor sentiment have often been associated with declining stock prices and increased scrutiny of the company’s financial statements. A thorough examination of Clover Health’s quarterly and annual financial reports, alongside news articles and analyst reports, would provide a more complete picture of this complex relationship.
For instance, a sharp drop in stock price might correlate with a missed earnings target or a negative report from a regulatory agency.
So Clover’s pulling out of ACO Reach Medicare? That’s a big shift in the healthcare landscape. It makes me wonder how other providers are adapting, like the Humana Centerwell primary care centers in Walmart, which are mentioned in this article humana centerwell primary care centers walmart. Their approach to value-based care might offer some insights into what Clover’s exit could mean for the future of ACO Reach and similar programs.
Timeline of Key Events
A detailed timeline of key events would include the company’s IPO, significant funding rounds, any major regulatory actions, and periods of particularly strong or weak financial performance. This timeline would highlight the correlation between investor activity and the company’s operational and financial progress. Such a timeline, constructed from publicly available information, would provide a valuable tool for understanding the evolution of Clover Health’s investor landscape.
For example, a specific date could mark a significant investment from a major player, or a regulatory decision that impacted investor confidence.
Clover Health’s Technology and Data Analytics in MA
Clover Health distinguishes itself in the Medicare Advantage market through its significant investment in technology and data analytics. This technological focus aims to improve patient care, streamline administrative processes, and ultimately, reduce healthcare costs. Their approach leverages a combination of data-driven insights and technological tools to personalize care and optimize resource allocation.Clover Health employs a sophisticated technology platform to manage and analyze the vast amounts of patient data inherent in Medicare Advantage plans.
This platform integrates data from various sources, including electronic health records (EHRs), claims data, pharmacy records, and wearable device data (where applicable and with patient consent). Machine learning algorithms are then applied to identify patterns and insights that can inform care decisions and predict potential health risks. This allows for proactive interventions, personalized care plans, and more efficient resource allocation.
Clover Health’s Technological Approach Compared to Competitors
While many MA providers utilize data analytics to some degree, Clover Health’s approach is characterized by a more aggressive and comprehensive integration of technology across its operations. Unlike some competitors who may rely on more traditional methods or less integrated systems, Clover Health emphasizes a proactive, data-driven approach to care management. This difference manifests in their ability to identify at-risk patients earlier, personalize care plans more effectively, and ultimately, achieve better patient outcomes.
For example, some competitors might use data analytics primarily for fraud detection or claims processing, while Clover Health uses it for proactive care management and predictive analytics to prevent hospital readmissions.
Data Analytics for Improved Patient Care and Outcomes
Clover Health uses data analytics to personalize care plans, predict potential health risks, and proactively intervene to prevent adverse events. By identifying patients at high risk of hospitalization or other negative health outcomes, the company can tailor interventions such as increased telehealth monitoring, home visits, or medication management to mitigate those risks. Their algorithms analyze patient data to identify trends and patterns, enabling proactive engagement and more effective disease management.
This proactive approach leads to improved patient outcomes and potentially lower overall healthcare costs.
Impact of Clover Health’s Technology on Patient Experience and Cost-Effectiveness
Clover Health’s technology has demonstrably impacted both patient experience and cost-effectiveness. The personalized care plans, driven by data analytics, contribute to improved patient satisfaction by providing more targeted and relevant support. Proactive interventions help prevent costly hospital readmissions and emergency room visits, leading to greater cost-effectiveness for the plan. For example, early identification of patients at risk of developing chronic conditions allows for timely interventions, potentially preventing the progression of the disease and reducing long-term healthcare costs.
Technology Comparison: Clover Health vs. Competitor X
| Feature | Clover Health | Competitor X (Example: Humana) | Comparison |
|---|---|---|---|
| Data Integration | Comprehensive integration of EHRs, claims data, pharmacy records, and potentially wearable device data. | Integration of claims data and some EHR data, potentially less comprehensive integration of other sources. | Clover Health demonstrates a broader and deeper data integration strategy. |
| Predictive Analytics | Utilizes machine learning to predict risk of hospitalization, readmissions, and other adverse events. | Employs predictive modeling, but may focus less on proactive interventions based on these predictions. | Both use predictive analytics, but Clover Health’s emphasis on proactive intervention distinguishes its approach. |
| Personalized Care Plans | Highly personalized care plans tailored to individual patient needs and risk profiles. | Offers personalized care, but the level of personalization may be less granular. | Clover Health’s approach to personalized care is more data-driven and tailored. |
| Telehealth Integration | Seamless integration of telehealth services into care plans. | Offers telehealth services, but the level of integration may vary. | Clover Health prioritizes telehealth integration for proactive and convenient care. |
Medicare Advantage Program’s Impact on Clover Health’s Strategy: Clover Exits Aco Reach Medicare
Clover Health, a company heavily invested in Medicare Advantage (MA) plans, is significantly impacted by the ever-evolving landscape of MA regulations. Understanding these regulations and adapting to them is crucial for the company’s continued success and profitability. The complexities of the MA program present both opportunities and challenges for Clover Health’s unique technology-driven approach to healthcare.The Medicare Advantage program’s reimbursement models and regulatory frameworks directly influence Clover Health’s business model.
Clover’s strategy relies on leveraging data analytics and technology to improve patient outcomes and reduce costs, thereby increasing efficiency and potentially earning higher reimbursement rates. Changes in how the Centers for Medicare & Medicaid Services (CMS) calculates payments or adjusts risk adjustment models directly impact Clover’s revenue projections and operational strategies. For example, shifts in the weighting of various chronic conditions within the risk adjustment model could alter Clover’s profitability depending on the specific patient demographics it serves.
Consequently, Clover must continually adapt its algorithms and care management programs to reflect these shifts and maintain its competitive edge.
Clover Health’s Adaptive Strategies
Clover Health employs several strategies to remain compliant with MA program requirements and navigate the complexities of the regulatory environment. This includes investing heavily in compliance personnel and systems to ensure accurate reporting and adherence to all relevant regulations. They also actively participate in industry associations and engage with CMS to understand upcoming changes and provide input on policy development.
Furthermore, Clover’s technology platform is designed to be flexible and adaptable, allowing for quick updates and adjustments to accommodate new regulations and evolving reimbursement models. This agility is critical in a rapidly changing environment. A key component of this adaptation involves ongoing refinement of their predictive models and risk assessment tools to accurately reflect changes in CMS guidelines and to optimize their resource allocation for patient care.
Clover’s exit from ACO Reach in Medicare is a significant development, highlighting the challenges of managing healthcare costs effectively. Understanding the complexities involved requires looking at the bigger picture, like the issues discussed in this insightful article on health cost inflation variation price transparency turquoise , which explores price transparency and its impact on overall healthcare spending. Ultimately, Clover’s decision underscores the need for innovative solutions to curb rising healthcare costs within the Medicare system.
Challenges in Navigating the Medicare Advantage Landscape
The Medicare Advantage landscape presents significant challenges for Clover Health. Competition is fierce, with established players and new entrants vying for market share. Maintaining profitability in the face of fluctuating reimbursement rates and increasing regulatory scrutiny requires constant innovation and efficiency improvements. Another key challenge is the inherent complexity of the MA program itself. Understanding and complying with the multitude of regulations and requirements across various states can be demanding and resource-intensive.
Finally, maintaining patient trust and ensuring high-quality care while simultaneously managing costs and optimizing for reimbursement presents a constant balancing act.
Potential Future Regulatory Changes and Their Impact
The Medicare Advantage program is subject to periodic changes and revisions. Several potential future regulatory changes could significantly impact Clover Health’s operations:
- Increased scrutiny of risk adjustment models: More stringent audits and adjustments to risk adjustment methodologies could reduce Clover’s reimbursement rates, impacting profitability.
- Changes in star ratings system: Alterations to the star rating system, which reflects the quality of care provided by MA plans, could affect enrollment and potentially impact Clover’s market share. A decline in star ratings could lead to reduced enrollment and, consequently, lower revenue.
- Expansion of telehealth regulations: While potentially beneficial, changes to telehealth reimbursement rates and regulations could necessitate adjustments to Clover’s operational model and technology infrastructure, requiring further investment.
- Increased focus on social determinants of health: Future regulations might emphasize addressing social determinants of health, requiring Clover to integrate these factors more comprehensively into its care management strategies and potentially increasing operational costs.
Clover Health’s Member Experience and Satisfaction
Clover Health’s success hinges not only on its technological advancements in Medicare Advantage but also on its ability to provide a positive and satisfying experience for its members. A strong member experience fosters loyalty, improves health outcomes, and ultimately contributes to the company’s overall performance. This section delves into Clover Health’s approach to member engagement, satisfaction metrics, and strategies for improvement.Clover Health’s approach to member engagement and communication centers around personalized interactions and readily accessible support.
They utilize a multi-channel strategy, incorporating telehealth options, dedicated care teams, and a user-friendly mobile app for easy access to information and services. This proactive communication aims to keep members informed about their coverage, benefits, and health management tools. The company also emphasizes clear and concise communication, avoiding jargon and ensuring information is easily understood by all members, regardless of their technological literacy.
Clover Health Member Engagement Strategies
Clover Health employs several strategies to foster member engagement. These include personalized wellness programs tailored to individual member needs, proactive outreach regarding preventative care, and convenient access to telehealth services. Regular communication, such as newsletters and personalized reminders, keeps members informed about their plan benefits and upcoming appointments. The company also actively solicits member feedback through surveys and other channels to continuously improve its services.
A strong focus on personalized care and proactive communication is central to their strategy.
Hypothetical Case Study: A Positive Member Experience
Imagine Mrs. Eleanor Vance, a 72-year-old with type 2 diabetes. After enrolling in Clover Health’s Medicare Advantage plan, she was assigned a dedicated care coordinator who proactively contacted her to schedule a telehealth appointment with her physician. The appointment was seamless and convenient, allowing Mrs. Vance to discuss her diabetes management from the comfort of her home.
Her care coordinator also helped her navigate the complexities of her prescription coverage and arranged for home delivery of her medications. Throughout her experience, Mrs. Vance felt supported, informed, and empowered to manage her health effectively. This positive interaction fostered a strong sense of trust and satisfaction with Clover Health.
Comparison of Member Satisfaction Levels with Industry Benchmarks
While specific, publicly available data on Clover Health’s member satisfaction compared to industry benchmarks is limited, it’s crucial to note that Medicare Advantage plans are regularly evaluated by the Centers for Medicare & Medicaid Services (CMS) through the CMS Star Ratings system. This system uses a variety of metrics to assess plan performance, including member satisfaction. Clover Health’s performance in this system provides an indication of their member satisfaction levels relative to other plans.
Higher star ratings suggest greater member satisfaction. Direct comparison to competitors requires access to proprietary data from each company, which is not always publicly available.
Clover Health’s Member Satisfaction Measurement and Improvement Processes, Clover exits aco reach medicare
Clover Health utilizes a multi-faceted approach to measure and improve member satisfaction. They regularly conduct member satisfaction surveys, analyzing responses to identify areas for improvement. They also track key performance indicators (KPIs) such as member retention rates, call center resolution times, and Net Promoter Score (NPS) to gauge member sentiment and identify trends. This data informs continuous improvements in their communication strategies, care coordination processes, and overall member experience.
By actively seeking and responding to member feedback, Clover Health strives to consistently enhance its services and maintain high levels of satisfaction.
Financial Implications of “Clover Exits ACO Reach Medicare”

Source: cloverhealth.com
Clover Health’s decisions regarding its participation in ACO REACH (Accountable Care Organizations Realizing Equity, Access, and Community Health) and its broader Medicare Advantage (MA) strategy have significant financial ramifications. Understanding these implications requires examining Clover’s revenue streams, its dependence on MA, and the potential long-term effects of its strategic choices. The “exits” from ACO REACH, if any, represent a shift in their approach to risk and reward within the Medicare Advantage market.Clover Health’s revenue is heavily reliant on Medicare Advantage premiums.
A significant portion of their income comes from the per-member-per-month (PMPM) payments they receive from Medicare for managing the care of their MA enrollees. Other revenue streams, such as those generated through ancillary services or technological solutions, are comparatively smaller. Therefore, any reduction in MA membership or changes in reimbursement rates directly impact their bottom line.
Clover Health’s Revenue Streams and Dependence on Medicare Advantage
Clover Health’s financial performance is intrinsically linked to its success in the Medicare Advantage market. Their primary revenue source is the PMPM payments received from the Centers for Medicare & Medicaid Services (CMS). The number of enrolled members and the average PMPM rate are crucial factors determining their overall revenue. Any decrease in membership, due to exits from ACO REACH or other strategic decisions, will directly reduce revenue.
Furthermore, changes in CMS reimbursement policies can also significantly impact their profitability. A hypothetical example: if Clover Health loses 10,000 members with an average PMPM of $1000, this represents a $10 million annual revenue reduction. This highlights the company’s vulnerability to fluctuations in membership and regulatory changes.
Long-Term Financial Implications of Clover Health’s Medicare Advantage Strategies
Clover Health’s long-term financial outlook hinges on its ability to effectively manage its MA plans and navigate the evolving landscape of healthcare policy. Their strategies concerning ACO REACH participation, technological investments, and member acquisition directly impact their profitability and sustainability. Continued success in attracting and retaining members, coupled with efficient cost management and technological innovation, will be crucial for long-term financial stability.
Clover’s exit from ACO Reach Medicare is a significant development, highlighting the challenges of coordinating care for seniors. This underscores the urgent need for innovative solutions, like those explored in this insightful article on reimagining collaboration in senior care a technology driven approach , which suggests that tech-driven approaches could streamline processes and improve patient outcomes. Ultimately, the Clover situation reinforces the importance of finding better ways to manage senior care within the Medicare system.
Conversely, failure to adapt to changing market conditions or regulatory shifts could lead to significant financial challenges. For example, a failure to adopt innovative care models or improve member satisfaction could result in membership loss and reduced PMPM rates, impacting future growth and profitability.
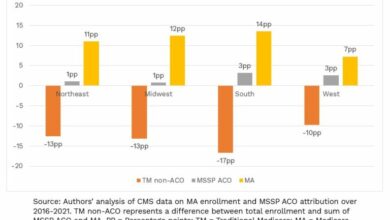
Visual Representation of Exits and Financial Performance
Imagine a line graph. The X-axis represents time (e.g., quarters or years), and the Y-axis represents Clover Health’s financial performance, measured by metrics like net income or revenue. Each data point on the graph represents Clover Health’s financial performance during a specific period. Now, let’s represent “exits” from ACO REACH or other MA initiatives. These “exits” can be visually represented as downward spikes or dips in the line graph, occurring at the specific time points when these exits were reported.
The magnitude of the dip would correspond to the financial impact of the exit. The graph would visually illustrate the correlation (or lack thereof) between these exits and Clover Health’s financial performance. A sustained downward trend after multiple exits would suggest a negative correlation, while a recovery or resilience in the line despite exits might suggest a less significant impact or successful mitigation strategies.
This visual would effectively showcase the relationship between Clover Health’s strategic decisions and their financial outcomes over time.
Outcome Summary

Source: amac.us
Clover Health’s departure from certain ACO arrangements within the Medicare Advantage program represents a significant shift in their strategy. The long-term implications remain to be seen, but this decision underscores the ongoing challenges and opportunities within the complex world of Medicare Advantage. It highlights the need for adaptability and innovation in a market constantly evolving due to regulatory changes and competitive pressures.
Keep an eye on Clover Health – this is definitely a story to follow.
Q&A
What is an ACO (Accountable Care Organization)?
An ACO is a group of healthcare providers who work together to coordinate care for Medicare patients. The goal is to improve the quality of care while reducing costs.
Why did Clover exit some ACO arrangements?
The reasons are likely multifaceted and may include financial considerations, strategic realignment, or a shift in focus towards different market segments. More specific information would require access to Clover’s internal documents and announcements.
What are the potential consequences for patients affected by these changes?
The impact on patients will vary depending on their specific circumstances and the nature of Clover’s exit strategy. It’s crucial for affected patients to reach out to Clover Health or their healthcare provider to understand how the changes will affect their care.
How does this affect Clover Health’s long-term prospects?
The long-term impact is uncertain. Success will depend on how effectively Clover adapts its strategy and navigates the changing Medicare Advantage landscape. Time will tell if this decision ultimately benefits or harms the company’s growth.