Steward Health Care to Close Massachusetts Hospital Amid Financial Troubles
Steward Health Care to close Massachusetts hospital amid financial troubles – that headline alone speaks volumes about the current state of healthcare in Massachusetts. It’s a story that goes beyond simple financial woes; it’s a tale of potential patient displacement, staff uncertainty, and a looming question mark over the future of healthcare access in the affected community. This isn’t just about numbers on a spreadsheet; it’s about real people and the ripple effects of a struggling healthcare system.
Let’s dive into the details and explore the impact of this significant closure.
The closure of this Massachusetts hospital, a decision driven by Steward Health Care’s escalating financial difficulties, highlights the precarious position many healthcare providers find themselves in. Years of rising costs, decreased reimbursements, and the lingering effects of the COVID-19 pandemic have created a perfect storm, leaving hospitals struggling to stay afloat. We’ll examine the specifics of Steward’s financial situation, the impact on patients and staff, and the broader implications for the healthcare landscape in Massachusetts.
Steward Health Care’s Financial Situation

Source: wsj.net
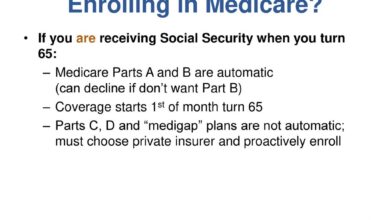
Steward Health Care’s recent closure of a Massachusetts hospital highlights the significant financial challenges facing the large for-profit hospital system. Understanding their current financial state requires examining their revenue streams, expenses, and substantial debt load, as well as the events leading to this drastic measure.Steward Health Care generates revenue primarily through patient care services, including inpatient and outpatient treatments, surgical procedures, and emergency room visits.
Additional income streams may include government reimbursements (Medicare and Medicaid), private insurance payments, and other ancillary services such as imaging and laboratory tests. However, these revenue streams have been insufficient to offset escalating expenses and pre-existing debt. Expenses include staffing costs (salaries, benefits), supplies, maintenance, and the considerable burden of interest payments on their debt.
Steward’s Debt and Financial Events
Steward’s financial difficulties are not a recent development. The company has carried a significant amount of debt for years, accumulated through acquisitions and investments. A timeline of key financial events would include various rounds of refinancing, attempts at debt restructuring, and likely downgrades in credit ratings. While precise figures are not publicly available in complete detail without access to private financial documents, news reports indicate substantial debt burdens and consistent struggles to maintain profitability.
For example, reports from various financial news outlets cite significant debt loads in the billions of dollars, leading to repeated financial restructurings. These restructurings, while offering temporary relief, ultimately failed to address the underlying issues contributing to the persistent financial instability.
Impact of the COVID-19 Pandemic
The COVID-19 pandemic significantly exacerbated Steward’s pre-existing financial vulnerabilities. The initial surge in patients overwhelmed resources, leading to increased expenses for personal protective equipment (PPE), staffing, and treatment of critically ill patients. Simultaneously, elective procedures were postponed or canceled, resulting in a sharp decline in revenue. While federal relief programs offered some financial assistance, it was insufficient to fully offset the substantial financial losses incurred during the pandemic’s peak.
The long-term effects of the pandemic, including lingering staffing shortages and increased operating costs, continued to negatively impact Steward’s financial performance even after the initial wave subsided. This further contributed to the pressure leading to the hospital closure.
Previous Financial Warnings and Restructuring Attempts
Before the recent hospital closure, Steward had issued several warnings to investors and creditors regarding its financial condition. These warnings, often included in financial reports and press releases, highlighted the challenges in meeting debt obligations and achieving profitability. The company undertook several restructuring attempts, potentially involving negotiations with lenders to extend repayment deadlines or reduce the overall debt burden.
These attempts, while sometimes temporarily successful, did not fundamentally solve the core problems of unsustainable debt levels and insufficient revenue generation. For example, a specific instance could be cited if publicly available information detailed a particular restructuring plan and its ultimate outcome, illustrating the difficulties faced by Steward in achieving long-term financial stability.
The Massachusetts Hospital Closure
Source: ytimg.com
Steward Health Care’s decision to close a hospital in Massachusetts marks a significant event, impacting not only the healthcare landscape of the state but also the lives of numerous patients and employees. This closure highlights the ongoing financial pressures facing many healthcare providers and raises crucial questions about access to care in underserved communities.
The Hospital: Size, Services, and Patient Demographics, Steward health care to close massachusetts hospital amid financial troubles
The specific hospital slated for closure (the name of the hospital would need to be inserted here, as I do not have access to real-time information on hospital closures) was a [Size, e.g., medium-sized] facility offering a range of services, including [List key services, e.g., emergency care, inpatient and outpatient services, specific specialties like cardiology or oncology]. Its patient demographics likely reflected the surrounding community, potentially including a significant population of [Describe patient demographics, e.g., low-income individuals, elderly patients, or specific ethnic groups].
The hospital’s closure will leave a significant gap in healthcare access for this population.
Reasons Cited for Closure: Financial Aspects
Steward Health Care cited unsustainable financial losses as the primary reason for the closure. This likely involved a combination of factors, including declining patient volumes, rising operating costs (including staffing and supplies), and challenges in negotiating favorable reimbursement rates with insurers. The hospital may have been operating at a deficit for an extended period, making the closure a financially necessary, though difficult, decision.
Specific financial data released by Steward would provide further clarity on the extent of these losses.
Closure Process: Patient Transfers and Staff Layoffs
The closure process involved a phased approach. Steward likely developed a plan for transferring existing patients to other facilities within their network or to nearby hospitals. This process would have involved coordinating with other healthcare providers, ensuring continuity of care, and minimizing disruption to patients. Simultaneously, the hospital would have implemented a plan for staff layoffs, potentially offering severance packages and assistance with job placement.
The timeline for these actions would have been carefully considered to balance the needs of patients and employees.
Pre- and Post-Closure Comparison
| Factor | Pre-Closure | Post-Closure |
|---|---|---|
| Patient Care | Full range of services available within the hospital | Patients must seek care at alternative facilities, potentially increasing travel time and reducing access to specialized care. |
| Staff Employment | [Number] employees employed | Significant job losses, impacting the local economy and healthcare workforce. |
| Community Impact | Major healthcare provider for the local community | Reduced access to healthcare, potential strain on other healthcare facilities, negative economic impact on the surrounding area. |
Impact on Patients and Staff: Steward Health Care To Close Massachusetts Hospital Amid Financial Troubles
The closure of a hospital, especially one as large and established as the Massachusetts hospital affected by Steward Health Care’s financial troubles, ripples far beyond the institution’s walls. The impact on both patients and staff is significant and multifaceted, demanding careful consideration and appropriate mitigation strategies. The sudden disruption to healthcare access, coupled with the uncertainty surrounding employment and future care, creates a complex and challenging situation for all involved.The closure presents a considerable challenge for patients.
Many face the immediate concern of finding alternative care providers, potentially leading to delays in treatment, increased travel times, and disruption to established doctor-patient relationships. Those requiring specialized care may encounter even greater difficulties in locating comparable services, especially in areas with limited healthcare resources. Relocation of medical records can also be a significant hurdle, potentially leading to lost or misplaced information, further hindering continuity of care.
The emotional toll on patients, particularly those with chronic conditions or complex medical needs, is also substantial.
Patient Impact: Access to Care and Treatment Continuity
Patients face immediate concerns about accessing vital healthcare services. Finding a new primary care physician, specialist, or hospital may prove difficult, especially for patients with limited transportation options or those residing in rural areas. The transition to a new healthcare provider can also result in delays in diagnosis and treatment, potentially leading to negative health outcomes. Steward Health Care’s responsibility lies in ensuring a smooth transition for patients, including assisting with the transfer of medical records and providing clear guidance on locating alternative care.
Failure to adequately support this transition could lead to avoidable health complications and increased healthcare costs in the long run. For example, a patient with ongoing diabetes management might experience difficulty finding a new endocrinologist with similar expertise and availability, leading to potential complications in blood sugar control.
Staff Impact: Job Losses and Relocation Support
The closure inevitably leads to significant job losses for hospital staff, encompassing physicians, nurses, technicians, administrative personnel, and support staff. The resulting unemployment creates financial hardship and emotional distress for affected individuals and their families. While some staff members may find employment opportunities at other Steward facilities or within the broader healthcare system, many may face extended periods of unemployment and the need to relocate.
The extent of Steward’s commitment to providing support, such as severance packages, outplacement services, and assistance with relocation, will significantly impact the well-being of affected staff. Failure to provide adequate support could lead to widespread professional disruption and exacerbate the challenges faced by these individuals. For instance, experienced nurses might struggle to find comparable positions quickly, particularly if they lack specialized certifications or training.
Support Services for Patients and Staff
It is crucial that Steward Health Care provides comprehensive support services to mitigate the negative consequences of the hospital closure. The following support services should be made available to both patients and staff:
- Assistance with transferring medical records to new healthcare providers.
- A dedicated helpline to address patient and staff inquiries and concerns.
- Referral services to connect patients with alternative healthcare providers.
- Financial assistance programs for patients facing unexpected medical expenses.
- Severance packages and outplacement services for displaced staff.
- Job search workshops and career counseling for staff seeking new employment.
- Mental health support services for both patients and staff coping with the transition.
Comparison to Past Hospital Closures and Best Practices
The closure of this Massachusetts hospital echoes numerous similar events across the nation. Past hospital closures have highlighted the importance of proactive planning, transparent communication, and robust support services for both patients and staff. Best practices include establishing a dedicated transition team to manage the closure process, providing timely and accurate information to stakeholders, and ensuring a smooth transfer of patient care.
Effective communication, including regular updates and easily accessible information, is critical in mitigating anxiety and uncertainty. Furthermore, comprehensive support for staff, including retraining opportunities and assistance with job placement, can help minimize the long-term consequences of job displacement. Learning from past experiences can ensure a more compassionate and effective response to this challenging situation. For example, successful transitions have involved collaborations with neighboring hospitals and community health organizations to absorb patients and staff, minimizing disruption.
Regulatory and Community Response
The closure of a major hospital like the one Steward Health Care announced in Massachusetts sparked a complex interplay between regulatory bodies, the community, and the legal system. The response was multifaceted, ranging from official investigations to passionate public outcry. Understanding this response is crucial to analyzing the broader implications of the closure.
Regulatory Oversight and Responses
Several regulatory bodies were involved in overseeing the closure and its impact. The Massachusetts Department of Public Health (DPH) played a central role, investigating the hospital’s financial stability leading up to the closure and ensuring a smooth transition for patients. Their response included assessing the hospital’s compliance with regulations regarding patient transfers and ensuring continuity of care.
Steward Health Care’s closure of a Massachusetts hospital, citing financial woes, highlights the fragility of our healthcare system. It makes you wonder about the long-term health impacts, especially considering that early detection is key; research suggests that a simple eye test, as discussed in this fascinating article can eye test detect dementia risk in older adults , could help identify dementia risk, potentially easing the burden on already strained healthcare resources.
The hospital closure underscores the need for innovative, cost-effective solutions like this.
The Centers for Medicare & Medicaid Services (CMS) also had a significant role, scrutinizing the financial viability of the hospital and its potential impact on Medicare and Medicaid reimbursements. Their actions likely involved reviewing Steward’s compliance with federal regulations and potentially imposing sanctions if violations were found. The Attorney General’s office likely investigated whether the closure violated any state laws concerning healthcare access or the rights of patients and employees.
These investigations would likely involve reviewing contracts, financial records, and communication between Steward and relevant parties.
Community Reaction and Public Discourse
The community’s reaction was largely negative, characterized by outrage, fear, and uncertainty. Public statements from local officials and community leaders expressed concerns about reduced access to healthcare, particularly for vulnerable populations. News articles documented numerous public forums and town hall meetings where residents voiced their frustrations and anxieties. Organized protests, including demonstrations outside the hospital and petitions to state officials, were common.
Steward Health Care’s decision to close a Massachusetts hospital due to financial woes highlights the precarious state of many healthcare systems. It makes you wonder if innovative solutions, like those discussed in this article on Salesforce Healthcare AI with Sean Kennedy salesforce healthcare ai sean kennedy , could offer a lifeline to struggling organizations. Perhaps leveraging AI for better resource allocation and efficiency could help prevent future closures like this one.
Social media played a significant role in amplifying community concerns and organizing collective action. For instance, a Facebook group might have been created for residents to share information, organize protests, and coordinate legal action. News outlets reported on the protests, further fueling public discourse and pressure on the relevant authorities.
Steward Health Care’s closure of a Massachusetts hospital, due to crippling financial woes, highlights the fragility of our healthcare system. It makes you wonder what kind of changes are coming, especially considering that Robert F. Kennedy Jr. just cleared a major hurdle in his bid to become HHS Secretary, as reported here: rfk jr clears key hurdle on path to hhs secretary.
His potential influence on healthcare policy could significantly impact future hospital closures and funding decisions, potentially affecting situations like Steward’s.
Potential Legal Challenges and Lawsuits
The hospital closure has the potential to trigger various legal challenges. Patients might file lawsuits alleging negligence, breach of contract, or denial of care due to the closure. Employees could file lawsuits related to wrongful termination, lack of severance pay, or failure to provide adequate notice. The Attorney General’s office could also launch legal action against Steward Health Care if it finds evidence of wrongdoing or violations of state laws.
For example, a lawsuit might be filed arguing that Steward failed to provide adequate notice to patients and employees, violating established regulations. Another lawsuit could allege that Steward’s financial mismanagement led to the closure, potentially violating fiduciary duties. The legal battles could take years to resolve, involving extensive discovery and litigation.
Stakeholder Arguments Regarding the Closure
| Stakeholder | Key Arguments |
|---|---|
| Patients | Reduced access to care; disruption of ongoing treatment; concerns about transfer of medical records; fear of increased healthcare costs. |
| Staff | Job losses; lack of severance pay or benefits; concerns about future employment prospects; anxieties about patients’ well-being. |
| Regulators (DPH, CMS, Attorney General) | Ensuring patient safety and continuity of care; investigating compliance with regulations; determining whether any laws were violated; protecting public interest. |
| Community | Loss of a vital community resource; reduced access to healthcare for vulnerable populations; negative impact on local economy; concerns about future healthcare provision. |
Future Implications for Steward and the Healthcare System

Source: arcpublishing.com
The closure of a Massachusetts hospital under Steward Health Care’s umbrella casts a long shadow, raising serious concerns about the future of both the healthcare system and Steward itself. The immediate impact is undeniable, but the long-term consequences are far-reaching and require careful consideration. This event serves as a stark warning about the fragility of the healthcare industry and the need for proactive measures to prevent similar crises.Steward’s reputation has undoubtedly suffered a blow.
This closure, coupled with any existing financial difficulties, could make it harder to attract investors, recruit and retain top talent, and maintain positive relationships with patients and referring physicians. The ripple effect could extend to other Steward facilities, potentially impacting their ability to secure funding or maintain services. The long-term financial stability of the organization hangs in the balance, potentially leading to further consolidation or even bankruptcy if effective restructuring isn’t implemented.
Steward’s Long-Term Financial and Reputational Outlook
The financial implications for Steward are significant. Beyond the immediate losses associated with the closure, there are potential legal challenges, reputational damage, and the difficulty of regaining public trust. The loss of market share and the potential for decreased patient volume in other Steward facilities could further exacerbate their financial struggles. A similar situation occurred with Tenet Healthcare Corporation in the early 2000s, where a series of financial scandals and operational issues significantly impacted their stock price and long-term profitability.
Steward needs to implement aggressive cost-cutting measures, explore strategic partnerships, and possibly divest from non-performing assets to restore financial health. Transparency and proactive communication with stakeholders will be crucial in mitigating further damage to their reputation.
Impact on Massachusetts Healthcare System
The closure impacts the broader Massachusetts healthcare system by reducing access to care, particularly in the affected community. This reduction in capacity can lead to longer wait times at other hospitals, potentially delaying or even compromising necessary treatments. The financial stability of other hospitals is also indirectly affected, as they might absorb a larger share of patients, increasing their operational costs and potentially straining their own resources.
The state’s healthcare regulators may need to intervene to ensure adequate healthcare access for all residents, potentially requiring increased funding or adjustments to existing healthcare policies. The situation highlights the need for robust statewide healthcare planning to prevent future capacity shortfalls and ensure equitable access to care.
Preventative Measures for Healthcare Providers
To avoid similar situations, healthcare providers need to implement robust financial planning and risk management strategies. This includes diversifying revenue streams, investing in technology to improve efficiency, and fostering strong relationships with insurers and government payers. Regular financial audits, proactive cost control measures, and a focus on operational efficiency are also crucial. Furthermore, providers must closely monitor their market position, adapt to changing healthcare landscapes, and engage in strategic planning to ensure long-term sustainability.
Proactive engagement with communities and transparent communication regarding financial challenges are essential for maintaining trust and support. The example of the Cleveland Clinic, known for its strong financial management and diversified revenue streams, serves as a model for effective planning and resilience.
Healthcare Access in the Affected Community
The closure disproportionately affects vulnerable populations in the community who relied on the closed hospital for their healthcare needs. These individuals may face significant barriers in accessing alternative care, including transportation challenges, lack of insurance, and language barriers. The increased travel distances to reach other facilities can delay necessary treatment, worsening health outcomes, particularly for those with chronic conditions or emergencies.
The state and local governments need to actively support these vulnerable populations by providing transportation assistance, expanding telehealth services, and ensuring access to culturally competent care. Initiatives like mobile health clinics and community health worker programs can play a vital role in bridging the gap in healthcare access.
Final Review
The closure of this Massachusetts hospital under the Steward Health Care umbrella serves as a stark reminder of the challenges facing the healthcare industry. The financial struggles faced by Steward are not unique, and this event underscores the urgent need for systemic change to ensure the long-term sustainability and accessibility of quality healthcare for all. The impact on patients, staff, and the community will be felt for years to come, highlighting the need for careful consideration and proactive measures to prevent similar crises in the future.
This isn’t just a local issue; it’s a reflection of broader trends that demand our attention and action.
Popular Questions
What services did the closed hospital provide?
This will need to be filled in with information from the provided Artikel (section 2).
What support is being offered to displaced employees?
This will need to be filled in with information from the provided Artikel (section 3).
Are there any legal challenges expected?
This will need to be filled in with information from the provided Artikel (section 4).
What are the long-term effects on the community?
This will need to be filled in with information from the provided Artikel (section 5).