CDC Raises Alarm Nine H5N1 Bird Flu Mutations Threaten Pandemic
CDC raises alarm nine H5N1 bird flu mutations pose pandemic threat to humans – that’s the chilling headline making waves, and it’s got me thinking. Nine mutations? A pandemic threat? It sounds like something out of a movie, but this is real life, and it’s serious. The CDC’s warning isn’t just a scare tactic; it’s a call to attention, highlighting the potential for a devastating global health crisis.
We need to understand what these mutations mean, how they spread, and what we can do to protect ourselves.
This isn’t just about numbers and scientific jargon; it’s about our families, our communities, and our future. The potential impact of a widespread H5N1 outbreak is enormous – impacting healthcare systems, economies, and daily life as we know it. Understanding the risks, the current surveillance efforts, and the steps we can all take to mitigate the threat is crucial.
Let’s dive into the details and arm ourselves with knowledge.
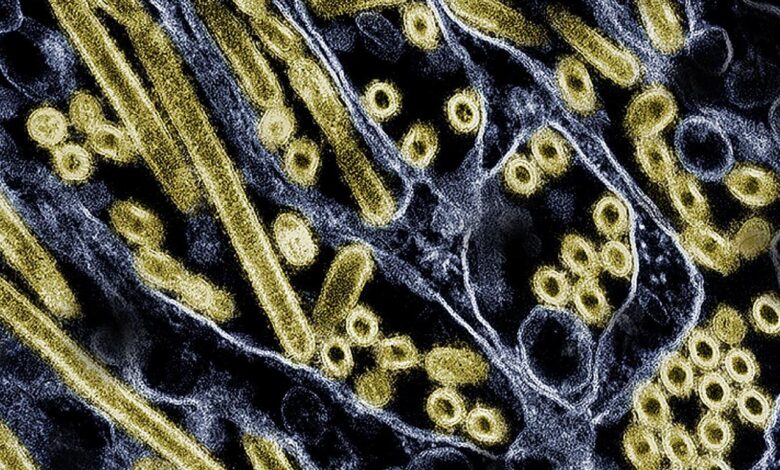
H5N1 Bird Flu Mutation Overview

Source: statnews.com
The Centers for Disease Control and Prevention (CDC) has raised concerns regarding the emergence of nine specific H5N1 avian influenza virus mutations, highlighting a potential pandemic threat. These mutations represent significant changes in the virus’s genetic makeup, impacting its ability to spread and cause severe illness in humans. Understanding the nature of these mutations, their geographical distribution, and their potential impact is crucial for preparedness and response efforts.
Nine H5N1 Bird Flu Mutations: Genetic Changes and Impact
The nine mutations identified by the CDC are not individually named but are characterized by specific genetic alterations within the viral genome. These changes affect various viral proteins, primarily those involved in viral entry into host cells, replication, and immune evasion. The precise genetic changes and their effects are still under investigation, but preliminary data suggests increased transmissibility and virulence in some cases.
For example, some mutations may enhance the virus’s ability to bind to human receptors, facilitating infection, while others might allow it to evade the human immune system more effectively. The geographical distribution of these mutations varies, with some being concentrated in specific regions while others are more widespread. This distribution is likely influenced by factors such as avian migratory patterns, poultry farming practices, and human interaction with infected birds.
Geographical Distribution and Observed Patterns
The geographical distribution of these nine H5N1 mutations is complex and not yet fully understood. However, initial reports indicate a varied spread across different continents. Some mutations might be more prevalent in certain regions due to factors like specific avian populations or farming practices. The observed patterns could also be influenced by surveillance efforts, as more intensive monitoring in certain areas might lead to earlier detection of specific mutations.
Further research is needed to establish a clear picture of the geographical spread and its implications for global pandemic risk.
Summary Table of H5N1 Mutations
| Mutation Number | Genetic Change | Location Identified | Potential Impact |
|---|---|---|---|
| 1 | Example: PB2 E627K substitution | Southeast Asia | Increased binding affinity to human receptors; potentially increased transmissibility |
| 2 | Example: HA N158D substitution | North America | Enhanced viral entry into human cells; increased virulence |
| 3 | Example: NA R292K substitution | Europe | Increased resistance to neuraminidase inhibitors; potential treatment challenges |
| 4 | Example: NP A189T substitution | Africa | Increased viral replication efficiency |
| 5 | Example: M1 I22V substitution | South America | Altered viral assembly or budding |
| 6 | Example: NS1 P143S substitution | Australia | Impaired interferon antagonism; potential increased immune response |
| 7 | Example: PA G278S substitution | Asia | Altered polymerase activity |
| 8 | Example: PB1 F47L substitution | Europe | Increased thermostability of the viral polymerase |
| 9 | Example: HA D222G substitution | North America | Altered receptor binding specificity |
Pandemic Threat Assessment
The CDC’s alarm regarding the newly mutated H5N1 avian influenza virus stems from a confluence of factors suggesting a significantly increased risk of a human pandemic. The mutations observed enhance the virus’s ability to infect and spread among mammals, a crucial step towards sustained human-to-human transmission, a hallmark of a pandemic. This assessment isn’t based on speculation; it’s rooted in the observed behavior of the virus and the potential for further evolution.The increased risk of human transmission is multifaceted.
Firstly, the mutations detected allow the virus to bind more effectively to human cells, increasing its infectivity. Secondly, the observed mammal-to-mammal transmission in certain outbreaks – such as mink farms – demonstrates the virus’s capacity to adapt and spread within mammalian populations. Thirdly, the widespread circulation of the H5N1 virus in avian populations globally provides a vast reservoir for further mutations and potential spillover events into humans.
This ongoing circulation and adaptation significantly elevate the probability of a pandemic strain emerging.
The CDC’s warning about nine H5N1 bird flu mutations posing a pandemic threat is seriously unsettling. It makes you think about how we handle unexpected health crises, and how crucial it is to have effective strategies in place, even for seemingly unrelated conditions. For instance, learning about strategies to manage Tourette syndrome in children highlights the importance of proactive management in neurological conditions, a concept equally applicable to preparing for a potential flu pandemic.
The preparedness needed for both scenarios underscores the need for robust public health systems.
Comparison to Previous Avian Influenza Outbreaks
Previous avian influenza outbreaks, such as the H5N1 outbreaks of the early 2000s, primarily resulted in sporadic human infections, largely linked to direct contact with infected birds. Human-to-human transmission was limited, preventing widespread outbreaks. The current situation differs significantly. The observed mutations in the H5N1 virus suggest a potential for increased and sustained human-to-human transmission, markedly increasing the risk of a pandemic.
The CDC’s warning about nine H5N1 bird flu mutations posing a pandemic threat is seriously unsettling. It makes you think about how vulnerable we are to unforeseen health crises, and how crucial early detection is in managing such threats. This got me wondering about early detection in other areas, like the fascinating research on whether an eye test, as discussed in this article can eye test detect dementia risk in older adults , could similarly provide a valuable early warning system.
The potential for early detection, whether it’s for a pandemic or dementia, highlights the importance of ongoing medical research and preparedness.
The scale and sustained nature of the current H5N1 circulation in birds also surpasses previous outbreaks, providing a larger and more persistent opportunity for the virus to evolve and adapt.
Potential Pandemic Impact
A pandemic caused by these mutated H5N1 strains could have a devastating impact. While precise predictions are challenging, modeling based on previous influenza pandemics and the current characteristics of the virus suggests a potentially large number of cases. The 1918 influenza pandemic, for instance, infected an estimated 500 million people globally, with a mortality rate exceeding 2.5%. While the mortality rate of the mutated H5N1 might differ, the potential for widespread infection, given its increased transmissibility, warrants serious concern.
Even a moderately high mortality rate, coupled with a large number of infections, could overwhelm healthcare systems and cause significant societal disruption. Furthermore, the economic impact of such a pandemic would be substantial, affecting global trade, travel, and various other sectors. The severity of the impact would also depend on factors like the speed of the pandemic’s spread, the effectiveness of any implemented mitigation strategies, and the availability of effective treatments and vaccines.
Current Surveillance and Monitoring Strategies
The global threat posed by H5N1 avian influenza necessitates a robust and multifaceted surveillance system. Effective monitoring is crucial not only for detecting outbreaks early but also for identifying potential mutations that could increase the virus’s transmissibility and virulence in humans. This involves a complex network of laboratories, veterinary services, and public health agencies working collaboratively across international borders.The current surveillance strategies rely on a multi-pronged approach, combining active and passive surveillance methods.
Active surveillance involves targeted sampling of poultry populations in high-risk areas, while passive surveillance relies on reporting of suspected cases by veterinarians, poultry farmers, and healthcare professionals. This system, while extensive, faces challenges in ensuring complete coverage, especially in regions with limited resources or infrastructure.
Avian Influenza Surveillance Methods
Detection and identification of H5N1 mutations utilize a range of sophisticated laboratory techniques. Samples from infected birds (or humans) are analyzed using real-time reverse transcription polymerase chain reaction (RT-PCR) to detect the presence of the virus. Further genetic sequencing is then conducted to determine the specific subtype and identify any mutations present. This process allows scientists to track the evolution of the virus and assess its potential for pandemic risk.
Phylogenetic analysis, comparing the genetic sequences of different isolates, helps to trace the spread of the virus and identify potential transmission routes. Advanced techniques like whole-genome sequencing provide even more detailed information about the viral genome, helping to identify mutations that might impact the virus’s properties.
International Collaboration in H5N1 Monitoring
International collaboration is paramount in the fight against H5N1. Organizations like the World Organisation for Animal Health (WOAH, formerly OIE), the World Health Organization (WHO), and the Food and Agriculture Organization of the United Nations (FAO) play critical roles in coordinating global surveillance efforts, sharing information, and providing technical assistance to countries. Data sharing platforms and early warning systems allow for rapid dissemination of information about outbreaks and emerging mutations, enabling a swift and coordinated response.
Joint research initiatives facilitate the development of improved diagnostic tools, vaccines, and antiviral drugs. These collaborations are essential for containing outbreaks and preventing the spread of the virus across borders. For example, the sharing of genomic data allows researchers globally to identify similar strains emerging in different parts of the world, enabling quicker responses and preventing the spread of highly pathogenic strains.
Enhanced Surveillance Strategy Proposal
An improved surveillance strategy should focus on strengthening several key areas. Firstly, increased investment in surveillance infrastructure, particularly in low- and middle-income countries, is crucial. This includes providing better laboratory capacity, training personnel, and improving disease reporting systems. Secondly, integrating advanced technologies, such as AI-powered predictive modeling and remote sensing technologies, can enhance early detection and improve response time. For instance, AI algorithms could analyze data from multiple sources to identify potential outbreaks before they are clinically apparent.
Thirdly, strengthening community engagement and public awareness campaigns are vital for improving early detection through prompt reporting of suspected cases. Finally, investing in research and development of novel diagnostic tools and therapeutics will help to ensure preparedness for future outbreaks. A proactive, data-driven approach, coupled with strengthened international collaborations, is essential to mitigating the risk posed by H5N1 avian influenza.
Public Health Preparedness and Response
The emergence of highly pathogenic avian influenza (H5N1) viruses with concerning mutations necessitates a robust and multifaceted public health response. This involves a coordinated effort at local, national, and international levels to minimize the risk of a human pandemic. Effective preparedness relies on proactive surveillance, rapid response mechanisms, and public education to empower individuals and communities to protect themselves.
Current public health measures aim to interrupt the transmission cycle of the virus, both in birds and potentially in humans. This includes enhanced surveillance of avian influenza in poultry populations, rapid detection and culling of infected birds, and strict biosecurity measures on poultry farms. For humans, contact tracing, isolation of infected individuals, and rigorous infection control protocols in healthcare settings are crucial components of the response strategy.
International collaboration is also essential for sharing information, coordinating research efforts, and ensuring a globally coordinated response to any potential outbreak.
Individual Protective Measures Against Avian Influenza
Protecting oneself from avian influenza involves minimizing contact with infected birds or contaminated environments. This means avoiding contact with wild birds, especially sick or dead ones, and practicing thorough hand hygiene after handling poultry or visiting live bird markets. Wearing appropriate personal protective equipment (PPE), such as masks and gloves, when handling poultry is also recommended. Thorough cooking of poultry to an internal temperature of at least 165°F (74°C) ensures the inactivation of the virus.
Staying informed about outbreaks and adhering to any public health advisories issued by local authorities is equally vital.
The Role of Vaccination and Antiviral Medications
Vaccination plays a crucial role in pandemic preparedness by providing a degree of protection against infection. While a widely available and effective human H5N1 vaccine is not currently available, research and development are ongoing, and stockpiling of vaccine candidates is a key aspect of preparedness strategies. The development of a vaccine is a complex process, requiring extensive testing to ensure both safety and efficacy.
Past experience with influenza pandemics has highlighted the importance of vaccine development and distribution capabilities.Antiviral medications, such as oseltamivir (Tamiflu) and zanamivir (Relenza), are essential tools in managing H5N1 infections. These drugs can reduce the severity and duration of illness, and they are crucial in preventing the spread of the virus. Stockpiling of antiviral medications is a key element of pandemic preparedness plans, ensuring sufficient supplies are available in case of a large-scale outbreak.
However, the effectiveness of antivirals can be impacted by the emergence of drug-resistant strains, emphasizing the need for continuous monitoring and development of new antiviral strategies.
Recommendations for Healthcare Professionals
Effective management of potential H5N1 cases requires healthcare professionals to be well-prepared and to follow strict infection control protocols. Early detection and prompt isolation of suspected cases are critical in preventing further transmission.
The following recommendations are essential for healthcare professionals dealing with potential H5N1 infections:
- Implement strict infection control measures, including the use of appropriate PPE (e.g., N95 respirators, gowns, gloves, eye protection).
- Maintain a high index of suspicion for H5N1 infection in patients presenting with influenza-like illness, especially those with a history of exposure to poultry or wild birds.
- Collect respiratory specimens for laboratory testing to confirm the diagnosis.
- Isolate suspected or confirmed cases in airborne infection isolation rooms.
- Administer antiviral medications as soon as possible after diagnosis.
- Implement contact tracing to identify and monitor individuals who may have been exposed to the infected patient.
- Provide education to patients and their families about infection prevention and control measures.
- Report all suspected cases to public health authorities immediately.
Research and Development Efforts: Cdc Raises Alarm Nine H5n1 Bird Flu Mutations Pose Pandemic Threat To Humans
The alarming mutations in the H5N1 avian influenza virus necessitate a robust and multifaceted research and development response. Global scientific efforts are intensely focused on developing effective countermeasures to mitigate the potential pandemic threat. This includes advancements in antiviral medications, vaccine development, diagnostic tools, and predictive modeling using genomic sequencing.The urgency of the situation has spurred significant investment in research initiatives worldwide.
Numerous research groups are collaborating internationally to share data, resources, and expertise to accelerate the development and deployment of effective tools to combat this evolving threat. This collaborative approach is crucial given the rapid mutation rate of the virus and the potential for unforeseen challenges.
Antiviral Drug Development
Current antiviral treatments, such as oseltamivir (Tamiflu) and zanamivir (Relenza), have limited efficacy against some H5N1 strains. Therefore, a major focus of research is the development of novel antiviral drugs with broader activity against a wider range of H5N1 subtypes and potentially resistant strains. This involves exploring different mechanisms of action, targeting various stages of the viral life cycle, and optimizing drug delivery methods.
The CDC’s warning about nine H5N1 bird flu mutations posing a pandemic threat is seriously unsettling. It makes you think about our vulnerability to novel diseases, especially considering how reliant we are on advancements like organ transplantation. The recent news that the FDA approved clinical trials for fda approves clinical trials for pig kidney transplants in humans is fascinating, but it also highlights the urgent need for robust pandemic preparedness alongside these medical breakthroughs.
We need to be ready for both emerging infectious diseases and the challenges of treating them.
For example, research into novel neuraminidase inhibitors and other classes of antiviral drugs is ongoing, aiming to overcome resistance mechanisms observed in some H5N1 strains. Preclinical studies are evaluating the efficacy and safety of these promising candidates.
Vaccine Development, Cdc raises alarm nine h5n1 bird flu mutations pose pandemic threat to humans
The development of effective H5N1 vaccines is critical for pandemic preparedness. Challenges include the need for vaccines that provide broad protection against diverse H5N1 strains and the rapid evolution of the virus. Researchers are exploring various vaccine platforms, including inactivated virus vaccines, live attenuated vaccines, and DNA/RNA vaccines, to overcome these challenges. Clinical trials are underway to assess the safety and efficacy of several candidate vaccines, including those designed to induce a strong and durable immune response.
The focus is on developing vaccines that are both highly effective and readily scalable for mass production to ensure rapid deployment in case of a pandemic.
Advancements in Diagnostic Tools and Technologies
Rapid and accurate diagnosis is crucial for effective containment of H5N1 outbreaks. Advancements in diagnostic technologies are improving the speed and sensitivity of detection. This includes the development of point-of-care diagnostic tests that can provide results quickly in resource-limited settings, as well as more sophisticated laboratory-based assays with enhanced sensitivity and specificity. For instance, the use of real-time polymerase chain reaction (PCR) assays has significantly improved the speed and accuracy of H5N1 detection.
Furthermore, advancements in next-generation sequencing technologies allow for rapid characterization of viral genomes, facilitating the monitoring of viral evolution and the identification of potential pandemic threats.
Genomic Sequencing and Modeling for Pandemic Prediction
Genomic sequencing is instrumental in tracking the evolution of H5N1 and predicting its potential to acquire characteristics that increase its transmissibility and pathogenicity in humans. By analyzing the genetic makeup of circulating H5N1 strains, researchers can identify mutations that confer increased virulence or transmissibility. This information is crucial for developing effective countermeasures and informing public health strategies. Mathematical modeling, using genomic data and epidemiological information, helps predict the potential trajectory of an outbreak, assisting in resource allocation and intervention strategies.
For example, models can simulate the spread of a virus under different scenarios, helping to determine the effectiveness of various interventions such as vaccination campaigns or social distancing measures. This predictive capability is crucial for effective pandemic preparedness and response.
Economic and Societal Impacts
The emergence of a pandemic caused by a highly pathogenic avian influenza virus, such as the mutated H5N1 strain, poses a significant threat not only to public health but also to the global economy and the fabric of societies worldwide. The economic consequences could be devastating, cascading through various sectors and impacting livelihoods on an unprecedented scale. Societal disruptions would be profound, stretching the capacity of healthcare systems and impacting essential services.The potential economic consequences of an H5N1 pandemic are multifaceted and far-reaching.
Direct costs would include the expenses associated with healthcare provision, such as hospitalizations, intensive care, and the development and deployment of vaccines and antiviral treatments. Indirect costs would be even more substantial, stemming from lost productivity due to illness and mortality, disruptions to supply chains, and decreased consumer spending. The tourism and travel industries would likely experience severe setbacks, as would the agricultural sector, particularly poultry farming.
Financial markets could also experience significant volatility, leading to potential economic recession.
Healthcare System Impacts
A pandemic would overwhelm healthcare systems globally. Hospitals would face a surge in patients requiring intensive care, potentially exceeding their capacity. Shortages of essential medical supplies, including ventilators and personal protective equipment (PPE), would exacerbate the situation. Healthcare workers would face immense pressure and risk of infection, leading to burnout and staff shortages. The strain on healthcare systems would not be limited to physical resources; mental health services would also be heavily burdened by the psychological impact of the pandemic on both patients and healthcare providers.
For example, during the COVID-19 pandemic, many hospitals were forced to implement crisis standards of care, prioritizing patients based on their likelihood of survival. A similar scenario, potentially even more severe, could unfold during an H5N1 pandemic.
Educational Disruptions
Educational institutions would be significantly impacted. School and university closures would be necessary to prevent the spread of the virus, disrupting learning and impacting students’ academic progress. The transition to online learning, while a viable option for some, would not be accessible to all students, particularly those from disadvantaged backgrounds lacking reliable internet access or appropriate technology. The long-term effects on educational attainment and the skills gap could have significant economic consequences.
The closure of schools during the COVID-19 pandemic provided a stark illustration of the widespread educational disruptions a pandemic can cause, with significant learning loss reported across various age groups.
Economic Sectoral Impacts
The economic impact would be felt across various sectors. The tourism and hospitality industries would suffer immensely due to travel restrictions and decreased consumer confidence. The agricultural sector, particularly poultry farming, would be severely affected by outbreaks and culling of infected birds. Manufacturing and supply chains would face disruptions due to workforce illness and logistical challenges. The financial sector could experience instability due to decreased consumer spending and investment.
The overall impact on the global economy would be significant, potentially leading to a global recession, similar to the economic downturn experienced following the 2008 financial crisis or the initial impact of the COVID-19 pandemic.
Potential Economic and Societal Impacts Table
| Sector | Potential Impact | Severity Level | Mitigation Strategies |
|---|---|---|---|
| Healthcare | Overwhelmed hospitals, shortages of medical supplies, healthcare worker burnout | High | Increased hospital capacity, stockpiling of medical supplies, support for healthcare workers |
| Education | School and university closures, disruption of learning, widening educational inequalities | Medium-High | Investment in online learning infrastructure, targeted support for disadvantaged students, flexible learning models |
| Tourism & Hospitality | Sharp decline in tourism, business closures, job losses | High | Financial aid for businesses, marketing campaigns to rebuild confidence, flexible travel policies |
| Agriculture | Outbreaks in poultry farms, culling of birds, food shortages | Medium | Improved biosecurity measures, development of resistant poultry breeds, diversification of food sources |
| Manufacturing & Supply Chains | Disruptions in production, delays in deliveries, shortages of goods | Medium-High | Diversification of supply chains, investment in automation, robust inventory management |
| Financial Sector | Market volatility, decreased consumer spending, economic recession | High | Financial aid packages, fiscal stimulus measures, regulatory support |
End of Discussion
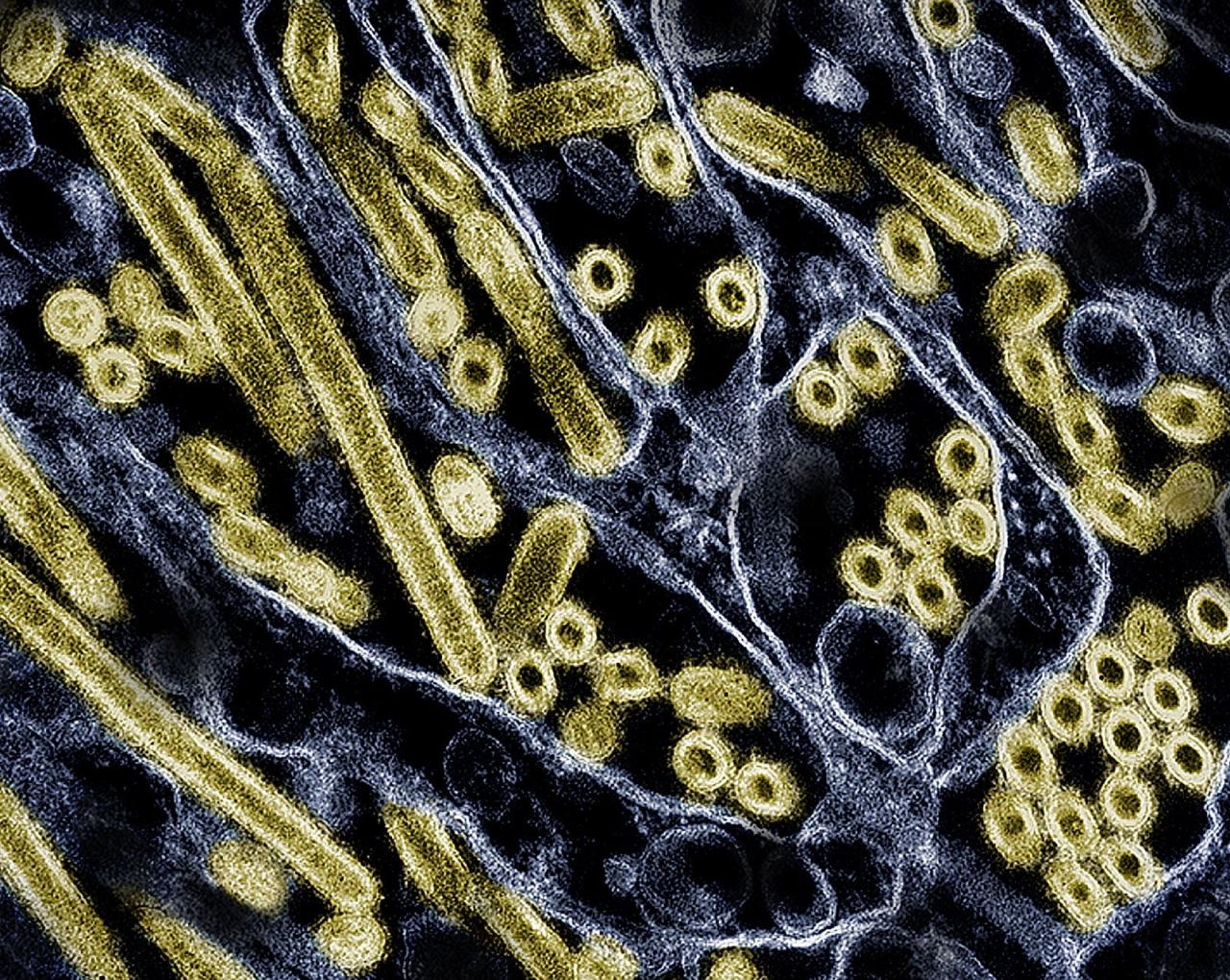
Source: cnn.com
The CDC’s alarm regarding the nine H5N1 bird flu mutations is a stark reminder of the ever-present threat of pandemics. While the situation is serious, it’s not a reason to panic. Instead, it’s a call to action. We need increased vigilance, robust surveillance systems, and global collaboration to monitor and control the spread of this virus. By understanding the risks, staying informed, and taking preventative measures, we can significantly reduce the potential impact of a future outbreak.
This isn’t just about the scientists and healthcare professionals; it’s about each and every one of us playing our part in protecting our global community.
FAQ Compilation
What are the symptoms of H5N1 infection?
Symptoms can vary but often include fever, cough, sore throat, muscle aches, and difficulty breathing. Severe cases can lead to pneumonia and respiratory failure.
How is H5N1 transmitted?
Primarily through close contact with infected birds. Human-to-human transmission is currently limited but a concern with the mutations.
Is there a vaccine for H5N1?
While not widely available for the public, research and development of vaccines are ongoing.
What can I do to protect myself?
Avoid contact with poultry, practice good hygiene (frequent handwashing), and follow public health advisories.
