An Inflection Point for Healthcare
An inflection point for healthcare: We’re witnessing a dramatic shift in how we approach health and wellness, driven by technological leaps, evolving demographics, and a fundamental change in the patient-provider dynamic. This isn’t just incremental change; it’s a fundamental reshaping of the entire healthcare landscape, impacting everything from diagnosis and treatment to cost and accessibility. This post explores the key forces driving this transformation and what it means for the future of health.
From the rise of AI-powered diagnostics and personalized medicine to the expanding role of telehealth and the growing power of the informed consumer, we’re entering an era where technology, economics, and ethical considerations are converging to redefine healthcare as we know it. We’ll delve into the challenges and opportunities presented by this revolution, examining how these forces are interacting to create a new paradigm for patient care and healthcare delivery.
Technological Advancements Reshaping Healthcare

Source: projectbodysmart.com
The healthcare landscape is undergoing a dramatic transformation, driven by rapid technological advancements. These innovations are not merely improving existing practices; they are fundamentally reshaping how we prevent, diagnose, treat, and manage diseases. This revolution promises to deliver more efficient, accessible, and personalized care, ultimately leading to better patient outcomes.
AI’s Impact on Diagnostic Accuracy and Treatment Planning
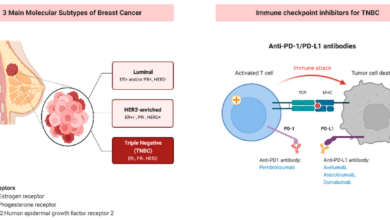
Artificial intelligence (AI) is rapidly changing the diagnostic process. AI algorithms, trained on massive datasets of medical images and patient records, can detect subtle patterns and anomalies that might be missed by the human eye. This leads to earlier and more accurate diagnoses, particularly in areas like radiology, pathology, and oncology. For instance, AI-powered systems are demonstrating impressive accuracy in detecting cancerous lesions in mammograms, often exceeding the performance of human radiologists.
Beyond diagnostics, AI is also improving treatment planning. By analyzing patient data, AI can help oncologists select the most effective chemotherapy regimens, predict treatment response, and personalize radiation therapy plans, ultimately optimizing treatment outcomes and minimizing side effects. The integration of AI into clinical workflows is still in its early stages, but the potential for improved accuracy and efficiency is immense.
Telehealth’s Role in Expanding Access to Care and Reducing Costs
Telehealth, the delivery of healthcare services remotely using technology, has emerged as a powerful tool for expanding access to care, particularly in underserved areas and for patients with mobility limitations. Video conferencing allows patients to consult with doctors from the comfort of their homes, eliminating the need for travel and reducing the time and expense associated with in-person visits.
Remote monitoring devices, such as wearable sensors and smart home technology, allow for continuous tracking of vital signs and other health metrics, enabling early detection of potential problems and proactive intervention. This approach can significantly reduce hospital readmissions and improve overall patient management. The cost-effectiveness of telehealth is also becoming increasingly evident, as it can lower expenses related to transportation, lost workdays, and hospital stays.
The COVID-19 pandemic dramatically accelerated the adoption of telehealth, demonstrating its effectiveness and flexibility in a crisis situation.
Personalized Medicine and its Implications for Patient Outcomes
Personalized medicine, also known as precision medicine, tailors medical treatment to the individual characteristics of each patient. This approach utilizes genetic information, lifestyle factors, and other data to identify the most effective treatment strategies for a specific patient. For example, genomic sequencing can identify genetic mutations that contribute to certain cancers, allowing doctors to select targeted therapies that are more likely to be effective and less toxic.
Pharmacogenomics uses genetic information to predict how patients will respond to different medications, minimizing adverse drug reactions and optimizing treatment efficacy. The ability to personalize treatment based on individual characteristics has the potential to significantly improve patient outcomes, reduce healthcare costs, and enhance the overall quality of life for patients with chronic diseases. While still in its early stages of development, personalized medicine holds immense promise for revolutionizing healthcare in the years to come.
Adoption Rates of Healthcare Technologies Across Countries
| Country | Technology | Adoption Rate | Impact |
|---|---|---|---|
| United States | AI in diagnostics | 25% | Improved diagnostic accuracy, faster turnaround times |
| United Kingdom | Telehealth | 40% | Increased access to care, reduced hospital readmissions |
| Canada | Personalized medicine (genomics) | 15% | Improved cancer treatment outcomes, reduced side effects |
| Germany | AI in drug discovery | 30% | Faster development of new drugs, reduced costs |
| Japan | Robotic surgery | 20% | Minimally invasive procedures, faster recovery times |
Shifting Demographics and Healthcare Needs
The healthcare landscape is undergoing a dramatic transformation, driven not only by technological advancements but also by profound shifts in demographics and the resulting changes in healthcare needs. An aging global population, coupled with rising rates of chronic diseases, is placing unprecedented strain on healthcare systems worldwide. Understanding these demographic shifts and their implications is crucial for developing effective and sustainable healthcare strategies.The increasing proportion of elderly individuals globally is significantly impacting healthcare resource allocation.
This demographic shift necessitates a substantial increase in resources dedicated to age-related conditions such as cardiovascular disease, dementia, arthritis, and cancer. The demand for geriatric care, including long-term care facilities and home healthcare services, is escalating rapidly. This increased demand often outpaces the capacity of existing healthcare systems, leading to longer wait times, increased costs, and potential compromises in the quality of care.
For example, in Japan, where the population is rapidly aging, the government is grappling with significant challenges in providing adequate elder care services, leading to a surge in demand for both public and private solutions.
Impact of Aging Population on Healthcare Resource Allocation
The aging population requires a significant reallocation of healthcare resources. This includes increased funding for geriatric specialists, expanded access to long-term care facilities, and the development of innovative technologies to support aging in place. Furthermore, a focus on preventative care and early intervention strategies can help mitigate the long-term burden on healthcare systems. For instance, increased investment in research on age-related diseases and the development of more effective treatments can significantly reduce the overall healthcare costs associated with managing these conditions.
The shift necessitates a paradigm change, moving from a predominantly reactive model to a more proactive and preventative approach to healthcare.
Growing Prevalence of Chronic Diseases and Their Effect on Healthcare Systems
The rise in chronic diseases, such as diabetes, heart disease, and cancer, presents a substantial challenge to healthcare systems globally. These conditions often require long-term management, resulting in ongoing healthcare costs and reduced productivity. The chronic nature of these illnesses necessitates a shift towards integrated care models that emphasize disease prevention, early detection, and coordinated management across various healthcare settings.
For instance, the increasing prevalence of type 2 diabetes is placing a significant burden on healthcare systems due to the high cost of managing its complications, including kidney disease, blindness, and amputations. Effective management requires a multifaceted approach, including lifestyle interventions, medication, and regular monitoring.
Strategies for Addressing Health Disparities Among Different Socioeconomic Groups
Significant health disparities exist across socioeconomic groups, with individuals from lower socioeconomic backgrounds often experiencing poorer health outcomes and reduced access to quality healthcare. Addressing these disparities requires a multi-pronged approach that tackles the social determinants of health, such as poverty, lack of education, and limited access to healthy food and safe housing. Investing in community-based programs that promote health literacy, improve access to affordable healthcare, and address social determinants of health is essential to reduce these disparities.
For example, initiatives that provide subsidized healthcare to low-income families, along with community education programs focusing on healthy lifestyle choices, can significantly improve health outcomes in underserved populations.
Healthcare’s at a major inflection point, grappling with evolving models and technological advancements. The recent news of AdventHealth CEO Terry Shaw’s retirement highlights the leadership changes impacting the industry’s trajectory. This shift, alongside broader industry trends, underscores just how transformative this period is for healthcare’s future.
Preventative Healthcare Measures Tailored to Specific Age Groups
Preventative healthcare is crucial for maintaining health and reducing the burden on healthcare systems. Tailoring preventative measures to specific age groups can maximize their effectiveness.
The following preventative healthcare measures are tailored to specific age groups:
- Children and Adolescents (0-18 years): Regular vaccinations, dental checkups, vision screenings, healthy eating habits promotion, physical activity encouragement, and mental health awareness.
- Young Adults (18-40 years): Regular checkups, screenings for sexually transmitted infections, cancer screenings (as appropriate), stress management techniques, and healthy lifestyle promotion.
- Middle-Aged Adults (40-65 years): Regular checkups, screenings for cholesterol, blood pressure, blood sugar, and cancer (as appropriate), bone density scans, vaccinations (influenza, shingles), and lifestyle modifications for cardiovascular health.
- Older Adults (65+ years): Regular checkups, screenings for age-related conditions, fall prevention strategies, vaccinations (influenza, pneumonia, shingles), medication reviews, and social engagement promotion.
Economic and Policy Changes Affecting Healthcare
The healthcare landscape is not just being reshaped by technological advancements and demographic shifts; it’s also undergoing a dramatic transformation driven by economic realities and evolving policy decisions. The rising cost of healthcare is a global concern, impacting access to care for millions and forcing governments and healthcare systems to seek innovative solutions. This section will explore the interplay between economic factors, policy changes, and their profound influence on healthcare delivery and affordability.Healthcare cost inflation significantly limits access to care.
The escalating costs of pharmaceuticals, medical procedures, and hospital stays create a financial barrier for many individuals and families, particularly those without comprehensive health insurance or those with high deductibles and co-pays. This often leads to delayed or forgone care, resulting in worse health outcomes and increased long-term costs. The gap between the cost of care and individual ability to pay widens, creating a significant challenge for both patients and the healthcare system as a whole.
This disparity is particularly pronounced in countries with limited public healthcare funding or those with high levels of uninsured individuals.
Innovative Payment Models Improving Efficiency and Affordability, An inflection point for healthcare
The unsustainable trajectory of healthcare costs has spurred the development of innovative payment models designed to incentivize efficiency and improve affordability. Value-based care, for example, shifts the focus from volume of services to the quality and outcomes of care. Instead of paying providers for each individual service rendered, value-based care models compensate providers based on the overall health of their patients and the achievement of specific quality metrics.
Another example is bundled payments, where providers receive a single payment for a specific episode of care, encouraging cost-effectiveness and coordination among different healthcare professionals. Accountable Care Organizations (ACOs) are another example, representing groups of providers who collaborate to deliver coordinated care to a defined population, aiming to improve quality and reduce costs. These models aim to address the fee-for-service model’s inherent incentives to provide more rather than better care.
Comparison of Healthcare Financing Systems Across Developed Nations
Developed nations employ diverse healthcare financing systems, each with its strengths and weaknesses. The United States, for example, relies heavily on a private insurance system supplemented by government programs like Medicare and Medicaid, leading to high overall healthcare spending and significant disparities in access to care. In contrast, Canada utilizes a single-payer system, where the government funds healthcare through taxes, providing universal access to essential services but potentially leading to longer wait times for certain procedures.
The United Kingdom’s National Health Service (NHS) is another single-payer system, with a greater emphasis on centralized planning and resource allocation. Germany’s system, a social health insurance model, mandates insurance coverage through non-profit sickness funds, offering a balance between government regulation and private provision. These differing approaches highlight the complex trade-offs between access, cost, and quality of care inherent in healthcare financing decisions.
Government Regulation’s Role in Shaping Healthcare Innovation
Government regulation plays a crucial role in shaping healthcare innovation, balancing the need to ensure safety and quality with the desire to foster competition and drive technological advancements. Regulations regarding drug approvals, medical device safety, and data privacy can significantly impact the speed and cost of bringing new technologies to market. While stringent regulations can ensure safety, they can also stifle innovation by increasing the time and resources required for product development and approval.
Conversely, a lack of regulation can lead to unsafe practices and compromised patient outcomes. Finding the right balance is a constant challenge, requiring careful consideration of the potential benefits and risks associated with different regulatory approaches. For instance, the FDA’s approval process for new drugs, while rigorous, ensures patient safety but can delay access to potentially life-saving medications.
This illustrates the ongoing tension between promoting innovation and safeguarding public health.
The Rise of Consumerism in Healthcare: An Inflection Point For Healthcare

Source: medium.com
The healthcare landscape is undergoing a dramatic shift, fueled by empowered patients who are increasingly demanding more control and personalization in their care. This rise of consumerism is reshaping the industry, pushing providers to adapt to new expectations and prioritize patient experience alongside clinical excellence. The factors driving this change are multifaceted and interconnected, impacting everything from how patients choose providers to how healthcare services are delivered and priced.Patient empowerment and the demand for personalized experiences are fueled by several key factors.
Increased access to health information online, coupled with a greater understanding of their own health conditions, has equipped patients with the knowledge to actively participate in their care decisions. The rise of telehealth and digital health tools has further contributed to this empowerment, giving patients more convenient access to information and care. Simultaneously, a growing emphasis on patient-centered care models, focusing on individual needs and preferences, is driving demand for personalized experiences.
This includes tailored treatment plans, customized communication styles, and greater flexibility in scheduling and access to care.
Patient Reviews and Online Ratings Influence Provider Selection
Online reviews and ratings have become a significant factor in how patients choose healthcare providers. Websites like Healthgrades, Vitals, and Zocdoc allow patients to share their experiences, rating providers on various aspects such as wait times, communication, and overall satisfaction. Positive reviews can significantly boost a provider’s reputation and attract new patients, while negative reviews can have a detrimental impact.
This system creates a powerful incentive for providers to prioritize patient satisfaction and deliver high-quality care. For example, a highly-rated orthopedic surgeon might see a significant increase in appointments compared to a similarly qualified surgeon with fewer or negative reviews, even if both offer the same level of clinical expertise. The transparency afforded by online platforms allows patients to make informed decisions based on the experiences of others.
Patient Engagement Strategies Improve Health Outcomes
Effective patient engagement strategies are crucial for improving health outcomes and enhancing the patient experience. These strategies involve actively involving patients in their care, fostering open communication, and empowering them to take an active role in managing their health. This might include providing patients with access to their medical records online, offering personalized education materials, and encouraging participation in shared decision-making.
Studies have shown that patients who are actively engaged in their care are more likely to adhere to treatment plans, resulting in better health outcomes and reduced healthcare costs. For instance, a patient with diabetes who actively participates in managing their blood sugar levels through regular monitoring and adherence to dietary guidelines will likely experience better long-term health outcomes compared to a patient who is less engaged in their care.
Transparency in Healthcare Pricing and Billing Enhances Consumer Trust
Lack of transparency in healthcare pricing and billing has long been a source of frustration for patients. The complexity of insurance plans and the often-unclear nature of medical bills can lead to confusion and distrust. Increasing transparency in pricing, by providing patients with clear and upfront estimates of costs before receiving services, can significantly enhance consumer trust. This can involve providing price lists for common procedures, offering online tools to estimate out-of-pocket expenses, and simplifying billing statements.
Initiatives like price transparency laws in some states are aiming to address this issue, promoting competition and empowering patients to make informed decisions about their healthcare spending. A clear understanding of costs can help patients choose the most cost-effective options while still receiving quality care, potentially leading to better financial planning and reduced medical debt.
Ethical Considerations in Healthcare Transformation
The rapid advancement of technology in healthcare presents incredible opportunities to improve patient care, but it also raises complex ethical dilemmas that demand careful consideration. Navigating this new landscape requires a proactive and thoughtful approach, balancing innovation with the fundamental principles of medical ethics. Ignoring these ethical considerations risks undermining public trust and hindering the potential benefits of technological progress.
Ethical Challenges of Artificial Intelligence in Healthcare
The integration of AI into healthcare, while promising, introduces several ethical challenges. One key concern is algorithmic bias. AI algorithms are trained on data, and if that data reflects existing societal biases (e.g., racial, socioeconomic), the AI system will perpetuate and even amplify those biases in its diagnoses and treatment recommendations. This can lead to disparities in care, disproportionately affecting vulnerable populations.
Another challenge is accountability. When an AI system makes an error, determining responsibility – whether it lies with the developers, the healthcare providers, or the AI itself – can be difficult and legally murky. Finally, the “black box” nature of some AI algorithms makes it challenging to understand how they arrive at their conclusions, hindering transparency and trust.
We’re definitely at an inflection point for healthcare, facing massive shifts in financing and delivery models. The recent news that Steward Health Care secured financing to navigate its bankruptcy, as reported by this article , highlights the precarious financial state of some major players. This instability underscores the urgent need for innovative, sustainable solutions to ensure accessible and affordable healthcare for everyone going forward.
It’s a critical moment for reform.
For example, an AI system might recommend a specific treatment, but without a clear explanation of its reasoning, clinicians might be hesitant to rely on it.
Data Privacy and Security in Digital Health
The increasing reliance on digital health technologies generates massive amounts of sensitive patient data. Protecting this data from unauthorized access, use, or disclosure is paramount. Data breaches can have devastating consequences, not only for individuals whose privacy is violated but also for the healthcare institutions involved. The ethical implications extend beyond simple breaches; the very collection and use of patient data raise questions about informed consent, data minimization, and the potential for data misuse for purposes other than healthcare.
Regulations like HIPAA in the US attempt to address these concerns, but the rapid evolution of technology often outpaces regulatory frameworks. For instance, the use of wearable health trackers raises questions about who owns and controls the data collected, and whether that data can be shared with third parties without explicit consent.
Approaches to Managing Healthcare Data Ethically
Several approaches aim to manage healthcare data ethically. One approach emphasizes data anonymization and de-identification techniques to protect individual privacy while still allowing for data analysis and research. Another focuses on robust data security measures, including encryption, access controls, and regular security audits. A third approach emphasizes transparency and patient control, giving individuals greater access to and control over their own health data.
These approaches are not mutually exclusive; a comprehensive ethical framework requires a combination of technical safeguards, legal frameworks, and ethical guidelines that prioritize patient autonomy and data protection. For example, the implementation of blockchain technology could enhance data security and transparency by providing an immutable record of data access and use.
Patient autonomy and informed consent are fundamental ethical principles that must be upheld in the age of advanced medical technology. Patients have the right to understand the risks and benefits of any procedure or treatment, including those involving AI or other digital health technologies, and to make informed decisions about their own care.
The Future of Healthcare Workforce
The healthcare industry stands at a precipice. Technological advancements, shifting demographics, and evolving patient expectations are reshaping the landscape, demanding a fundamental shift in the skills, training, and structure of the healthcare workforce. Meeting these challenges requires a proactive and multifaceted approach, focusing on upskilling existing professionals, attracting new talent, and leveraging technology to optimize efficiency and effectiveness.
Skills and Training for Healthcare Professionals
The rapidly evolving healthcare environment necessitates a continuous cycle of learning and adaptation for healthcare professionals. Traditional medical training is no longer sufficient. Professionals must develop proficiency in data analysis, technological integration, and patient communication skills tailored to the digital age. This includes competency in electronic health records (EHR) systems, telehealth platforms, and various diagnostic and therapeutic technologies.
We’re definitely at an inflection point for healthcare, aren’t we? The accessibility and affordability of quality care is a huge issue, and innovative models are crucial. One example that caught my eye is the partnership between Humana and Walmart, offering humana centerwell primary care centers walmart , bringing convenient primary care to more people. This kind of collaboration could be a game-changer, pushing us toward a more accessible and efficient healthcare system for the future.
Ultimately, this signifies a major shift in how we approach healthcare delivery.
Furthermore, strong interpersonal and communication skills remain crucial, particularly given the rise of patient empowerment and the need for shared decision-making. Specific training programs should focus on areas like data interpretation from AI-powered diagnostic tools, ethical considerations surrounding AI in healthcare, and the nuances of virtual patient interactions. For instance, a physician specializing in cardiology needs training not only in advanced cardiac procedures but also in interpreting data from wearable sensors and remotely monitoring patient health through telehealth platforms.
Automation and AI in Healthcare
Automation and artificial intelligence (AI) are poised to significantly augment the roles of healthcare workers, not replace them. AI can handle repetitive tasks such as data entry, appointment scheduling, and preliminary diagnosis analysis, freeing up healthcare professionals to focus on complex cases and patient interaction. Robotic surgery, AI-powered diagnostic tools, and personalized medicine algorithms are already transforming healthcare delivery.
However, the integration of these technologies requires careful consideration of ethical implications and the need for human oversight. For example, radiologists can use AI to pre-screen medical images, highlighting potential abnormalities for more detailed review, thus improving efficiency and accuracy without replacing the radiologist’s expertise. The role of the healthcare professional shifts from performing routine tasks to overseeing and interpreting AI-generated data, ensuring accuracy and addressing exceptional cases.
Impact of Workforce Shortages on Healthcare Access and Quality
The healthcare industry is facing a significant workforce shortage across various specialties. This shortage impacts access to care, leading to longer wait times for appointments, reduced availability of specialists, and potential compromises in the quality of services. The shortage is particularly acute in rural and underserved areas, exacerbating existing health disparities. Strategies to address this include increasing funding for medical education and training, creating incentives for healthcare professionals to work in underserved areas, and promoting the adoption of telehealth to expand access to care.
For example, the implementation of telehealth programs can allow specialists in urban centers to remotely consult with patients in rural communities, bridging the geographical gap and improving access to specialized care. This requires investment in robust telehealth infrastructure and training programs for healthcare professionals to effectively utilize these technologies.
Innovative Telehealth Training Program
An innovative training program for telehealth professionals should incorporate a blended learning approach, combining online modules, hands-on simulations, and mentored practical experience. The curriculum would cover technical skills, such as using telehealth platforms and managing virtual patient interactions, as well as soft skills, such as effective communication and empathy in a remote setting. The program would include simulated scenarios, allowing trainees to practice managing various clinical situations remotely.
Mentorship from experienced telehealth professionals would provide guidance and support throughout the training process. A crucial component would be a focus on ethical considerations and patient privacy in the context of telehealth, ensuring that trainees understand and adhere to best practices. Graduates of this program would be equipped with the skills and confidence to provide high-quality healthcare remotely, contributing to improved access and quality of care, particularly in underserved areas.
For instance, a module could focus on the legal and ethical considerations of prescribing medication remotely, including the necessary documentation and safeguards to ensure patient safety. Another module could simulate a virtual consultation with a patient experiencing a medical emergency, requiring the trainee to assess the situation, provide immediate instructions, and coordinate with emergency medical services.
Ultimate Conclusion

Source: globalheroes.com
The future of healthcare is undeniably bright, but the path forward requires careful navigation. Successfully navigating this inflection point necessitates a collaborative effort involving healthcare providers, policymakers, technology developers, and patients themselves. Embracing innovation while addressing ethical concerns and ensuring equitable access to care will be crucial in building a healthcare system that is both effective and compassionate.
The changes we’re witnessing are profound, and the choices we make today will shape the health and well-being of generations to come.
Detailed FAQs
What is meant by “inflection point” in the context of healthcare?
It refers to a point of significant and rapid change, marking a transition to a fundamentally different state. In healthcare, this means a period of accelerated transformation driven by various factors.
How will AI impact my doctor’s ability to treat me?
AI can improve diagnostic accuracy, personalize treatment plans, and even assist with surgery, leading to better outcomes and more efficient care. However, human oversight and ethical considerations remain crucial.
Will telehealth replace traditional doctor visits entirely?
Unlikely. Telehealth offers convenient access for certain situations, but in-person care will still be necessary for many medical needs. It’s more about supplementing, not replacing, traditional care.
How can I protect my health data in this increasingly digital world?
Be mindful of where you share your information, choose reputable providers, and understand your rights regarding data privacy. Look for providers with strong security measures.