California MediCal Medicaid Contracts Explained
California MediCal Medicaid contracts are a complex but fascinating system shaping healthcare access for millions. Understanding how these contracts are negotiated, awarded, and monitored is crucial for anyone involved in, or affected by, California’s healthcare landscape. This post dives into the intricacies of these contracts, exploring everything from eligibility criteria to the financial implications for providers and patients alike.
We’ll unravel the key players, the processes, and the potential impact on healthcare access and quality.
From the state government’s perspective, managing these contracts involves balancing budgetary constraints with the need to ensure adequate and quality care for recipients. For health plans, it’s a matter of strategic planning, efficient resource allocation, and maintaining strong provider networks. Providers, in turn, navigate the complexities of participation requirements, reimbursement rates, and performance metrics. The interplay of these diverse interests creates a dynamic and often challenging environment.
Overview of California Medi-Cal
Source: patch.com
California Medi-Cal, the state’s Medicaid program, provides healthcare coverage to millions of low-income residents. It’s a complex system with a multifaceted structure and a constantly evolving landscape of benefits and eligibility requirements. Understanding its intricacies is crucial for both recipients and those involved in its administration.California’s Medi-Cal program is jointly administered by the California Department of Health Care Services (DHCS) and the counties.
The DHCS sets the overall policies and guidelines, while the counties are responsible for local administration, including eligibility determination and case management. This shared responsibility creates a layered system, with both state-level oversight and localized implementation.
Types of Medi-Cal Coverage
Medi-Cal offers a variety of coverage options tailored to different populations. These options aren’t mutually exclusive; individuals may qualify for multiple benefits simultaneously. For example, a pregnant woman might qualify for both standard Medi-Cal and the Prenatal Care program. The specific benefits covered can vary depending on the individual’s specific coverage type. Common coverage types include: full-scope Medi-Cal, which provides comprehensive healthcare services; Medi-Cal for pregnant women and children; and Medi-Cal for seniors and people with disabilities.
There are also specialized programs focused on specific health conditions or demographics.
Medi-Cal Eligibility Criteria
Eligibility for Medi-Cal benefits hinges primarily on income and resource limits. These limits are adjusted periodically to reflect changes in the cost of living. Applicants must meet specific income and resource requirements, which are based on family size and the applicant’s income. Additionally, certain categories of individuals are automatically eligible, such as pregnant women, children, and individuals with disabilities who meet specific criteria.
Immigrant status also plays a role in eligibility, with some limitations applying to certain non-citizen groups. The application process involves submitting documentation verifying income, assets, and identity.
Historical Overview of Medi-Cal Changes
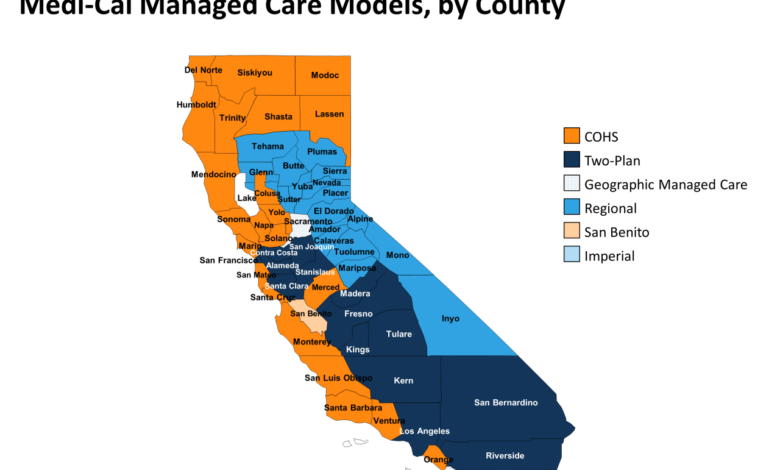
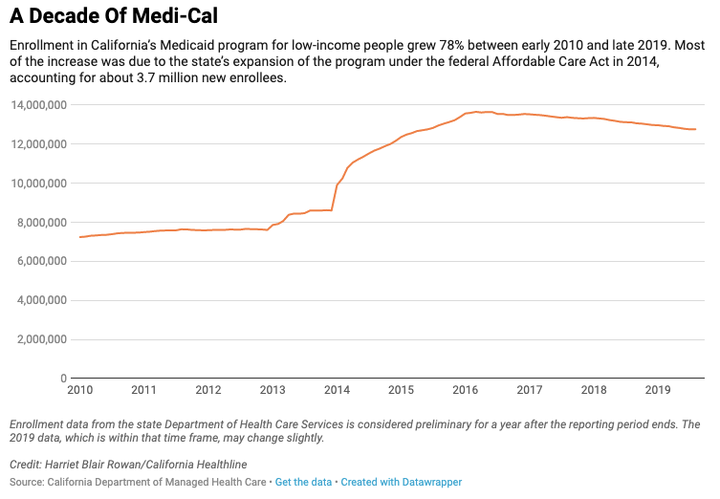
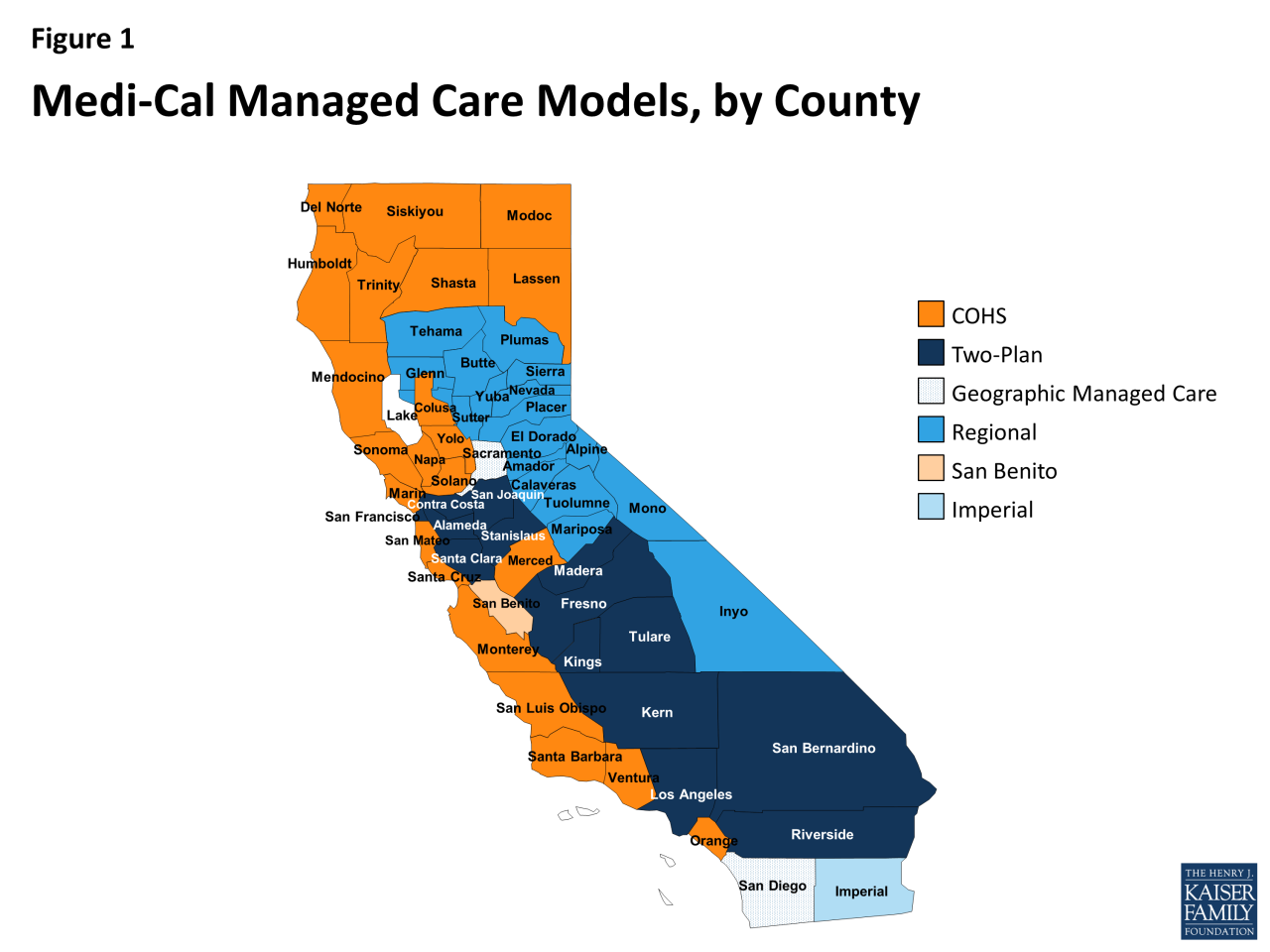
The California Medi-Cal program has undergone significant transformations throughout its history. Initially established with a narrower scope, it has expanded considerably over time to include a broader range of services and a larger population. For instance, the Affordable Care Act (ACA) led to significant expansions in Medi-Cal eligibility, enrolling millions of previously uninsured Californians. Other notable changes include the introduction of managed care, which shifted a substantial portion of Medi-Cal administration to private health plans, and ongoing efforts to improve the quality of care and reduce healthcare costs.
These ongoing adjustments reflect the program’s constant adaptation to meet the evolving needs of the state’s population and the changing healthcare landscape.
Medi-Cal Managed Care Contracts
Navigating the complex world of California’s Medi-Cal system requires understanding its managed care contracts. These contracts are the backbone of how millions of Californians receive healthcare coverage, outlining the agreements between the state and the health plans responsible for delivering services. This section delves into the key aspects of these crucial agreements.The California Department of Health Care Services (DHCS) plays a central role in Medi-Cal managed care contracting.
Key Players in Medi-Cal Managed Care Contracting
The Medi-Cal managed care system involves a complex interplay of key players. The DHCS, as the state agency administering the Medi-Cal program, is the primary contracting entity. They are responsible for establishing the program’s parameters, issuing requests for proposals (RFPs), and overseeing the performance of the health plans. Health plans, both large and small, are the other major players.
These plans bid for contracts to serve Medi-Cal beneficiaries within specific geographic regions. They are responsible for managing the care of their assigned enrollees, negotiating rates with providers, and ensuring access to quality healthcare services. Finally, healthcare providers – physicians, hospitals, and other medical professionals – are essential participants, as they deliver care to Medi-Cal beneficiaries under contracts with the health plans.
The Medi-Cal Managed Care Contracting Process, California MediCal Medicaid contracts
The process of awarding Medi-Cal managed care contracts is rigorous and competitive. It typically begins with the DHCS issuing a detailed RFP, outlining the state’s requirements and expectations for health plans. Health plans then submit proposals outlining their plans for delivering care, including their provider networks, quality improvement strategies, and financial viability. The DHCS evaluates these proposals based on a variety of factors, including the plan’s ability to meet the needs of the Medi-Cal population, its financial stability, and its commitment to quality care.
The process often involves multiple stages of review and negotiation before contracts are ultimately awarded.
Types of Medi-Cal Managed Care Contracts
Medi-Cal utilizes several types of contracts to reimburse health plans for the care they provide. The most common type is capitation. Under a capitation contract, health plans receive a fixed monthly payment per enrollee, regardless of the amount of services provided. This incentivizes plans to manage care efficiently and prevent unnecessary utilization. Fee-for-service contracts, while less prevalent in Medi-Cal managed care, also exist.
In these contracts, health plans are reimbursed for each individual service provided to an enrollee. The choice of contract type depends on the specific circumstances and goals of the DHCS and the health plan.
Performance Metrics for Evaluating Managed Care Plans
The DHCS employs a comprehensive set of performance metrics to evaluate the performance of Medi-Cal managed care plans. These metrics cover a broad range of areas, including access to care, quality of care, member satisfaction, and cost-effectiveness. Examples of key performance indicators (KPIs) include rates of preventative care, hospital readmission rates, patient satisfaction scores, and the efficiency of care coordination.
Regular monitoring and evaluation of these metrics ensure that health plans are meeting their contractual obligations and providing high-quality care to Medi-Cal beneficiaries. Plans that consistently fail to meet performance standards may face penalties or even contract termination.
Contract Negotiation and Award
The negotiation and award process for California Medi-Cal managed care contracts is a complex undertaking, involving intricate discussions between the state’s Department of Health Care Services (DHCS) and prospective health plans. This process aims to secure the best possible healthcare coverage for Medi-Cal beneficiaries while ensuring the financial viability of the participating health plans. The ultimate goal is a contract that balances the needs of the state and the capabilities of the health plans.The negotiation process itself is iterative, often involving multiple rounds of proposals, counter-proposals, and clarifications.
DHCS typically starts with a Request for Proposals (RFP), outlining the state’s requirements and expectations for managed care services. Health plans then submit detailed proposals, outlining their service delivery models, provider networks, and financial projections. Subsequent negotiation rounds focus on refining these proposals, addressing any discrepancies or ambiguities, and arriving at mutually agreeable terms. This often involves extensive data analysis, legal review, and discussions between DHCS representatives and the health plan’s negotiation team.
Key Provisions in Medi-Cal Managed Care Contracts
Medi-Cal managed care contracts typically include a comprehensive array of provisions covering various aspects of healthcare delivery and financial management. These provisions are crucial in ensuring accountability, transparency, and the provision of high-quality care. A key aspect is the definition of the scope of services to be provided, outlining the specific medical benefits covered under the contract. This often includes details about the types of providers included in the health plan’s network, access standards for beneficiaries, and quality assurance measures.
Further provisions often encompass financial arrangements, such as capitation rates (payments per member per month), risk-sharing mechanisms, and reporting requirements. Contracts also typically detail performance standards, penalties for non-compliance, and dispute resolution processes. Finally, contract terms and conditions usually include termination clauses, specifying the circumstances under which either party can terminate the agreement.
Comparison of Contract Terms and Conditions
Different Medi-Cal managed care contracts can vary significantly in their terms and conditions, reflecting the unique characteristics of the health plans and the specific needs of the populations they serve. For instance, contracts for plans serving geographically diverse regions might incorporate provisions related to transportation assistance or access to specialized care in rural areas. Similarly, contracts with plans specializing in specific populations (e.g., those with behavioral health needs) will include detailed provisions addressing those specific healthcare requirements.
Negotiating California MediCal Medicaid contracts can be a real headache, requiring careful consideration of provider reimbursements and patient access. It makes me think about the recent new york state nurse strike NYSNA Montefiore Mount Sinai , highlighting how crucial fair compensation is for healthcare workers. The struggles faced by those nurses underscore the importance of robust, equitable contracts in California’s MediCal system, ensuring both quality care and fair wages.
These variations often reflect differences in risk adjustment methodologies, where plans serving populations with higher healthcare needs receive adjusted payments to reflect the increased cost of care. Another key difference can be seen in the length of the contract term itself; some contracts may be for a shorter period, allowing for greater flexibility and adaptation to changing circumstances, while others may span several years, offering greater stability and predictability for both parties.
Navigating the complexities of California MediCal Medicaid contracts can be a real headache, especially when considering how to best utilize technology. I recently stumbled upon a fascinating study, study widespread digital twins healthcare , that suggests digital twins could revolutionize patient care. This got me thinking about how such technology could streamline processes and improve efficiency within the MediCal system, potentially leading to better contract management and patient outcomes.
Challenges and Risks in Contract Negotiation
Negotiating Medi-Cal managed care contracts presents several potential challenges and risks. One major challenge is balancing the state’s desire for comprehensive and affordable healthcare with the health plans’ need for financial viability. This often involves complex negotiations regarding capitation rates and risk-sharing mechanisms. Another challenge arises from the need to ensure equitable access to care for all Medi-Cal beneficiaries, regardless of their location or health status.
This requires careful consideration of provider network adequacy and the development of strategies to address health disparities. Furthermore, the constantly evolving healthcare landscape introduces complexities. Changes in healthcare regulations, technological advancements, and fluctuations in the healthcare market can impact the contract’s feasibility and necessitate adjustments throughout the contract’s duration. Finally, legal and regulatory compliance is paramount; failure to adhere to state and federal regulations can result in significant penalties and reputational damage.
Provider Network Participation
Source: kff.org
Getting your medical practice involved in the California Medi-Cal managed care network is a significant undertaking, but it can also be a rewarding way to serve a large and diverse patient population. This process involves understanding the requirements, navigating the application, and adhering to ongoing responsibilities. Successful participation hinges on a clear understanding of the network’s needs and your practice’s capabilities.
The process for providers to participate in Medi-Cal managed care networks typically begins with an application submitted to the specific health plan. Each plan has its own enrollment process, which usually involves completing a detailed application form, providing documentation to verify credentials and licensure, and agreeing to the terms and conditions of the contract. The application will likely require information about your practice’s location, specialties, staffing, and capacity.
After submitting the application, you’ll typically undergo a credentialing process that involves verifying your information and ensuring compliance with Medi-Cal’s requirements. This process can take several months. Once credentialing is complete and the contract is signed, your practice will be included in the health plan’s provider directory, making your services accessible to Medi-Cal beneficiaries.
Provider Requirements and Responsibilities
Participating in the Medi-Cal network comes with specific requirements and responsibilities. Providers must adhere to all applicable state and federal regulations, including those related to patient privacy (HIPAA), billing practices, and quality of care. They are also required to maintain accurate records, participate in quality improvement initiatives, and comply with the health plan’s operational guidelines. Failure to meet these requirements can result in contract termination or sanctions.
For example, a provider might be required to submit claims electronically, use a specific billing code set, or participate in utilization management programs designed to ensure cost-effectiveness and appropriate care. These responsibilities ensure that Medi-Cal beneficiaries receive high-quality, accessible, and affordable care.
Network Adequacy and Access to Care
Network adequacy is a critical factor in ensuring access to care for Medi-Cal beneficiaries. Health plans are required to maintain a sufficient number of providers in each geographic area to meet the needs of their enrolled population. This includes ensuring a diverse range of specialties and services are available. Insufficient network adequacy can lead to difficulties for beneficiaries in accessing timely and appropriate care, potentially impacting their health outcomes.
For instance, a lack of specialists in a rural area could mean significant delays or barriers for patients requiring specialized care. Regular monitoring of network adequacy, through measures like provider-to-patient ratios and wait times, is essential for ensuring access to care.
Factors Influencing Provider Participation Decisions
Several factors influence a provider’s decision to participate in the Medi-Cal managed care network. These factors can be broadly categorized into financial considerations, administrative burdens, and the impact on patient care.
Financial considerations are often paramount. Reimbursement rates, payment timelines, and the potential volume of Medi-Cal patients all play a significant role. Administrative burdens, such as the complexity of the enrollment process, ongoing reporting requirements, and the potential for denials or delays in payment, can also deter providers. Finally, the potential impact on patient care, including the ability to provide comprehensive care to a diverse population and the potential for increased patient volume, is a key factor.
Financial Aspects of Medi-Cal Contracts
Navigating the financial landscape of Medi-Cal managed care contracts requires a thorough understanding of reimbursement methodologies, risk-sharing mechanisms, and the overall financial implications for both health plans and providers. This section delves into these crucial aspects, providing a clearer picture of the complexities involved.
Medi-Cal Reimbursement Methodologies
Medi-Cal utilizes various reimbursement methodologies in its managed care contracts, aiming to balance cost-effectiveness with quality of care. These methods often involve capitation, fee-for-service, and various value-based payment models. Capitation, a common approach, pays health plans a fixed amount per member per month (PMPM), regardless of the services rendered. This incentivizes efficient care management and preventative services.
Fee-for-service, on the other hand, reimburses providers for each individual service provided, based on pre-established rates. Value-based payment models, increasingly prevalent, tie reimbursement to the quality of care delivered and the achievement of specific health outcomes. These models incentivize health plans and providers to focus on improving patient health and reducing costs. The specific reimbursement methodology employed varies depending on the contract and the type of service provided.
Risk Sharing Between the State and Health Plans
Risk sharing in Medi-Cal managed care contracts is a critical component. The state and health plans share the financial risk associated with providing healthcare services to Medi-Cal beneficiaries. This sharing can take various forms, including global capitation, where the health plan receives a fixed PMPM payment for all services, bearing the risk of exceeding costs. Alternatively, risk sharing might involve partial capitation, with the state retaining some risk for high-cost services, or even stop-loss provisions, which protect the health plan from catastrophic losses.
The specific risk-sharing arrangement depends on the contract’s terms and the state’s overall risk management strategy. For example, a global capitation contract might place a greater financial burden on the health plan in the event of unexpected increases in healthcare utilization or costs, while a partial capitation contract would distribute this risk more evenly.
Navigating the complexities of California MediCal Medicaid contracts can be a real headache for providers. Efficiency is key, and that’s where advancements like the integration of AI into EHRs become crucial. Check out this article on how Nuance integrates generative AI scribe with Epic EHRs: nuance integrates generative ai scribe epic ehrs. This kind of tech could significantly streamline documentation, freeing up time for providers to focus on patient care and successfully managing those MediCal contracts.
Financial Implications of Contract Terms
Contract terms significantly influence the financial viability of both health plans and providers. For health plans, favorable reimbursement rates and efficient risk-sharing arrangements are crucial for profitability. Conversely, unfavorable terms can lead to financial losses. Providers, too, are significantly affected by reimbursement rates and the terms of their participation in health plan networks. Low reimbursement rates can impact their financial stability and ability to provide quality care.
Contract terms related to network adequacy, utilization management, and quality metrics also play a crucial role in shaping the financial performance of both health plans and providers. For instance, a contract requiring a large provider network might necessitate significant upfront investment for the health plan, while restrictive utilization management policies could limit provider revenue.
Medi-Cal Reimbursement Rates for Different Services
The following table provides a simplified comparison of reimbursement rates for selected services under Medi-Cal. Note that these rates can vary significantly based on geographic location, provider type, and specific contract terms. The data is illustrative and should not be considered exhaustive or definitive. Actual rates should be obtained from official Medi-Cal sources.
| Service | Primary Care Physician Visit | Specialist Visit | Hospital Inpatient Day |
|---|---|---|---|
| Average Reimbursement Rate (Example) | $100 | $150 | $2000 |
| Notes | Rates vary widely by location and provider type. | May include additional charges for procedures. | Depends on diagnosis, length of stay, and hospital location. |
Contract Monitoring and Enforcement: California MediCal Medicaid Contracts
California Medi-Cal’s robust contract monitoring and enforcement system ensures accountability and protects the integrity of the program. This system involves a multi-faceted approach, encompassing regular audits, performance reviews, and dispute resolution mechanisms to guarantee that health plans adhere to the terms of their contracts and provide quality care to Medi-Cal beneficiaries.The state employs several methods to monitor compliance. These include regular data analysis of claims submitted by health plans, on-site audits of health plan operations, and reviews of health plan performance against pre-defined Key Performance Indicators (KPIs).
The Department of Health Care Services (DHCS) utilizes sophisticated data analytics tools to identify potential areas of non-compliance and triggers more in-depth investigations as needed. Furthermore, DHCS employs a team of auditors and compliance specialists dedicated to reviewing health plan practices and ensuring adherence to contractual obligations.
Methods of Monitoring Compliance
The DHCS utilizes a variety of methods to monitor compliance with Medi-Cal contract terms. These include, but are not limited to, regular data analysis of claims data to identify patterns of potential fraud, waste, or abuse; on-site audits to assess health plan operations and compliance with contractual requirements; and the ongoing review of health plan performance reports, which include various KPIs.
Data analysis might reveal discrepancies in billing practices, unusual referral patterns, or inconsistencies in the provision of services. On-site audits allow for a direct examination of health plan processes, records, and staff training. Regular performance reports provide a longitudinal view of a health plan’s adherence to contractual obligations.
Consequences of Non-Compliance
Failure to comply with Medi-Cal contract requirements can result in a range of consequences, from financial penalties to contract termination. These consequences are designed to incentivize compliance and protect the interests of Medi-Cal beneficiaries. Examples of non-compliance include failing to meet quality standards, inadequate provider networks, or submitting inaccurate claims data. The severity of the penalties imposed is typically proportionate to the nature and extent of the non-compliance.
For example, minor infractions might result in written warnings or small financial penalties, while more serious breaches could lead to significant financial penalties, suspension of payments, or even contract termination.
Dispute Resolution Mechanisms
Medi-Cal contracts typically Artikel a structured process for resolving disputes between the state and health plans. This often involves a series of escalating steps, starting with informal negotiations and progressing to formal mediation or arbitration if necessary. The goal is to resolve disputes efficiently and fairly, minimizing disruptions to the provision of healthcare services. For example, a dispute might arise regarding the interpretation of a specific contractual clause or disagreement over the appropriateness of a financial penalty.
The contract typically specifies the procedures for escalating the dispute and identifying a neutral third party to facilitate a resolution if needed.
Key Performance Indicator (KPI) Tracking System
A robust KPI tracking system is essential for effective contract monitoring. This system should track key metrics related to access to care, quality of care, member satisfaction, and cost-effectiveness. Examples of KPIs might include the percentage of members receiving timely access to primary care, the rate of hospital readmissions, member satisfaction scores from surveys, and the per-member per-month (PMPM) cost of care.
Data on these KPIs should be collected regularly, analyzed, and reported to DHCS. This data is then used to assess health plan performance, identify areas needing improvement, and inform contract renewal decisions. The system should also include a mechanism for identifying and addressing outliers or trends indicating potential problems. A dashboard summarizing key performance indicators would allow for efficient monitoring and prompt identification of areas requiring attention.
Impact on Healthcare Access and Quality
Medi-Cal managed care contracts significantly influence both access to and quality of healthcare services for California’s low-income residents. The shift from a fee-for-service model to managed care aimed to improve efficiency and cost-effectiveness, but its impact on access and quality is complex and multifaceted, varying depending on contract design and implementation.The implementation of managed care has, in many instances, improved access to care by offering comprehensive services through coordinated networks of providers.
However, challenges remain, particularly in ensuring equitable access across geographic areas and for specific vulnerable populations. The quality of care delivered under these contracts is also a subject of ongoing evaluation and improvement efforts. Understanding the nuances of these relationships is crucial for policymakers and stakeholders involved in shaping the future of California’s healthcare system.
Medi-Cal Managed Care Contracts and Healthcare Access
Managed care contracts, by their nature, aim to improve access to care by organizing providers into networks. This theoretically streamlines referrals, reduces administrative burden, and enhances coordination of care. However, the reality can be more nuanced. Network adequacy, the sufficient number of providers within a geographically accessible area, is a key determinant of access. If a network lacks sufficient specialists or primary care physicians in a particular region, patients may face difficulties accessing needed services, potentially leading to delayed or forgone care.
Furthermore, restrictions on provider choice within the network, while aiming for cost control, can limit patient autonomy and satisfaction. The impact of these factors can disproportionately affect individuals in rural or underserved areas, where provider density is already low.
Medi-Cal Contracts and Quality of Care
The relationship between Medi-Cal contracts and quality of care is complex and not always straightforward. While managed care organizations (MCOs) are incentivized to improve quality through performance-based payments and quality metrics, concerns remain about the potential for cost-cutting measures to compromise the quality of care. For example, focusing on reducing hospital readmissions might lead to insufficient post-discharge support, impacting patient outcomes.
Furthermore, the use of standardized quality measures may not fully capture the nuances of individual patient needs and experiences. Robust quality monitoring and oversight are therefore crucial to ensure that cost savings do not come at the expense of patient well-being. Independent audits and data analysis are essential to track key quality indicators and identify areas for improvement.
Effects of Different Contract Models on Patient Outcomes
Different contract models employed by Medi-Cal can lead to varying patient outcomes. For instance, capitated contracts, where MCOs receive a fixed payment per member per month, can incentivize cost-saving measures that might affect the intensity or comprehensiveness of services provided. Conversely, fee-for-service contracts, while potentially leading to higher costs, can allow for greater provider autonomy and potentially more personalized care.
The choice of contract model should carefully consider the potential trade-offs between cost containment and quality of care. Research comparing patient outcomes under different contract models is crucial to inform future contracting strategies. Analysis of data on hospital readmission rates, emergency department visits, and patient satisfaction scores could provide valuable insights.
Hypothetical Scenario Illustrating Contract Provision Impact
Imagine a scenario where a Medi-Cal contract includes a provision limiting access to specialized mental health services unless a patient has first received a referral from their primary care physician. This provision, intended to manage costs and improve care coordination, could negatively impact patients experiencing acute mental health crises. A patient experiencing a severe anxiety attack might face significant delays in accessing necessary care while waiting for a referral, potentially leading to a worsening of their condition and increased risk of hospitalization.
This illustrates how even well-intentioned contract provisions can have unintended consequences if not carefully considered in relation to patient needs and access to timely care. Such a provision necessitates robust systems for expedited referrals and access to crisis intervention services to mitigate its potential negative impact.
Future Trends in Medi-Cal Contracting
California’s Medi-Cal system is constantly evolving, driven by technological advancements, shifting demographics, and evolving healthcare policy. Understanding the future trends in Medi-Cal managed care contracting is crucial for both the state and the providers participating in the system. This section will explore key emerging trends, potential challenges, and opportunities that lie ahead.
The future of Medi-Cal contracting will be shaped by a complex interplay of factors, demanding adaptability and strategic planning from all stakeholders. Increased focus on value-based care, technological integration, and data-driven decision-making will significantly influence the landscape of Medi-Cal contracts.
Value-Based Care Models
The shift towards value-based care (VBC) is a major trend impacting Medi-Cal contracting. VBC models incentivize providers to focus on improving patient outcomes and reducing healthcare costs, moving away from the traditional fee-for-service model. This transition requires innovative contract designs that reward quality, efficiency, and patient satisfaction, rather than simply the volume of services provided. For example, contracts may incorporate metrics such as patient-reported outcome measures (PROMs), readmission rates, and adherence to clinical guidelines.
Successful implementation will require robust data collection and analysis systems to track performance and ensure accountability.
Technological Integration and Data Analytics
Technology is playing an increasingly important role in Medi-Cal contracting. The use of telehealth, electronic health records (EHRs), and data analytics is transforming how care is delivered and managed. Contracts are likely to incorporate requirements for providers to utilize these technologies, ensuring interoperability and data sharing to improve care coordination and reduce administrative burden. For example, contracts could incentivize the adoption of telehealth platforms to expand access to care in rural areas or for patients with mobility limitations.
Furthermore, the use of predictive analytics can help identify patients at high risk of hospitalization or other adverse events, allowing for proactive interventions and improved outcomes.
Impact of Policy Changes
Changes in federal and state healthcare policy will significantly impact Medi-Cal contracting. For instance, future legislation might introduce new requirements for provider participation, quality metrics, or payment models. The expansion or contraction of eligibility criteria could also alter the demand for services and necessitate adjustments to contract terms. The implementation of new federal regulations concerning data privacy and security will also need to be incorporated into contracts to ensure compliance.
For example, the California legislature might introduce legislation mandating specific telehealth reimbursement rates or requiring the use of specific EHR systems.
Potential Future Changes to the Medi-Cal Contracting System
Several potential future changes are on the horizon for the Medi-Cal contracting system. These changes will likely require significant adaptation from both the state and participating providers.
- Increased emphasis on population health management contracts, focusing on preventative care and holistic patient well-being.
- Greater use of risk-sharing models where providers share in both the financial gains and losses associated with patient outcomes.
- Enhanced transparency and public reporting of provider performance data to improve accountability and consumer choice.
- More stringent requirements for data security and privacy in accordance with evolving regulations.
- Expansion of telehealth services and integration of remote patient monitoring technologies into contracts.
- Development of more sophisticated contract designs that incorporate incentives for improved health equity and address social determinants of health.
Epilogue
Navigating the world of California MediCal Medicaid contracts requires a keen understanding of the various players, processes, and financial implications. While the system is undeniably complex, its impact on healthcare access and quality is undeniable. This post has provided a foundational overview, but further research and engagement with relevant stakeholders are essential for a complete understanding. Hopefully, this overview has shed light on the critical role these contracts play in shaping healthcare in California and sparked your interest in learning more.
FAQ Corner
What happens if a Medi-Cal managed care plan fails to meet its contractual obligations?
The state has mechanisms for monitoring compliance and enforcing contract terms. Failure to meet obligations can result in penalties, including financial sanctions and potential contract termination.
How can I find out which managed care plans operate in my area?
The California Department of Health Care Services (DHCS) website provides a directory of Medi-Cal managed care plans and their service areas.
What types of services are covered under Medi-Cal?
Medi-Cal covers a wide range of medical services, including doctor visits, hospital care, prescription drugs, mental health services, and more. Specific coverage can vary depending on the plan and individual eligibility.
How does Medi-Cal determine eligibility?
Eligibility is based on factors like income, resources, age, disability status, and family size. The DHCS website provides detailed information on eligibility requirements.