California Sues Drugmakers, PBMs Over Insulin Costs
California sues drugmakers PBMs insulin costs – that’s a headline that’s grabbing attention, and rightfully so! The soaring price of insulin has become a crisis for millions of Americans, forcing many to ration their life-saving medication or forgo it altogether. This lawsuit, filed by California against major drug manufacturers and Pharmacy Benefit Managers (PBMs), aims to tackle the complex web of factors driving up insulin costs.
We’ll delve into the specifics of the lawsuit, explore the roles of different players in the pharmaceutical industry, and examine the devastating consequences of unaffordable insulin. Get ready for a deep dive into this critical issue.
The lawsuit alleges that drugmakers and PBMs are colluding to inflate insulin prices, exploiting a system designed to protect patients. This isn’t just about profits; it’s about lives. The impact on individuals struggling to afford this essential medicine is heartbreaking, and the broader implications for the healthcare system are alarming. We’ll explore the potential solutions and policy changes that could make insulin accessible and affordable for everyone who needs it.
The Lawsuit

Source: upriseri.com
California’s lawsuit against insulin manufacturers and Pharmacy Benefit Managers (PBMs) represents a significant legal challenge to the complex pricing structure of this life-saving medication. The state alleges a coordinated scheme to inflate insulin prices, leaving many Californians struggling to afford their necessary medication. This blog post will delve into the details of the lawsuit, examining the allegations, legal basis, and timeline of events.
Allegations in California’s Lawsuit
The lawsuit alleges that insulin manufacturers and PBMs engaged in anti-competitive practices that artificially inflated insulin prices. Specifically, California claims that manufacturers engaged in price-fixing and other anti-competitive behavior to maintain high prices. The lawsuit further alleges that PBMs, who negotiate drug prices on behalf of insurers and employers, engaged in practices that prevented competition and suppressed price reductions.
These practices, according to the lawsuit, resulted in exorbitant insulin costs for consumers, disproportionately affecting vulnerable populations. The state argues that this constitutes unfair competition and violates various consumer protection laws.
Legal Basis for the Lawsuit
California’s lawsuit relies on several legal grounds, including state antitrust laws and consumer protection statutes. The state is likely to cite California’s Cartwright Act, which prohibits unfair competition and price-fixing, and the Unfair Competition Law (UCL), which protects consumers from unlawful business practices. The lawsuit may also draw on precedents established in similar antitrust cases involving pharmaceutical pricing.
Successful prosecution will hinge on demonstrating a concerted effort between manufacturers and PBMs to manipulate the market and inflate prices, rather than simply individual companies acting in their own self-interest.
Timeline of Events Leading to the Lawsuit
While a precise timeline requires detailed legal documentation, a general overview can be constructed. Years of escalating insulin prices, coupled with growing public outcry and media attention, likely played a significant role in the state’s decision to pursue legal action. Investigations into insulin pricing practices by various regulatory bodies and legislative inquiries may have provided the state with evidence to support its claims.
The lawsuit itself represents the culmination of this process, with the state aiming to hold accountable those it believes responsible for the affordability crisis surrounding insulin.
Comparison of Roles in Insulin Pricing
| Factor | Drug Manufacturers | Pharmacy Benefit Managers (PBMs) | Impact on Insulin Pricing |
|---|---|---|---|
| Pricing Strategy | Set initial list prices, often high; may offer rebates and discounts to PBMs. | Negotiate rebates and discounts with manufacturers; set reimbursement rates for pharmacies. | Both influence final price paid by consumers, though manufacturers set the initial price. |
| Market Influence | Control supply and initial pricing of insulin products. | Control access to insulin through formularies and reimbursement rates; influence demand through their negotiating power. | Combined influence creates a complex system where competition is limited, leading to higher prices. |
| Transparency | Limited transparency regarding pricing strategies and rebate negotiations. | Limited transparency regarding rebate negotiations and formulary decisions. | Lack of transparency makes it difficult to assess the fairness and competitiveness of the insulin market. |
| Legal Liability | Potentially liable for anti-competitive practices, price-fixing, and violations of consumer protection laws. | Potentially liable for anti-competitive practices, steering patients to more expensive drugs, and violations of consumer protection laws. | The lawsuit aims to establish legal responsibility for the inflated prices. |
Insulin Pricing and Affordability
The cost of insulin in the United States has become a major crisis, impacting the lives and financial stability of millions of Americans with diabetes. This isn’t simply a matter of fluctuating drug prices; it’s a systemic issue with profound consequences for patients and the healthcare system as a whole. The exorbitant cost of this life-saving medication is forcing many to ration their insulin, leading to severe health complications and even death.The current state of insulin pricing in the US is characterized by dramatic price increases far outpacing inflation.
For decades, insulin has been available as a relatively affordable medication, but in recent years, the cost has skyrocketed, leaving many patients struggling to afford their prescriptions. This dramatic increase hasn’t been matched by corresponding improvements in the drug’s efficacy or safety. Instead, it’s driven by a complex interplay of market forces and industry practices.
Insulin Cost Increases Over Time
Numerous studies and reports document the alarming rise in insulin prices. For example, a 2023 report from the Health Care Cost Institute showed that the average price of insulin nearly tripled between 2002 and 2013. While the exact figures vary depending on the type of insulin and the specific payer, the trend is consistently upward. This price escalation has far outstripped the rate of inflation, creating a significant financial burden for individuals and families.
California’s lawsuit against drugmakers and PBMs over exorbitant insulin costs highlights a critical healthcare access issue. This fight for affordability is even more relevant when you consider how technology can impact healthcare efficiency; for example, check out how nuance integrates generative AI scribe into Epic EHRs , potentially streamlining processes and freeing up time for patient care. Ultimately, both this tech advancement and the California lawsuit aim to improve the healthcare experience, though through different approaches.
Imagine a scenario where the cost of a loaf of bread tripled in a decade – that’s the reality many insulin-dependent individuals face. This unsustainable trend is directly correlated to increased rates of rationing and diabetes-related complications.
Comparison of Insulin Costs Internationally
A stark contrast emerges when comparing insulin prices in the US with those in other developed countries. In Canada, the United Kingdom, and many European nations, insulin is significantly more affordable, often available at a fraction of the cost seen in the US. This difference isn’t due to superior manufacturing processes or differences in the drug itself; rather, it reflects differences in drug pricing policies and regulatory frameworks.
These countries often employ government price controls, negotiations with pharmaceutical companies, and other mechanisms to keep drug costs down, ensuring accessibility for their citizens. This international comparison underscores the inherent affordability issues within the US healthcare system regarding insulin specifically.
Factors Contributing to High Insulin Prices
The high cost of insulin in the US is a multifaceted problem with several contributing factors.
The following factors contribute significantly to the high cost of insulin:
- Manufacturer Pricing Strategies: Pharmaceutical companies have employed various strategies to maximize profits, including significant price increases with minimal changes to the product. This prioritization of profit over patient access has driven the affordability crisis.
- Lack of Competition: The insulin market is dominated by a small number of large manufacturers, limiting competition and preventing price pressure. This oligopolistic market structure allows for higher prices to be sustained.
- Complex Pharmacy Benefit Manager (PBM) Practices: PBMs, who manage prescription drug benefits for insurance companies, play a significant role in determining the price patients ultimately pay. Their complex rebate and pricing structures can obscure the true cost of insulin and often lead to higher out-of-pocket expenses for consumers.
- Absence of Strong Government Regulation: The US government has historically had limited direct control over insulin pricing, unlike many other developed nations. The lack of strong regulatory oversight has allowed prices to escalate unchecked.
The Role of Pharmacy Benefit Managers (PBMs)
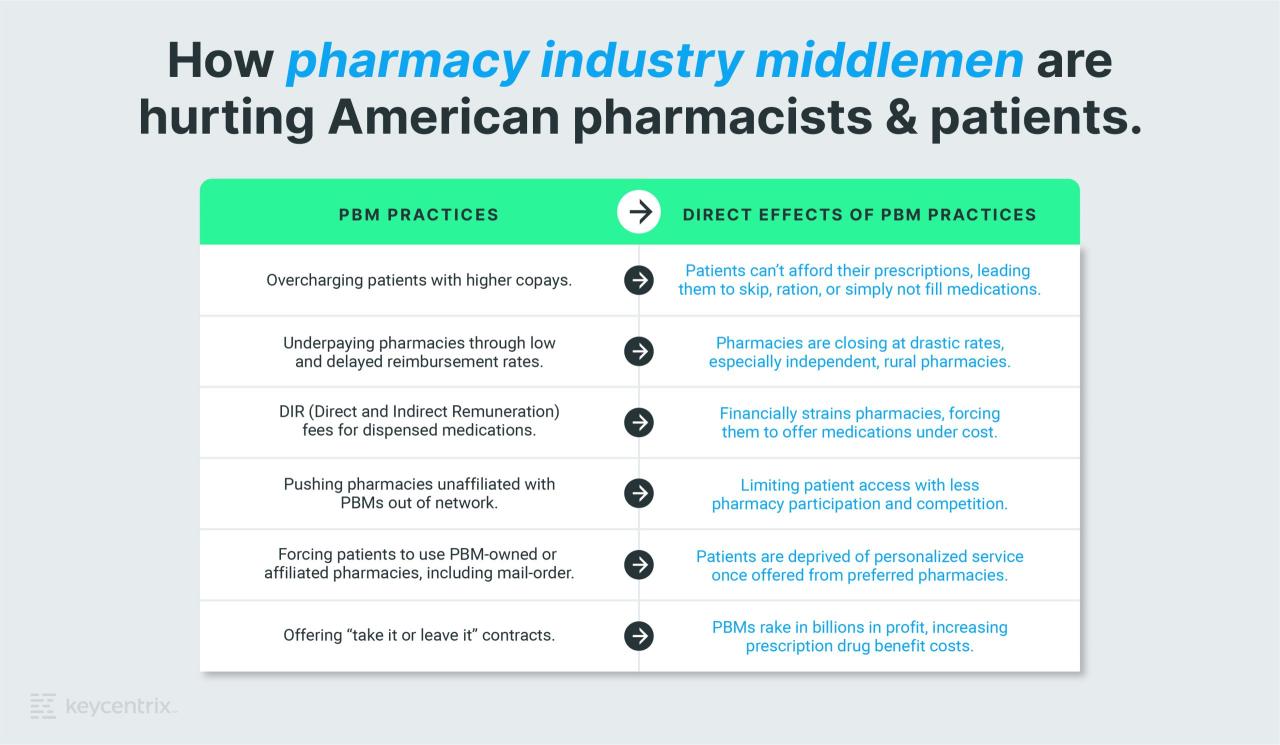
Pharmacy Benefit Managers (PBMs) are powerful intermediaries in the pharmaceutical supply chain, acting as negotiators between drug manufacturers, insurance companies, and pharmacies. Their influence on drug pricing, particularly for insulin, is significant and often a subject of intense scrutiny. Understanding their functions and potential conflicts of interest is crucial to addressing the affordability crisis surrounding insulin.PBMs perform several key functions.
They manage prescription drug benefits for health insurance plans, negotiating rebates and discounts with drug manufacturers. They also create and maintain formularies (lists of covered drugs), develop and implement utilization management programs (to control drug use and costs), and process claims for prescription drugs. Essentially, they act as the gatekeepers determining which drugs are covered, at what price, and under what conditions.
PBM Conflicts of Interest and Insulin Pricing
PBMs operate in a complex environment rife with potential conflicts of interest. One key concern is the “spread pricing” model, where PBMs negotiate a low price with manufacturers but charge pharmacies a significantly higher price, pocketing the difference. This practice, while potentially benefiting the PBM’s bottom line, directly contributes to higher costs for consumers and insurers. Another potential conflict arises from PBMs owning or operating pharmacies, creating an incentive to steer patients towards their own pharmacies, potentially at the expense of independent pharmacies offering lower prices.
In the case of insulin, this translates to patients facing higher out-of-pocket expenses even with insurance coverage. The lack of transparency in PBM negotiations further exacerbates this issue, making it difficult to determine the true cost of insulin and the extent of PBM profit margins.
PBM Practices and Higher Insulin Costs
Several PBM practices can contribute to higher insulin costs. The aforementioned spread pricing is a major factor. Additionally, the use of rebates and discounts negotiated with manufacturers often doesn’t translate into lower costs for consumers. Instead, these rebates can be kept by the PBM, or used to offset other costs, leaving patients to pay high co-pays and deductibles.
The design of formularies can also influence insulin prices. PBMs may favor more expensive insulin analogs over older, less expensive insulins, even if the clinical difference is minimal. This can drive up overall costs for patients and the healthcare system. Finally, restrictive prior authorization requirements for certain insulin products can create significant delays and hurdles for patients needing access to their medication, forcing them to either delay treatment or pay higher costs for an alternative.
Types of PBM Contracts and Their Impact on Insulin Prices, California sues drugmakers PBMS insulin costs
The impact of PBM contracts on insulin prices varies depending on the specific contract type. Different models exist, each with its own potential to influence cost.
| Contract Type | Description | Impact on Insulin Prices | Example |
|---|---|---|---|
| Traditional Fee-for-Service | PBMs charge a fee per claim processed. | Can lead to higher costs if PBMs prioritize processing volume over cost savings. | A PBM charges $2 per claim, regardless of the drug’s cost. |
| Performance-Based Contracts | PBMs are incentivized to reduce drug costs. | Potentially lower costs, but success depends on the specific metrics used. | A PBM receives a bonus for achieving a certain percentage reduction in insulin spending. |
| Risk-Sharing Contracts | PBMs share in the financial risk of managing drug costs. | Strong incentive to reduce costs, but can be complex to negotiate. | A PBM shares a portion of any cost overruns associated with insulin. |
| Bundled Payments | Payment for a range of services related to a specific condition (e.g., diabetes). | Can potentially incentivize cost savings across the entire care pathway. | A single payment covers all insulin, supplies, and related medical services for a diabetic patient. |
Impact on Patients and Healthcare System
Source: keycentrix.com
The exorbitant cost of insulin has created a devastating ripple effect, impacting not only individual patients but the entire healthcare system. For millions of Americans living with diabetes, the daily necessity of insulin has become a constant source of stress and financial hardship, forcing difficult choices between medication and other essential needs. This crisis highlights a critical failure in our healthcare system’s ability to ensure access to life-saving medication.High insulin prices disproportionately affect vulnerable populations.
The burden is particularly acute for low-income individuals and families, who may be forced to ration their insulin, leading to serious health consequences. This financial strain can extend beyond the individual, impacting family budgets and potentially leading to instability and hardship for entire households. The inability to afford insulin can lead to delayed or forgone medical care, resulting in preventable hospitalizations and worsening health outcomes, placing a greater strain on the healthcare system as a whole.
Financial Burden on Individuals and Families
The cost of insulin varies widely depending on the type and brand, but even generic insulins can be prohibitively expensive for many. Families struggling to afford insulin often face impossible choices: paying for insulin versus paying rent, buying groceries, or covering other essential expenses. Many individuals report skipping doses or using less insulin than prescribed to stretch their supply, a dangerous practice that can lead to serious complications, including diabetic ketoacidosis (DKA), a life-threatening condition.
Stories abound of individuals selling possessions, taking on debt, or even resorting to crowdfunding campaigns just to afford their insulin. The constant worry and stress associated with managing these financial burdens have significant negative impacts on mental and emotional well-being.
Impact on Healthcare System Resources
The high cost of insulin contributes significantly to escalating healthcare costs. When individuals are unable to afford their insulin, they often end up in emergency rooms or hospitals due to complications from uncontrolled diabetes. These emergency room visits and hospitalizations are far more expensive than the cost of the insulin itself, placing a significant burden on the healthcare system.
Furthermore, the long-term health consequences of uncontrolled diabetes, such as kidney failure, heart disease, and blindness, lead to even greater healthcare expenditures. The financial strain on the healthcare system ultimately impacts all stakeholders, including taxpayers and insurance providers.
Visual Representation of Impact on Patient Health Outcomes
Imagine a graph with “Insulin Affordability” on the x-axis, ranging from “Unaffordable” to “Affordable,” and “Health Outcomes” on the y-axis, ranging from “Poor” to “Excellent.” A line graph would show a clear upward trend: as insulin affordability increases, health outcomes improve. At the “Unaffordable” end of the x-axis, the line would be low on the y-axis, representing poor health outcomes, including complications like DKA, amputations, blindness, and heart disease.
As the line moves towards “Affordable,” it steadily rises, indicating improved health outcomes, such as better blood sugar control, fewer complications, and improved quality of life. This visualization powerfully illustrates the direct link between insulin affordability and patient well-being.
Potential Solutions and Policy Implications
California’s lawsuit against insulin manufacturers and PBMs shines a much-needed spotlight on the exorbitant cost of this life-saving medication. The implications extend far beyond the state’s borders, raising crucial questions about the future of drug pricing and access to essential medicines. Addressing this crisis requires a multifaceted approach, encompassing both immediate solutions and long-term policy changes.The high cost of insulin stems from a complex interplay of factors, including patent protection, manufacturing costs, and the influence of Pharmacy Benefit Managers (PBMs).
Simply suing the players involved, while a necessary step to expose wrongdoing, isn’t a sufficient solution. A comprehensive strategy is needed to ensure affordable and accessible insulin for all who need it.
Government Price Negotiation
The federal government’s ability to negotiate drug prices directly with pharmaceutical companies is a key area for potential reform. Currently, Medicare is largely prohibited from negotiating prices, a restriction that has significantly contributed to the high cost of many drugs, including insulin. Allowing Medicare to negotiate could significantly reduce insulin prices, making it more affordable for seniors and other vulnerable populations.
This approach has been successfully implemented in other countries, resulting in lower drug costs for their citizens. For example, Canada’s national pharmacare program utilizes bulk purchasing and negotiation to achieve lower prices. A similar model in the United States could leverage the government’s purchasing power to secure better deals for insulin.
Increased Transparency and Regulation of PBMs
Pharmacy Benefit Managers (PBMs) play a significant role in determining drug prices and reimbursement rates. Their opaque practices and potential conflicts of interest often result in higher costs for patients. Increased transparency in PBM operations, including the disclosure of their rebate and spread pricing models, is essential. Stricter regulations on their practices, including limitations on rebates and spread pricing, could also help lower insulin costs.
For instance, requiring PBMs to pass on savings to consumers directly, rather than keeping a portion for profit, could dramatically improve affordability.
Incentivizing Generic and Biosimilar Insulin Production
The market dominance of a few insulin manufacturers has limited competition and driven up prices. Policies that incentivize the development and production of generic and biosimilar insulins are crucial. This could include streamlining the approval process for biosimilars, reducing regulatory hurdles, and providing financial incentives to manufacturers. The faster generic and biosimilar insulins become available, the more competition will be introduced, and the lower the prices will fall.
Examples of successful biosimilar programs in other therapeutic areas show that such strategies can significantly reduce drug costs.
California’s lawsuit against drugmakers and PBMs over exorbitant insulin costs highlights a critical healthcare access issue. Understanding the complexities of pricing requires looking at innovative solutions, like those explored in a recent study widespread digital twins healthcare , which could potentially improve efficiency and transparency. Ultimately, the lawsuit’s success could significantly impact how insulin is priced and accessed, hopefully leading to fairer costs for patients.
Expanding Access to Affordable Insurance
Ensuring access to affordable health insurance is crucial for making insulin accessible. Expanding Medicaid eligibility, strengthening the Affordable Care Act, and addressing the uninsured population will help more people afford their insulin. This will not only improve individual health outcomes but also reduce the burden on the healthcare system. Studies have shown that increased insurance coverage is associated with improved access to medication and better health outcomes.
Policies that expand coverage are therefore essential components of a comprehensive strategy.
Public Health Perspective: California Sues Drugmakers PBMS Insulin Costs
The escalating cost of insulin presents a significant and growing public health crisis, impacting not only individual well-being but also straining healthcare systems and exacerbating existing health disparities. Inadequate access to this life-saving medication leads to preventable complications, hospitalizations, and even deaths, placing a considerable burden on individuals, families, and society as a whole.High insulin costs disproportionately affect vulnerable populations, creating a serious public health concern.
The financial burden of insulin forces many individuals, particularly those with lower incomes or limited insurance coverage, to ration their medication, leading to dangerous health consequences. This rationing can result in severe hyperglycemia, causing long-term damage to vital organs like the kidneys, eyes, and nerves, ultimately leading to increased healthcare utilization and decreased quality of life. The impact is particularly pronounced among marginalized communities who already face systemic barriers to healthcare access.
Health Disparities and Insulin Access
The high cost of insulin significantly contributes to existing health disparities. Individuals living in poverty, those belonging to racial and ethnic minority groups, and those lacking adequate health insurance are disproportionately affected. These populations often face multiple challenges, including limited access to healthcare, lower health literacy, and higher rates of chronic conditions like diabetes. The financial burden of insulin exacerbates these existing inequalities, creating a cycle of poor health outcomes and limited opportunities.
For example, a study might show that individuals in low-income zip codes experience significantly higher rates of diabetes-related complications due to insulin rationing compared to those in higher-income areas. This highlights the unequal impact of high insulin prices on different segments of the population.
California’s lawsuit against drugmakers and PBMs over exorbitant insulin costs highlights a broader healthcare affordability crisis. This isn’t just about insulin; it impacts access to vital care across the board, even impacting services like those offered at rural hospitals, as highlighted in this insightful article on Rural Hospitals Labor Delivery & which shows how strained resources affect essential services.
Ultimately, the fight for affordable insulin is intertwined with the larger struggle for accessible healthcare for all.
Initiatives to Improve Insulin Access and Affordability
Several initiatives are underway to address the insulin affordability crisis. Many states have implemented programs to provide insulin at lower costs to low-income individuals. These programs often involve negotiating with manufacturers or establishing state-funded assistance programs. Additionally, some pharmaceutical companies have introduced patient assistance programs, providing discounted or free insulin to eligible patients. However, these programs often have complex eligibility requirements and are not always sufficient to meet the needs of all patients struggling with insulin affordability.
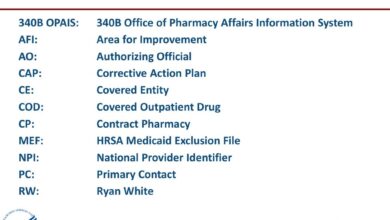
For example, the 340B drug pricing program, designed to reduce drug costs for safety-net hospitals, is one such initiative aiming to improve access for vulnerable patients. However, the effectiveness of these programs is often hampered by limitations in funding, stringent eligibility criteria, and the complexity of navigating the application processes.
Strategies for Improving Public Health Outcomes Related to Insulin Access
Addressing the public health consequences of high insulin costs requires a multi-pronged approach. The following strategies are crucial:
- Implement price controls or negotiations to lower the cost of insulin.
- Expand access to affordable insurance coverage, including Medicaid and the Affordable Care Act.
- Increase funding for state and federal programs that provide assistance with insulin costs.
- Improve health literacy and patient education on diabetes management and insulin use.
- Promote the development and use of biosimilar insulins, which are generally less expensive than brand-name insulins.
- Strengthen oversight of Pharmacy Benefit Managers (PBMs) to ensure transparency and fair pricing practices.
- Invest in research to develop more affordable and effective insulin therapies.
Ultimate Conclusion
California’s lawsuit against drugmakers and PBMs over insulin costs is a significant step in addressing a critical public health crisis. The high price of insulin is not just a financial burden; it’s a matter of life and death for millions. While the legal battle unfolds, the conversation around insulin affordability must continue. We need innovative solutions, regulatory changes, and a renewed commitment to ensuring that everyone has access to this life-saving medication.
The fight for affordable insulin is far from over, but this lawsuit represents a powerful push towards a more just and equitable healthcare system.
Top FAQs
What are Pharmacy Benefit Managers (PBMs)?
PBMs are third-party administrators of prescription drug benefits. They negotiate drug prices with manufacturers, manage formularies, and process claims for insurance companies and employers.
How does this lawsuit differ from previous attempts to lower insulin costs?
This lawsuit directly targets both drug manufacturers and PBMs, alleging collusion to keep prices high. Previous efforts have often focused on one or the other, or on broader drug pricing reform.
What are the potential outcomes of this lawsuit?
Potential outcomes range from financial penalties for the defendants to changes in industry practices and regulations aimed at lowering insulin costs. The legal process is lengthy and the final outcome is uncertain.
Are there other states considering similar lawsuits?
Yes, several other states are considering or have already filed similar lawsuits, demonstrating a growing national concern about insulin affordability.