Change Healthcare Cyberattack Data Breach Reporting HHS OCR
Change Healthcare Cyberattack Data Breach Reporting Requirements HHS OCR: The healthcare industry faces a constant barrage of cyber threats, leading to increasingly frequent data breaches. This has spurred significant discussion around how we report these incidents, prompting a closer look at the regulations set by the HHS Office for Civil Rights (OCR). Understanding these rules—and the potential changes on the horizon—is crucial for healthcare providers to navigate the complex landscape of data security and compliance.
This post dives into the current HHS OCR data breach reporting requirements, exploring the notification timelines, affected entities, and types of breaches mandating reporting. We’ll also examine proposed changes, analyzing their potential impact on healthcare providers and comparing them to regulations in other sectors. Furthermore, we’ll explore the role of technology in improving data breach detection and response, highlighting best practices for prevention and incident response.
Finally, we’ll take a look at international comparisons, drawing lessons from global approaches to this critical issue.
Current HHS OCR Data Breach Reporting Requirements: Change Healthcare Cyberattack Data Breach Reporting Requirements Hhs Ocr
Navigating the complex world of HIPAA and data breach reporting can be daunting for healthcare providers. Understanding the specific requirements set forth by the HHS Office for Civil Rights (OCR) is crucial for maintaining compliance and mitigating potential risks. This post Artikels the key aspects of these regulations.
Data Breach Notification Timelines and Procedures
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule, enforced by the OCR, mandates that covered entities and business associates report breaches of unsecured protected health information (PHI). The timeline for notification is dependent on the nature and scope of the breach. If a breach affects a significant number of individuals, notification must be made to affected individuals without unreasonable delay and in no case later than 60 days following the discovery of the breach.
The OCR must also be notified of breaches affecting 500 or more individuals. For breaches affecting fewer than 500 individuals, notification to OCR is not mandated, though they may still be notified depending on the circumstances. The notification process typically involves a written or electronic notification to individuals, outlining the type of information breached, steps individuals can take to protect themselves, and contact information for assistance.
OCR notification typically involves submitting a breach report through their online portal, providing details of the breach investigation and remediation efforts.
Types of Breaches Requiring Mandatory Reporting
Mandatory reporting applies to breaches involving unsecured PHI. This includes, but is not limited to, unauthorized access, use, disclosure, acquisition, alteration, or destruction of electronic or paper PHI. Examples include hacking incidents, loss or theft of devices containing PHI, improper disposal of PHI, and insider threats. The determination of whether a breach is considered “unsecured” involves assessing whether the risk of harm is present.
This assessment takes into account the nature of the PHI, the sensitivity of the information, the likelihood of unauthorized access, and the potential consequences of such access.
Reporting Requirements for Different Covered Entities
HIPAA’s reporting requirements apply to covered entities, which include health plans, healthcare providers, and healthcare clearinghouses. Business associates, who perform functions or activities that involve the use or disclosure of PHI on behalf of a covered entity, also have reporting obligations. While the core requirements are consistent across these entities, the specific implementation might vary based on their individual organizational structures and the nature of their activities.
For example, a large hospital system will have a more complex reporting process than a small physician practice. The responsibility for reporting ultimately rests with the covered entity or business associate that experienced the breach.
Summary of Key Aspects of Current Reporting Regulations
| Aspect | Description |
|---|---|
| Covered Entities | Health plans, healthcare providers, healthcare clearinghouses, and their business associates. |
| Types of Breaches | Unauthorized access, use, disclosure, acquisition, alteration, or destruction of unsecured PHI. |
| Notification to Individuals | Required without unreasonable delay and no later than 60 days after discovery, if the breach affects more than a small number of individuals. |
| Notification to OCR | Required for breaches affecting 500 or more individuals. |
Proposed Changes to Reporting Requirements
The HHS Office for Civil Rights (OCR) periodically reviews and potentially updates its data breach notification rules under the HIPAA Privacy Rule. While specific proposals are subject to change and official publication in the Federal Register, general trends and potential areas of modification can be discussed based on ongoing discussions within the healthcare and regulatory communities. These potential changes aim to modernize the reporting process, improve transparency, and better protect patient data.The rationale behind proposed changes often centers on enhancing the effectiveness of the breach notification system.
Current regulations may not adequately capture the nuances of modern cyberattacks, particularly those involving sophisticated techniques like ransomware or AI-driven attacks. Furthermore, the evolving landscape of data storage and transfer necessitates adjustments to ensure consistent protection across various technologies. A more streamlined and efficient reporting process could also alleviate burdens on healthcare providers while simultaneously improving the overall response to breaches.
Rationale for Proposed Changes
Proposed changes often stem from a need to address limitations in the current system. For example, the current definition of a “breach” might be too narrow, failing to encompass certain types of data compromises that still pose significant risks to patient information. Another area of potential modification involves the timing and methods of notification. Faster reporting could enable quicker remediation efforts and potentially minimize the impact of a breach.
The goal is to create a more proactive and responsive system that aligns with the ever-increasing sophistication of cyber threats.
Potential Impact on Healthcare Providers
Proposed changes could significantly impact healthcare providers. For instance, broader definitions of a “breach” could lead to an increase in the number of incidents requiring notification. This might necessitate greater investment in cybersecurity infrastructure, incident response planning, and breach notification expertise. On the other hand, a streamlined reporting process could reduce administrative burdens. The overall impact will depend on the specific nature of the proposed changes and how effectively healthcare providers can adapt to them.
A successful implementation would require collaboration between regulatory bodies and healthcare organizations to ensure a smooth transition and minimize disruption.
Comparison with Other Sectors
The HIPAA breach notification rule is unique to the healthcare sector, but comparisons can be drawn with regulations in other industries. For example, the California Consumer Privacy Act (CCPA) and other state-level data breach notification laws often have broader definitions of a “breach” and may require notification even in cases where there is no evidence of actual harm. Similarly, the General Data Protection Regulation (GDPR) in Europe emphasizes data protection by design and default, requiring proactive measures to prevent breaches.
Comparing and contrasting these regulations can provide insights into best practices and potential areas for improvement in the HIPAA framework.
Key Differences from Current Regulations
The following list Artikels potential key differences between proposed and current HHS OCR data breach reporting requirements. It’s important to note that these are potential changes and may not reflect the final outcome of any proposed rulemaking.
- Expanded Definition of a Breach: The proposed changes might expand the definition of a “breach” to include incidents that may not currently trigger notification requirements, such as unauthorized access to data even without evidence of exfiltration.
- Shorter Reporting Timeframes: A reduction in the time healthcare providers have to report breaches to both OCR and affected individuals. This could be a significant change from the current timeframe.
- Enhanced Notification Requirements: More detailed information might be required in breach notifications to both OCR and affected individuals, such as a more thorough description of the incident and the steps taken to mitigate the harm.
- Increased Focus on Risk Assessment: Proposed changes might emphasize a more robust risk assessment process, requiring providers to analyze the potential impact of a breach before determining whether notification is required.
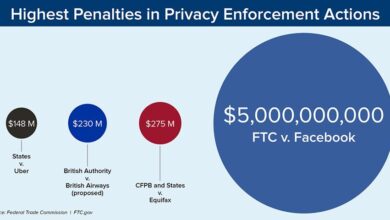
- Strengthened Enforcement: Increased penalties for non-compliance with breach notification requirements.
Impact of Cyberattacks on Healthcare Data Breach Reporting

Source: alamy.com
Cyberattacks significantly complicate healthcare data breach reporting, introducing delays, inaccuracies, and challenges in determining the true scope of compromised information. The increasing sophistication of these attacks, coupled with the sensitive nature of healthcare data, necessitates a deeper understanding of their impact on the reporting process. This section explores how cyberattacks affect timely and accurate reporting, examines past examples, and illustrates the complexities through a hypothetical scenario.Cyberattacks often make determining the full extent of a data breach extremely difficult.
The nature of many attacks, particularly ransomware or sophisticated intrusion attempts, involves stealthy data exfiltration that can go undetected for extended periods. This delay directly impacts the timeliness of breach reporting, potentially violating mandated reporting deadlines and leaving affected individuals vulnerable for longer than necessary. Furthermore, the complexity of many cyberattacks can hinder accurate assessment of the types and amounts of data compromised.
The new HHS OCR changes to healthcare cyberattack data breach reporting are definitely making things more complex for providers. I’ve been spending so much time on compliance lately that my wrists are killing me! I actually found some helpful information on ways to treat carpal tunnel syndrome without surgery which I’m planning to try. Hopefully, that will free up some time to focus more on the intricacies of these new reporting requirements.
Back to the grindstone!
Decryption of encrypted data, analysis of system logs, and forensic investigation can be extensive and time-consuming processes.
Examples of Cyberattacks Impacting Healthcare Data Breach Reporting
Several high-profile cyberattacks have demonstrably impacted healthcare data breach reporting. For instance, the 2017 NotPetya ransomware attack affected hospitals worldwide, causing significant disruption to operations and delaying patient care. The widespread nature of the attack made determining the precise scope of data breaches across different healthcare organizations extremely challenging, leading to fragmented and delayed reporting. Similarly, the 2020 attacks targeting the University of California San Francisco Health System highlighted the difficulties in quickly assessing the extent of data compromise when faced with advanced persistent threats.
The attackers employed techniques designed to evade detection, making the initial assessment and subsequent reporting significantly more complex and time-consuming. These examples underscore the inherent difficulties in swiftly and accurately reporting breaches resulting from complex cyberattacks.
Challenges Posed by Cyberattacks to Timely and Accurate Reporting
The challenges posed by cyberattacks to timely and accurate reporting are multifaceted. Firstly, the often-stealthy nature of sophisticated attacks makes early detection extremely difficult. Attackers frequently employ techniques to mask their presence and avoid triggering traditional security alerts. Secondly, even after detection, determining the precise scope of the breach can be incredibly complex. This involves meticulously analyzing system logs, identifying compromised data, and assessing the potential impact on affected individuals.
Thirdly, the remediation process following a cyberattack can be lengthy and resource-intensive. This includes restoring systems, patching vulnerabilities, and implementing enhanced security measures. This process itself can delay the reporting process, potentially exceeding mandated reporting timelines. Finally, the legal and regulatory complexities surrounding data breach reporting can further complicate matters, especially in cases involving international actors or intricate attack vectors.
The need to coordinate with law enforcement, regulatory bodies, and potentially legal counsel adds to the already considerable burden.
Hypothetical Scenario Illustrating Reporting Complexities
Imagine a large hospital system targeted by a sophisticated state-sponsored cyberattack. The attackers, using advanced malware and social engineering techniques, gain unauthorized access to the hospital’s network over several months. They exfiltrate protected health information (PHI) in small batches, cleverly avoiding detection by security systems. The breach only comes to light when an external security audit reveals unusual network activity.
Determining the precise timeframe of the attack, the exact amount of data compromised, and the identities of all affected individuals requires extensive forensic investigation and data analysis, taking several weeks or even months. This delay significantly complicates reporting to HHS OCR and potentially triggers additional regulatory scrutiny. The hospital’s subsequent efforts to notify affected individuals, remediate the vulnerabilities, and implement improved security measures will be equally challenging and time-consuming.
Impact of Cyberattack Nature on Breach Scope and Severity
The type of cyberattack directly influences the scope and severity of the reported breach. A ransomware attack, for example, might lead to a relatively localized breach, impacting specific systems or data sets. However, the disruption to hospital operations and the potential for data loss due to system downtime can still be significant. Conversely, a sophisticated, multi-stage attack, such as an advanced persistent threat (APT), could compromise a far broader range of data and systems over a much longer period.
This can result in a far more extensive and severe breach, requiring significantly more resources for remediation and reporting. The attackers’ motives also play a role. A financially motivated attack might focus on data exfiltration for ransom, while a state-sponsored attack might aim to steal intellectual property or disrupt operations. Understanding the attacker’s goals helps to determine the scope and potential long-term consequences of the breach.
The new HHS OCR changes to healthcare cyberattack data breach reporting requirements are significant, impacting how facilities handle sensitive patient information. This comes at a time when the legal landscape is shifting, as the Supreme Court’s decision to overturn the Chevron Doctrine, as detailed in this article scotus overturns chevron doctrine healthcare , could further reshape regulatory enforcement.
This means navigating these new reporting requirements will require even more careful attention to detail and legal counsel.
Best Practices for Data Breach Prevention and Response
Protecting patient data in the healthcare industry is paramount, given the sensitive nature of the information involved. A robust approach to cybersecurity, encompassing preventative measures and a well-defined incident response plan, is essential to minimize the risk and impact of data breaches. This section Artikels key best practices to help healthcare organizations strengthen their defenses.
Key Best Practices for Preventing Healthcare Data Breaches
Implementing a multi-layered approach to security is crucial for preventing data breaches. This involves a combination of technical, administrative, and physical safeguards. A strong security posture is built upon a foundation of proactive measures rather than reactive responses.
- Regular Security Awareness Training: Employees are often the weakest link in the security chain. Regular training on phishing scams, malware, and social engineering tactics helps equip staff to identify and avoid potential threats. This should include simulated phishing attacks to assess employee vulnerability and reinforce learning.
- Strong Access Control and Authentication: Implementing multi-factor authentication (MFA) for all users, especially those with access to sensitive data, significantly enhances security. Access should be granted based on the principle of least privilege, meaning users only have access to the data and systems necessary for their job functions. Regular access reviews should be conducted to ensure continued appropriateness.
- Data Encryption: Encrypting data both in transit and at rest protects it from unauthorized access even if a breach occurs. This applies to data stored on servers, laptops, mobile devices, and in the cloud.
- Regular Security Audits and Vulnerability Scanning: Proactive identification and remediation of vulnerabilities are essential. Regular security audits and vulnerability scans help identify weaknesses in systems and applications before they can be exploited by attackers.
- Robust Patch Management: Promptly patching software vulnerabilities is critical. Outdated software is a prime target for attackers. A centralized patch management system can streamline this process and ensure timely updates.
- Network Segmentation: Dividing the network into smaller, isolated segments limits the impact of a breach. If one segment is compromised, the attacker’s access to other parts of the network is restricted.
Importance of Robust Cybersecurity Measures
Robust cybersecurity measures are not simply a cost; they are an investment in protecting patient data, maintaining public trust, and avoiding the potentially devastating financial and reputational consequences of a data breach. The costs associated with a breach – including fines, legal fees, remediation efforts, and loss of business – far outweigh the cost of implementing strong security measures.
A strong cybersecurity program demonstrates a commitment to patient privacy and compliance with regulations like HIPAA.
Creating an Effective Incident Response Plan for Data Breaches
An effective incident response plan is crucial for minimizing the damage caused by a data breach. This plan should Artikel clear procedures for identifying, containing, eradicating, recovering from, and reporting a security incident.
- Preparation: Define roles and responsibilities, establish communication protocols, and identify key stakeholders.
- Identification: Establish methods for detecting a breach, including intrusion detection systems and security information and event management (SIEM) tools.
- Containment: Isolate affected systems to prevent further damage and data exfiltration.
- Eradication: Remove malware and restore systems to a secure state.
- Recovery: Restore data from backups and resume normal operations.
- Post-Incident Activity: Conduct a thorough investigation to determine the root cause of the breach, implement corrective actions to prevent future incidents, and review and update the incident response plan.
Data Breach Incident Response Flowchart
[Imagine a flowchart here. The flowchart would begin with “Suspected Breach Detected,” branching to “Incident Response Team Activated.” Subsequent steps would include “Assess the Breach,” “Contain the Breach,” “Eradicate the Threat,” “Recover Data,” “Notify Affected Parties,” and “Conduct Post-Incident Review.” Each step would lead to the next, with potential loops back for additional investigation or remediation if necessary.
The flowchart would visually represent the sequential steps of the incident response process.]
Effective Communication Strategies for Data Breaches
Effective communication is critical during and after a data breach. Transparency builds trust and minimizes negative consequences.
- Patient Notification: Provide timely and accurate information to affected patients, including the type of data compromised, the steps taken to mitigate the breach, and resources available to help protect them from identity theft.
- Regulatory Reporting: Comply with all applicable regulations, such as HIPAA’s breach notification rule, by promptly reporting the breach to the appropriate authorities.
- Internal Communication: Keep employees informed throughout the process to maintain morale and ensure everyone understands their roles and responsibilities.
- Public Relations: Develop a communication strategy to address public concerns and maintain a positive reputation.
The Role of Technology in Improving Data Breach Reporting
The healthcare industry faces a constant barrage of cyber threats, making robust and efficient data breach reporting crucial. Emerging technologies offer significant potential to improve the speed, accuracy, and overall effectiveness of this process, reducing the impact of breaches and strengthening patient data security. This involves not only faster detection but also a more streamlined reporting process that minimizes administrative burden and maximizes compliance.
Automation is key to streamlining the reporting process. Manual data breach reporting is time-consuming, prone to errors, and often delays crucial response actions. Automating tasks like data aggregation, analysis, and report generation can significantly reduce the time it takes to comply with HHS OCR regulations. This allows healthcare providers to focus their resources on remediation and patient notification, rather than paperwork.
Automated Data Breach Detection Systems, Change healthcare cyberattack data breach reporting requirements hhs ocr
Automated data breach detection systems leverage advanced analytics and machine learning algorithms to identify suspicious activities in real-time. These systems can monitor network traffic, user behavior, and database activity for anomalies indicative of a breach. For example, a system might flag unusual login attempts from unfamiliar geographic locations or detect unusual data access patterns. The system can then automatically trigger alerts, initiate incident response protocols, and even begin compiling data for the breach report.
This proactive approach drastically reduces the time between a breach and its reporting, limiting potential damage.
The new HHS OCR changes to healthcare cyberattack data breach reporting are significant, impacting how facilities handle sensitive patient information. This heightened focus on security is crucial, especially considering the advancements in medical technology; for example, the recent FDA approval of clinical trials for pig kidney transplants in humans, as reported on this site , highlights the need for robust data protection around these groundbreaking procedures.
Stronger security measures are vital to safeguarding this emerging field’s sensitive data from breaches.
AI-Powered Threat Intelligence Platforms
AI-powered threat intelligence platforms provide valuable insights into emerging threats and vulnerabilities. These platforms analyze vast amounts of data from various sources, including security feeds, dark web activity, and industry reports, to identify potential risks. By proactively identifying vulnerabilities and predicting potential attack vectors, healthcare providers can strengthen their security posture and reduce the likelihood of breaches. This proactive approach translates to fewer breaches to report and more efficient response when incidents do occur.
Blockchain Technology for Enhanced Data Security
Blockchain technology offers a secure and transparent way to manage and track sensitive patient data. Its decentralized and immutable nature makes it extremely difficult for unauthorized actors to access or alter data. By integrating blockchain into their data management systems, healthcare providers can enhance data security and reduce the risk of breaches. Furthermore, a blockchain-based system can automatically log and timestamp all data access events, providing an auditable trail that simplifies the breach reporting process.
While still emerging in widespread healthcare adoption, the potential for improved security and reporting is significant.
Comparison of Data Breach Detection and Response Technologies
Several technologies are used for data breach detection and response, each with its strengths and weaknesses. Traditional signature-based intrusion detection systems (IDS) rely on known attack patterns, making them less effective against zero-day exploits. However, they are relatively inexpensive and easy to implement. In contrast, anomaly-based IDS can detect unknown attacks by identifying deviations from normal system behavior, but they are more complex to manage and can generate false positives.
Advanced technologies like machine learning and AI-powered systems offer a more comprehensive approach, combining the strengths of both signature-based and anomaly-based detection methods. The choice of technology depends on factors such as budget, technical expertise, and the specific security needs of the healthcare organization.
Hypothetical System for Improved Breach Reporting
A hypothetical system for improved breach reporting could incorporate several of these technologies. This system would include:
- An AI-powered threat intelligence platform to proactively identify and mitigate potential vulnerabilities.
- An automated data breach detection system using machine learning to identify suspicious activities in real-time.
- A blockchain-based data management system to enhance data security and provide an auditable trail.
- An automated reporting module that integrates with the detection system and compiles the necessary information for the HHS OCR breach report.
This integrated system would provide a comprehensive and efficient solution for data breach detection, response, and reporting, significantly reducing the time and effort required to comply with regulatory requirements while enhancing overall data security. Such a system could potentially leverage existing EHR systems for seamless integration and data flow.
International Comparisons of Data Breach Reporting

Source: epiconferences.com
The United States’ approach to healthcare data breach reporting, while robust in its notification requirements, isn’t universally adopted. A global perspective reveals significant variations in regulations, enforcement, and the overall effectiveness of data breach response mechanisms across different nations. Comparing these differences illuminates both strengths and weaknesses in the current US system and highlights potential areas for improvement.
Several key differences exist between the US approach and those of other developed nations. The US system, primarily governed by HIPAA, focuses on notification thresholds and timelines, placing a significant emphasis on individual patient notification. Other countries, however, may prioritize different aspects, such as data security standards or the involvement of data protection authorities in investigations. This leads to varied approaches in data breach handling and potentially different outcomes for affected individuals.
Data Breach Notification Thresholds and Timelines
The US HIPAA Breach Notification Rule mandates notification within 60 days of discovering a breach affecting 500 or more individuals. Many other countries have similar notification requirements, though the thresholds and timelines can differ considerably. For example, the EU’s General Data Protection Regulation (GDPR) doesn’t specify a numerical threshold but requires notification “without undue delay,” placing the onus on organizations to assess the risk and notify affected individuals promptly.
Some nations may have more lenient or stricter thresholds and deadlines, impacting the speed and scale of response to breaches.
Roles of Data Protection Authorities
The US system relies heavily on self-reporting by covered entities, with OCR (Office for Civil Rights) acting as the primary oversight body. In contrast, many European nations have established independent data protection authorities with significant investigative powers. These authorities actively monitor compliance, conduct investigations into breaches, and can impose substantial penalties for non-compliance. This proactive approach, while potentially more resource-intensive, can lead to more effective breach prevention and response.
The UK’s Information Commissioner’s Office (ICO) and the French Commission Nationale de l’Informatique et des Libertés (CNIL) are examples of such powerful regulatory bodies.
Best Practices from Other Nations
Several international best practices could be beneficial to the US system. The GDPR’s emphasis on data protection by design and default, requiring organizations to embed security measures from the outset, is one example. Another is the proactive approach taken by some countries in promoting data breach incident response plans and conducting regular security audits. The focus on data minimization and purpose limitation, also emphasized by the GDPR, could significantly reduce the potential impact of breaches.
Challenges of Harmonizing Data Breach Reporting Requirements
Harmonizing data breach reporting requirements across international borders presents several significant challenges. Differing legal systems, data protection philosophies, and levels of technological development all contribute to this complexity. Furthermore, achieving consensus on a universally applicable definition of a “data breach” and establishing consistent notification thresholds and timelines would be a monumental task. The issue of data sovereignty, which emphasizes a nation’s right to regulate data within its borders, also presents a significant hurdle.
Successful International Collaborations in Addressing Data Breaches
While complete harmonization remains elusive, several successful international collaborations illustrate the potential for cooperation. Sharing best practices through international organizations, such as the OECD, and fostering cross-border information sharing amongst data protection authorities are important steps. Joint investigations into transnational breaches and the development of common standards for data security and incident response are further examples of successful collaborations.
These collaborative efforts can improve global response to data breaches and enhance the overall security posture of healthcare systems worldwide.
Comparison of Data Breach Reporting Regulations
| Country | Notification Threshold | Notification Timeline | Regulatory Body |
|---|---|---|---|
| United States | 500 or more individuals | 60 days | HHS OCR |
| United Kingdom | Significant risk to individuals | Without undue delay | ICO |
| European Union (GDPR) | Significant risk to individuals | Without undue delay | National Data Protection Authorities |
| Canada | Varies by province/territory | Varies | Provincial/Territorial authorities |
End of Discussion
Navigating the complexities of healthcare data breach reporting is a constant challenge. The evolving threat landscape, coupled with increasingly stringent regulations, demands proactive measures from healthcare providers. By understanding the current HHS OCR requirements, anticipating future changes, and implementing robust cybersecurity strategies, healthcare organizations can better protect patient data and minimize the impact of breaches. Staying informed and adapting to these changes is not just a matter of compliance; it’s a crucial step in safeguarding patient trust and upholding the integrity of the healthcare system.
Query Resolution
What happens if I don’t report a data breach to HHS OCR?
Failure to report a breach as required can result in significant civil monetary penalties.
What types of data are considered protected health information (PHI) under HIPAA?
PHI includes individually identifiable health information, such as names, addresses, medical records, and insurance information.
How long do I have to report a breach to affected individuals?
The timeframe for notifying individuals varies depending on the circumstances of the breach and state laws, but HHS OCR provides guidance.
Are there resources available to help healthcare providers improve their cybersecurity?
Yes, numerous organizations offer resources, training, and tools to enhance cybersecurity posture. HHS OCR also provides guidance and support.