Healthcare Systems Make Valuable Strides in a Pandemic
Healthcare systems make valuable strides in the eye of a pandemic – a statement that feels both profoundly true and incredibly understated. The past few years have witnessed a seismic shift in how we approach healthcare, driven by the urgent need to combat a global crisis. From the rapid adoption of telehealth to the development of groundbreaking diagnostic tools and treatments, the pandemic forced innovation at an unprecedented scale.
This journey wasn’t without its challenges, of course – overburdened healthcare workers, resource shortages, and stark inequalities in access to care remain pressing concerns. But exploring the advancements, the adaptations, and the lessons learned offers a powerful narrative of resilience, ingenuity, and the enduring commitment to human health.
This post delves into the remarkable transformations within healthcare systems, examining the innovative solutions implemented, the crucial role of technology, and the lasting impact on both healthcare professionals and patients. We’ll also explore the critical issues of equity and access, ensuring no one is left behind in the quest for better healthcare.
Pandemic-Driven Innovations in Healthcare Delivery
The COVID-19 pandemic presented unprecedented challenges to healthcare systems globally, forcing rapid adaptation and innovation. The crisis acted as a catalyst, accelerating the adoption of technologies and strategies that had previously been slow to integrate into mainstream healthcare. These changes, while born from necessity, have fundamentally reshaped how healthcare is delivered, potentially improving access and efficiency in the long term.
Telehealth Expansion and Impact on Patient Access
The pandemic dramatically increased the reliance on telehealth, transforming virtual care from a niche service to a vital component of healthcare delivery. Prior to the pandemic, telehealth adoption faced barriers such as reimbursement limitations and regulatory hurdles. However, the urgent need for remote consultations and monitoring during lockdowns swiftly removed these obstacles. Patients, particularly those in rural areas or with mobility issues, gained significantly improved access to specialists and routine care.
For example, virtual consultations for chronic conditions like diabetes and hypertension became commonplace, enabling ongoing management without requiring in-person visits. This increased accessibility led to better health outcomes for many patients who might have otherwise delayed or forgone essential care. The expanded use of telehealth platforms also allowed for more efficient triage and monitoring of COVID-19 patients, reducing the strain on in-person healthcare facilities.
Development and Deployment of New Diagnostic Tools and Treatments
The pandemic spurred intense research and development efforts leading to significant advancements in diagnostic tools and treatments. Rapid diagnostic tests for COVID-19 were developed and deployed globally, enabling faster identification of infected individuals and facilitating quicker isolation and contact tracing. This rapid development showcased the potential for accelerated innovation in diagnostics, paving the way for similar rapid response capabilities for other infectious diseases.
Furthermore, the pandemic accelerated research into existing and novel treatments for COVID-19, leading to the development and widespread use of antiviral medications, monoclonal antibodies, and ultimately, effective vaccines. These advancements not only improved patient outcomes during the pandemic but also advanced our understanding of viral pathogenesis and treatment strategies, which will likely have lasting implications for future pandemic preparedness.
Table of Pandemic-Driven Innovations
| Innovation | Description | Impact | Future Implications |
|---|---|---|---|
| Telehealth Expansion | Widespread adoption of virtual consultations, remote monitoring, and digital health platforms. | Increased access to care, particularly for rural and underserved populations; improved patient convenience and reduced healthcare costs in some instances. | Continued integration of telehealth into routine care, potentially reducing healthcare disparities and improving efficiency. |
| Rapid Diagnostic Tests | Development and deployment of rapid, point-of-care diagnostic tests for COVID-19. | Faster identification of infected individuals, enabling quicker isolation and contact tracing; improved infection control measures. | Enhanced diagnostic capabilities for future outbreaks and improved surveillance systems for infectious diseases. |
| Development of COVID-19 Treatments | Rapid development and deployment of antiviral medications, monoclonal antibodies, and vaccines. | Improved patient outcomes, reduced severity of illness, and decreased mortality rates. | Advancements in antiviral drug development and vaccine technology, improved understanding of viral pathogenesis. |
| Improved Data Sharing and Collaboration | Increased collaboration between healthcare providers, researchers, and public health agencies facilitated by enhanced data sharing platforms. | Faster dissemination of information, improved coordination of responses to the pandemic, and accelerated research progress. | More robust and efficient public health surveillance systems, enhanced collaboration in future pandemic responses. |
Enhanced Public Health Infrastructure and Response
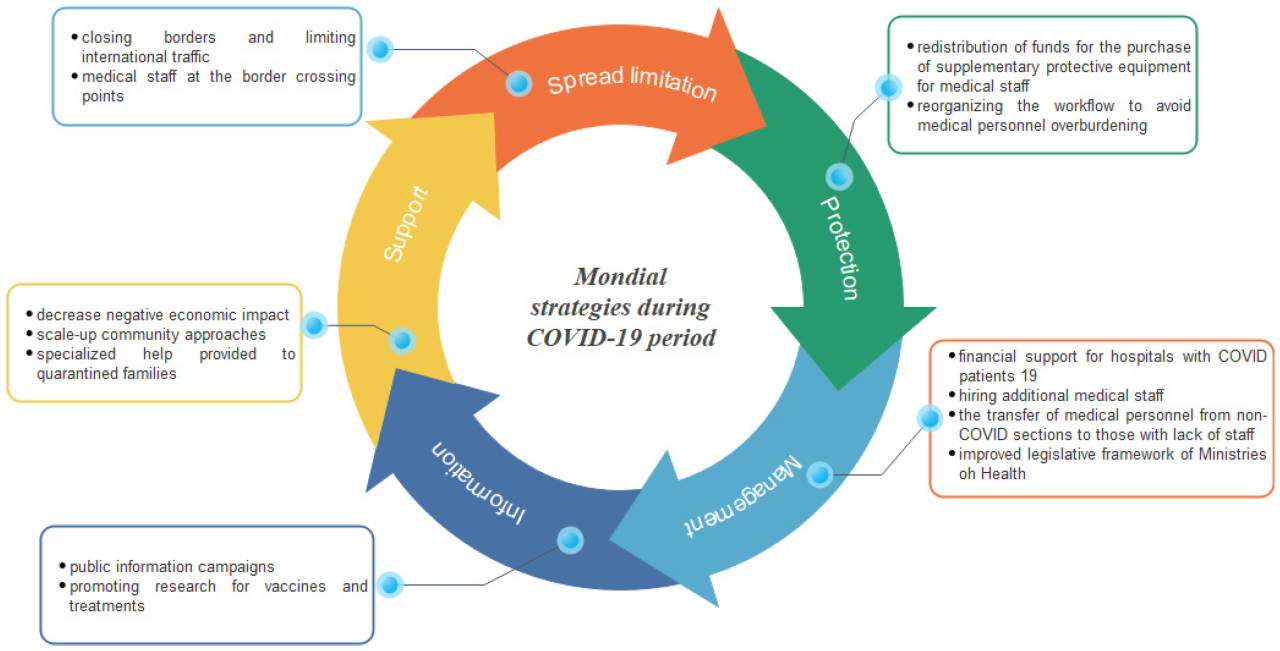
The COVID-19 pandemic exposed significant weaknesses in global public health infrastructure, but it also spurred unprecedented innovation and improvements in preparedness and response capabilities. Many nations learned valuable lessons, leading to significant advancements in surveillance, communication, and resource allocation within their public health systems. These improvements are crucial for mitigating the impact of future outbreaks.The pandemic forced a rapid evolution in how public health agencies operate, particularly concerning data collection, analysis, and dissemination.
This involved not only technological upgrades but also a significant shift in operational strategies and collaborative efforts between different levels of government and international organizations. This section explores some key areas of enhancement.
Improved Public Health Agency Preparedness and Response Capabilities
Many public health agencies significantly increased their capacity for rapid response to outbreaks. This included bolstering laboratory testing capabilities, expanding workforce training programs, and establishing clearer lines of communication and coordination between local, regional, and national levels. For example, the Centers for Disease Control and Prevention (CDC) in the United States invested heavily in improving its epidemiological investigation capacity, allowing for faster identification and containment of outbreaks.
Similarly, many countries strengthened their disease surveillance systems, incorporating real-time data analysis to identify emerging threats more quickly. The establishment of dedicated pandemic response teams, often composed of experts from various fields, also became a common practice.
Development and Implementation of Contact Tracing and Surveillance Systems
Contact tracing, the process of identifying and monitoring individuals who have been in contact with infected persons, became a cornerstone of pandemic response. Many countries implemented digital contact tracing applications, leveraging technology to automate and streamline the process. These apps, while facing privacy concerns in some cases, proved effective in quickly identifying and isolating potential cases. Beyond digital tools, robust manual contact tracing systems were also essential, particularly in areas with limited technological access.
Simultaneously, improved disease surveillance systems, integrating data from various sources (hospital admissions, laboratory results, and mortality data), allowed for better monitoring of the pandemic’s spread and the effectiveness of interventions. This real-time data informed decision-making, enabling a more agile response to changing circumstances.
Successful Public Health Communication Strategies During the Pandemic
Effective communication proved vital in mitigating the pandemic’s impact. Successful strategies involved clear, consistent, and accessible messaging to the public, tailored to diverse audiences and addressing misinformation. Many public health agencies utilized multiple communication channels, including social media, traditional media, and community outreach programs, to disseminate crucial information on preventive measures, testing availability, and treatment options. The use of trusted messengers, such as healthcare professionals and community leaders, also proved crucial in building public trust and promoting adherence to public health guidelines.
Examples include targeted campaigns addressing specific concerns of vulnerable populations and the use of infographics and videos to simplify complex information.
Flowchart Illustrating a Typical Public Health Response to a Pandemic
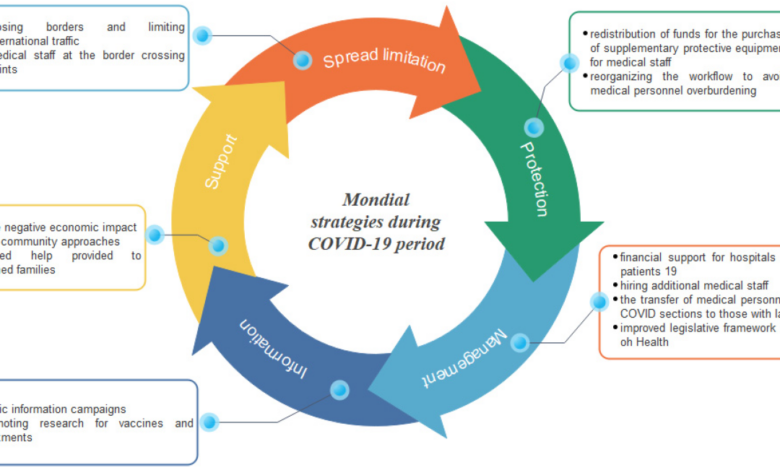
The following flowchart Artikels the key steps in a typical public health response to a pandemic. Note that the specifics can vary depending on the nature of the pathogen and the context.[Diagram description: A flowchart would be included here. It would begin with a box labeled “Detection of Novel Pathogen/Outbreak.” This would lead to a decision diamond: “Is it a significant public health threat?” A “Yes” branch would lead to a series of boxes representing actions: “Activate Pandemic Response Plan,” “Enhance Surveillance,” “Implement Infection Control Measures,” “Communicate Risk to Public,” “Develop and Distribute Vaccines/Treatments (if available),” and “Monitor and Evaluate Response.” A “No” branch from the decision diamond would lead to a box labeled “Continue routine surveillance.” All boxes would connect with arrows indicating the flow of the response process.]
The Role of Data and Technology in Healthcare Advancement
The COVID-19 pandemic dramatically highlighted the critical role of data and technology in managing public health crises and improving healthcare delivery. The sheer volume of information generated – from patient demographics and symptoms to viral genomic sequences and treatment outcomes – underscored the need for sophisticated analytical tools and robust data infrastructure. This surge in data-driven decision-making ultimately spurred significant advancements in healthcare, many of which are likely to reshape the field for years to come.The rapid mobilization of technology and data analytics during the pandemic showcased their transformative potential.
From contact tracing apps to telemedicine platforms, technological solutions were rapidly deployed to address the immediate challenges posed by the virus. However, the pandemic also exposed existing weaknesses in data infrastructure and interoperability, prompting a critical reassessment of data management practices and a renewed focus on collaborative data sharing.
Big Data Analytics in Disease Surveillance and Prediction
Big data analytics played a pivotal role in improving disease surveillance and prediction during the pandemic. By analyzing vast datasets encompassing epidemiological data, social media trends, and mobility patterns, researchers were able to identify emerging outbreaks, predict the spread of the virus, and optimize resource allocation. For instance, analyzing anonymized mobile phone location data helped identify areas with high infection rates, allowing public health officials to target interventions more effectively.
Predictive modeling, using machine learning algorithms trained on historical data and real-time information, enabled more accurate forecasts of hospital bed needs and ventilator requirements, facilitating better preparedness and resource management. These advancements demonstrated the power of big data analytics in enhancing public health preparedness and response.
Technological Advancements in Faster Diagnosis and Treatment
Several key technological advancements facilitated faster diagnosis and treatment during the pandemic. Rapid diagnostic tests, utilizing techniques like PCR and antigen detection, allowed for quicker identification of infected individuals, enabling prompt isolation and contact tracing. Telemedicine platforms, which experienced a massive surge in adoption, enabled remote consultations and monitoring, reducing the strain on healthcare facilities and ensuring continued access to care for patients.
Furthermore, the development and deployment of mRNA vaccines, a testament to advancements in biotechnology and genetic engineering, marked a significant milestone in combating the pandemic. These innovations demonstrated the potential of technology to accelerate the development and delivery of effective healthcare solutions.
Pre-Pandemic and Pandemic Approaches to Data Management and Sharing
Pre-pandemic approaches to data management in healthcare were often characterized by data silos, limited interoperability between systems, and concerns around data privacy and security. Data sharing was often hampered by regulatory barriers and a lack of standardized data formats. The pandemic necessitated a shift towards more collaborative and integrated data management strategies. Data sharing initiatives, such as the sharing of genomic data to track viral mutations, became crucial for coordinating global responses.
While privacy concerns remained paramount, the urgency of the situation fostered greater willingness to share data across institutions and borders. This accelerated the development of secure data sharing platforms and the adoption of standardized data formats, leading to improved data interoperability and more efficient public health responses.
Benefits and Challenges of Using Technology in Healthcare During a Pandemic
The use of technology in healthcare during the pandemic presented numerous benefits and challenges.
- Benefits: Faster diagnosis and treatment, improved disease surveillance and prediction, increased access to care through telemedicine, accelerated vaccine development, enhanced resource allocation, improved communication and coordination among healthcare providers.
- Challenges: Digital divide and unequal access to technology, data privacy and security concerns, interoperability issues between different healthcare systems, the need for robust cybersecurity measures to prevent data breaches, ethical considerations surrounding the use of AI and big data analytics in healthcare decision-making, the need for training and education to ensure effective use of new technologies.
Impact on Healthcare Workforce and Training
The COVID-19 pandemic placed an unprecedented strain on healthcare systems globally, significantly impacting the workforce and necessitating rapid adaptations in training and resource allocation. The sheer volume of patients, coupled with the high risk of infection, created a perfect storm of challenges for healthcare professionals. This section will explore these challenges, the innovative responses implemented, and the resulting outcomes.The pandemic dramatically highlighted existing vulnerabilities within healthcare systems, particularly concerning workforce capacity and preparedness for large-scale health crises.
Healthcare systems showed incredible resilience during the pandemic, adapting and innovating to provide care. A huge step forward in streamlining this process comes from advancements like AI integration in EHRs; for example, check out how nuance integrates generative AI scribe with Epic EHRs to improve efficiency. This kind of technological leap is crucial for healthcare systems to continue making valuable strides, ensuring better patient care in the future.
Healthcare workers faced not only immense physical and emotional burdens but also systemic issues that exacerbated their difficulties. The rapid evolution of the virus and the constantly shifting treatment protocols added another layer of complexity, demanding continuous learning and adaptation.
Healthcare systems showed incredible resilience during the pandemic, adapting to unprecedented challenges. A key area highlighting this adaptability is the continued provision of essential services, even in underserved areas, like the crucial role of rural hospitals in labor and delivery, as detailed in this insightful article: Rural Hospitals Labor Delivery &. This demonstrates how healthcare systems made valuable strides, prioritizing essential care even amidst crisis.
Challenges Faced by Healthcare Workers
Healthcare workers faced a multitude of challenges during the pandemic. These included increased workloads due to a surge in patients, prolonged exposure to a highly contagious virus resulting in high infection rates and burnout, a lack of adequate personal protective equipment (PPE) in the early stages, moral distress from difficult end-of-life decisions and rationing of care, and the emotional toll of witnessing widespread suffering and death.
Healthcare systems showed incredible resilience during the pandemic, adapting rapidly to new challenges. A key area of innovation involves leveraging technology, as highlighted in this fascinating study on study widespread digital twins healthcare , which explores how digital models can improve efficiency and patient care. Ultimately, these advancements underscore the ongoing evolution of healthcare’s ability to meet crises head-on.
The psychological impact, including PTSD and anxiety, was profound and widespread. Many healthcare workers experienced moral injury, a sense of betrayal of their professional values and oaths due to the circumstances.
Adaptations in Healthcare Workforce Training and Education, Healthcare systems make valuable strides in the eye of a pandemic
In response to the pandemic, healthcare systems rapidly adapted training and education programs. Online learning platforms became essential, enabling remote training on infection control protocols, the use of new technologies (like telehealth), and the management of COVID-19 patients. Accelerated training programs were implemented to rapidly upskill existing staff and onboard new recruits. Simulations and virtual reality tools were employed to provide realistic training experiences without exposing trainees to unnecessary risk.
Furthermore, mental health support services became more readily available for healthcare workers, recognizing the significant psychological impact of the pandemic.
Healthcare System Adaptations to Shortages
Facing critical shortages of personnel and resources, healthcare systems implemented several strategies. This included redeploying staff from less critical areas to COVID-19 units, extending working hours (often leading to burnout), recruiting retired healthcare professionals and medical students, leveraging telehealth to reduce the burden on in-person care, and prioritizing the most urgent cases. International collaborations facilitated the sharing of resources and personnel, and innovative approaches such as the use of temporary field hospitals helped to alleviate capacity constraints.
Summary of Challenges and Adaptations
| Challenge | Adaptation | Outcome |
|---|---|---|
| Increased workload and patient volume | Redeployment of staff, extended working hours, recruitment of retired professionals and medical students | Partially mitigated workload, but contributed to staff burnout |
| Shortage of PPE | Rapid procurement and distribution of PPE, innovation in PPE design and manufacturing | Improved PPE availability, but shortages persisted in some areas |
| High infection rates among healthcare workers | Improved infection control protocols, increased access to testing and treatment | Reduced infection rates, but still a significant concern |
| Mental health challenges among healthcare workers | Increased access to mental health services, peer support programs | Improved mental health support, but long-term effects still being assessed |
| Lack of trained personnel | Accelerated training programs, online learning platforms, simulation-based training | Increased workforce capacity, but quality of training varied |
Lessons Learned and Future Preparedness
The COVID-19 pandemic served as a brutal but invaluable stress test for healthcare systems globally. It exposed vulnerabilities, highlighted successes, and ultimately provided a wealth of data to inform future preparedness strategies. Analyzing these lessons learned is crucial to building more resilient and responsive healthcare systems capable of withstanding future pandemics or large-scale health crises.The pandemic underscored the critical need for robust public health infrastructure and a coordinated global response.
Weaknesses in surveillance systems, supply chain management, and communication strategies were painfully evident. Furthermore, the pandemic highlighted existing inequities in healthcare access and outcomes, disproportionately impacting vulnerable populations. Addressing these systemic issues is paramount to ensuring equitable health security for all.
Key Lessons Learned from the Pandemic
The pandemic revealed several critical weaknesses in existing healthcare systems. These included insufficient surge capacity in hospitals, shortages of essential medical supplies like ventilators and personal protective equipment (PPE), and a lack of readily available testing and treatment options in the early stages. Furthermore, the pandemic exposed the critical need for improved data collection, analysis, and dissemination to inform public health decision-making.
Finally, the strain placed on healthcare workers highlighted the importance of workforce planning and training to ensure adequate staffing levels during crises.
Strategies for Improving Healthcare System Resilience
Building resilient healthcare systems requires a multi-pronged approach. This includes investing in robust public health infrastructure, strengthening surveillance systems, and developing strategic national and international stockpiles of essential medical supplies. Furthermore, improving healthcare workforce planning and training, including cross-training healthcare professionals to handle multiple roles during surges, is vital. Investing in advanced technologies, such as telehealth and predictive modeling, can enhance responsiveness and improve the efficiency of healthcare delivery.
Finally, fostering stronger collaboration between healthcare providers, public health agencies, and government entities is crucial for effective crisis management.
Long-Term Implications for Healthcare Policies and Practices
The pandemic is likely to have lasting effects on healthcare policies and practices. Increased emphasis on telehealth and remote monitoring is expected, leading to improved access to care, particularly in rural or underserved areas. Greater investment in public health infrastructure and pandemic preparedness is also anticipated. Furthermore, there’s a growing recognition of the need for equitable access to healthcare, prompting policy changes to address health disparities.
Finally, the pandemic has spurred innovation in vaccine development and deployment, leading to potentially faster responses to future outbreaks.
A Resilient Healthcare System: A Descriptive Illustration
Imagine a healthcare system characterized by robust surveillance systems capable of rapidly detecting and tracking emerging infectious diseases. This system features a well-trained and adequately staffed healthcare workforce equipped with advanced technologies for remote monitoring and telehealth. Strategic national and international stockpiles of essential medical supplies ensure availability during crises. Furthermore, this system incorporates flexible surge capacity in hospitals and other healthcare facilities, allowing for rapid expansion of services during outbreaks.
Finally, this system prioritizes data-driven decision-making, leveraging advanced analytics to inform public health strategies and resource allocation. Effective communication channels ensure seamless coordination between healthcare providers, public health agencies, and the public. Such a system, though requiring significant investment and ongoing refinement, represents a pathway towards greater health security and equitable access to care.
Equity and Access to Healthcare During the Pandemic
Source: coveryou.in
The COVID-19 pandemic exposed and exacerbated existing health inequities, disproportionately impacting vulnerable populations. While the pandemic challenged healthcare systems globally, its impact was far from uniform, highlighting deep-seated disparities in access to care, testing, treatment, and ultimately, vaccines. Understanding these disparities is crucial for building a more resilient and equitable healthcare system for the future.
Disproportionate Impact on Vulnerable Populations
The pandemic revealed stark differences in health outcomes based on race, ethnicity, socioeconomic status, geographic location, and pre-existing health conditions. Individuals from marginalized communities experienced higher rates of infection, hospitalization, and death due to a complex interplay of factors. These include increased exposure risk due to essential worker roles, limited access to quality healthcare, higher rates of chronic diseases, and underlying social determinants of health like housing insecurity and food insecurity.
For example, studies consistently showed higher COVID-19 mortality rates among Black and Hispanic communities compared to white communities, a disparity attributable to a combination of factors including higher rates of underlying health conditions, increased exposure to the virus, and unequal access to quality healthcare.
Initiatives Aimed at Improving Healthcare Equity and Access
In response to the widening health disparities, numerous initiatives emerged to improve equity and access to care. Many organizations focused on expanding telehealth services to reach remote or underserved communities, reducing barriers to accessing care. Mobile testing and vaccination clinics were deployed to increase access in areas with limited healthcare infrastructure. Community health workers played a vital role in outreach, education, and vaccine hesitancy reduction within marginalized communities.
Furthermore, some healthcare systems implemented culturally sensitive communication strategies and language services to ensure effective communication and engagement with diverse patient populations. These initiatives, while valuable, often faced significant challenges in reaching the most vulnerable populations effectively.
Challenges in Ensuring Equitable Access to Vaccines and Treatments
Ensuring equitable access to vaccines and treatments proved to be a major challenge. Vaccine rollout strategies often prioritized healthcare workers and the elderly, leaving vulnerable populations waiting longer. Geographic disparities in vaccine access, coupled with digital literacy barriers and lack of transportation, further hindered equitable distribution. Moreover, misinformation and vaccine hesitancy disproportionately impacted certain communities, leading to lower vaccination rates.
Similar challenges arose with access to effective treatments, particularly for those lacking health insurance or residing in areas with limited access to specialized care. These inequities underscore the need for targeted interventions and robust public health infrastructure to reach all populations.
Disparities in Healthcare Access: Before, During, and After the Pandemic
| Demographic Factor | Before Pandemic | During Pandemic | After Pandemic |
|---|---|---|---|
| Race/Ethnicity (e.g., Black/African American) | Higher rates of chronic diseases, lower access to primary care | Higher infection, hospitalization, and mortality rates; unequal vaccine access | Continued health disparities; need for ongoing interventions |
| Socioeconomic Status (Low Income) | Limited access to insurance, healthcare services, and preventative care | Increased risk of infection due to essential worker roles; delayed or forgone care | Persistent financial barriers to healthcare; ongoing need for affordable care |
| Geographic Location (Rural Areas) | Shortage of healthcare providers, limited access to specialized care | Delayed access to testing, treatment, and vaccines | Continued healthcare workforce shortages; need for telehealth expansion |
| Pre-existing Health Conditions (e.g., Diabetes, Heart Disease) | Higher risk of severe illness and complications | Increased vulnerability to severe COVID-19; higher mortality rates | Increased need for chronic disease management and preventative care |
Last Point
Source: mdpi-res.com
The pandemic, while undeniably devastating, served as a brutal catalyst for progress in healthcare. The innovations and adaptations we’ve witnessed aren’t just temporary fixes; they represent a fundamental reimagining of how we deliver and access care. While challenges remain, the lessons learned – the importance of preparedness, the power of collaboration, and the crucial need for equitable access – will shape the future of healthcare for years to come.
The story isn’t over, but the strides made offer a beacon of hope, a testament to the incredible adaptability and dedication of the healthcare community.
Helpful Answers: Healthcare Systems Make Valuable Strides In The Eye Of A Pandemic
What were some unexpected benefits of the pandemic on healthcare?
The increased adoption of telehealth expanded access to care for remote populations and improved efficiency in some areas. The pandemic also spurred innovation in areas like diagnostics and treatment.
How did the pandemic impact mental health services?
The pandemic significantly increased the demand for mental health services, highlighting pre-existing gaps in access and creating new challenges related to delivering care remotely.
What long-term effects are predicted on healthcare infrastructure?
Experts predict increased investment in digital infrastructure, enhanced pandemic preparedness planning, and a greater focus on resilient healthcare systems capable of handling future crises.





