HHS Final Rule Information Blocking Penalties for Healthcare Providers
Hhs final rule information blocking penalties healthcare providers – HHS Final Rule information blocking penalties for healthcare providers – it sounds scary, right? But understanding this new rule is crucial for every healthcare provider, big or small. This rule aims to improve healthcare data sharing, making it easier for patients to access their own records and for different healthcare systems to communicate effectively. However, failing to comply comes with hefty fines, so let’s dive into what you need to know to stay on the right side of the law and keep your practice running smoothly.
This post breaks down the key aspects of the HHS Final Rule, from understanding what constitutes information blocking to navigating the exceptions and safe harbors. We’ll explore the potential penalties, discuss strategies for compliance, and even look at real-world case studies to illustrate the importance of understanding and adhering to these regulations. Get ready to become an information blocking expert!
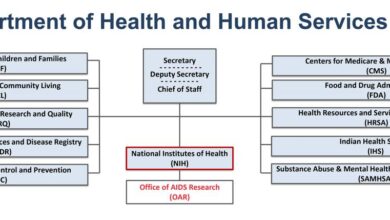
HHS Final Rule Overview

Source: qtxasset.com
The 21st Century Cures Act spurred the development of the HHS Final Rule on Information Blocking, aiming to improve health data exchange and patient access. This rule sets clear expectations for healthcare providers and health information exchanges, outlining what constitutes information blocking and the associated penalties. Understanding this rule is crucial for healthcare professionals to ensure compliance and avoid potential legal repercussions.The HHS Final Rule defines information blocking as practices that interfere with the access, exchange, or use of electronic health information.
It Artikels eight exceptions where information blocking may be permissible, such as preventing security breaches or protecting privacy. However, the burden of proof rests on the provider to demonstrate that an action falls under one of these exceptions. The rule focuses on promoting interoperability and patient empowerment by facilitating seamless data sharing.
Penalties for Information Blocking Violations
Penalties for violating the HHS Final Rule on information blocking can be substantial. The rule establishes a tiered penalty system, with penalties ranging from $1,000 to $10,000 per violation. The specific penalty amount depends on factors such as the severity of the violation, whether it was intentional, and the provider’s history of compliance. For example, a small practice accidentally failing to provide data due to a technical glitch might face a smaller penalty than a large hospital system intentionally restricting access to information for competitive reasons.
The Office of Inspector General (OIG) has the authority to impose these penalties.
Timeline of Rule Implementation and Enforcement
The HHS Final Rule on information blocking went into effect on April 5, 2021. While the initial focus was on education and compliance assistance, enforcement actions began soon after. The OIG has established a process for investigating complaints and determining penalties. The timeline for investigations and penalty assessments can vary depending on the complexity of the case.
While there’s no set timeframe, the OIG actively monitors compliance and takes enforcement action when necessary. Providers should be aware that this is an ongoing process, and continuous monitoring of compliance is essential.
Examples of Information Blocking Actions
Several actions can be considered information blocking under the HHS Final Rule. These include, but are not limited to, refusing to provide electronic health information in a standard format, imposing unreasonable fees for access to data, or using technology that deliberately restricts data exchange. For example, a hospital system that only allows access to its data through a proprietary system that’s incompatible with other systems could be deemed as engaging in information blocking.
Similarly, a physician’s office that consistently delays or denies access to patient records without a legitimate justification could also face penalties. The rule emphasizes the importance of using industry-standard formats and technologies to facilitate seamless data exchange.
Penalties and Enforcement Mechanisms
The HHS Final Rule on Information Blocking Artikels a robust system of penalties and enforcement mechanisms designed to deter violations and ensure the free flow of health information. Understanding these mechanisms is crucial for healthcare providers to maintain compliance and avoid potentially significant financial repercussions. The severity of penalties varies depending on the nature and extent of the violation, as well as the provider’s history of compliance.The HHS Office of Inspector General (OIG) plays a central role in investigating potential information blocking violations.
Their investigations can stem from complaints, audits, or self-reporting by providers. The process involves gathering evidence, interviewing witnesses, and analyzing the provider’s practices to determine whether information blocking occurred and, if so, the extent of the violation. This investigative process can be lengthy and complex, requiring significant resources from both the OIG and the provider under investigation.
Levels of Penalties for Information Blocking Violations
Penalties for information blocking range from relatively minor civil monetary penalties (CMPs) to significant financial repercussions, including exclusion from federal healthcare programs. The amount of the CMP is determined on a case-by-case basis, considering factors such as the severity of the violation, the provider’s knowledge and intent, and their cooperation with the investigation. For example, a minor, unintentional violation might result in a relatively low CMP, while a willful and widespread practice of information blocking could lead to substantial penalties and potential exclusion from Medicare and Medicaid.
The OIG has the authority to impose penalties ranging from thousands to millions of dollars, depending on the circumstances.
Investigation and Enforcement Process
The OIG’s investigation typically begins with a preliminary assessment to determine whether a violation has occurred. If a violation is suspected, a formal investigation is launched, which may include on-site visits, document reviews, and interviews with staff and patients. Throughout this process, providers are expected to cooperate fully with the OIG’s requests for information. Failure to cooperate can result in increased penalties.
Following the investigation, the OIG issues a report outlining its findings and recommendations. If a violation is confirmed, the OIG can impose penalties, including CMPs and potential exclusion from federal healthcare programs. Providers have the right to appeal the OIG’s decision through administrative processes.
Factors Influencing Penalty Severity
Several factors influence the severity of penalties imposed for information blocking violations. These include the nature and extent of the violation (was it a single incident or a pattern of behavior?), the provider’s knowledge and intent (was the blocking intentional or unintentional?), the impact on patients (did the blocking cause harm or delay in care?), and the provider’s history of compliance (has the provider had previous violations?).
The OIG also considers the provider’s efforts to remedy the situation and cooperate with the investigation. Demonstrating a commitment to correcting the problem and preventing future violations can mitigate the severity of the penalties.
Hypothetical Scenario Illustrating Potential Financial Impact
Imagine a large hospital system that intentionally restricts access to patient data for a competitor’s telehealth platform, resulting in delayed or denied care for patients. This action constitutes a significant violation of the information blocking rule. The OIG, after a thorough investigation, could impose a CMP of several million dollars, depending on the number of patients affected and the duration of the violation.
Additionally, the hospital system could face exclusion from Medicare and Medicaid, leading to a substantial loss of revenue and potential damage to its reputation. This scenario highlights the potentially devastating financial consequences of non-compliance with the information blocking rule.
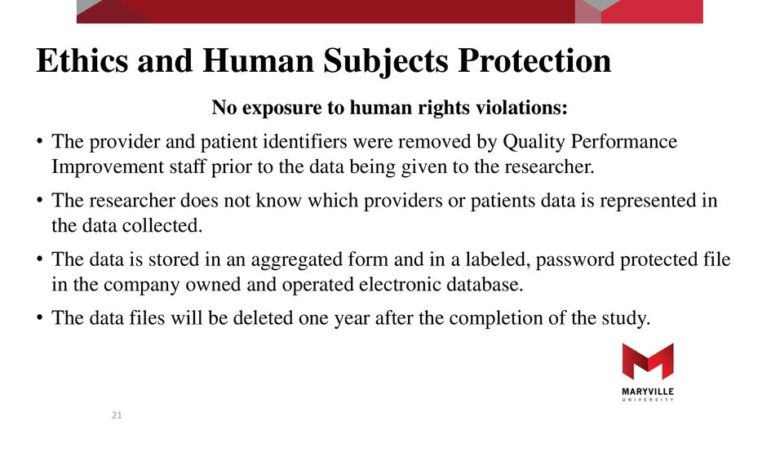
Impact on Healthcare Providers
Source: slideplayer.com
The HHS Final Rule on Information Blocking has significant implications for healthcare providers of all sizes, impacting their operational workflows, technological investments, and potential legal liabilities. Understanding these impacts is crucial for successful navigation of the new regulatory landscape. This section will delve into the specific challenges faced by different sized providers, the rule’s effects on data exchange, and the resources available to ensure compliance.
Challenges Faced by Large vs. Small Healthcare Providers
Large healthcare systems and smaller practices face distinct challenges in complying with the information blocking rule. Large organizations, with their extensive IT infrastructure and diverse provider networks, often grapple with the complexities of integrating disparate systems and ensuring consistent data exchange policies across their entire enterprise. This requires significant investment in both technology and personnel to achieve seamless interoperability.
The HHS final rule on information blocking penalties is a big deal for healthcare providers, impacting how they share patient data. This is especially relevant considering advancements like the fda approves clinical trials for pig kidney transplants in humans , where seamless data exchange between researchers and clinicians will be crucial for success. The penalties for non-compliance could significantly hinder such collaborations, potentially slowing down the progress of life-saving innovations.
Conversely, smaller practices may lack the financial resources and technical expertise to implement the necessary upgrades and training. They may struggle to find and implement compliant solutions, potentially facing disproportionate burdens compared to their larger counterparts. For example, a large hospital system might have dedicated IT teams to manage updates and compliance, while a small clinic might rely on a single employee to handle all IT and compliance tasks.
This difference in resources significantly impacts their ability to meet the rule’s demands.
Effects of the Rule on Interoperability and Data Exchange
The Information Blocking Rule aims to significantly improve interoperability and data exchange within the healthcare ecosystem. By prohibiting certain actions that hinder data access, the rule fosters a more collaborative environment where patients and providers can readily share information. This can lead to improved care coordination, reduced medical errors, and enhanced patient outcomes. For instance, seamless access to patient records across different healthcare systems could prevent duplicate testing, leading to cost savings and improved patient experience.
However, successful implementation depends on the willingness and ability of providers to adopt compatible technologies and workflows. The potential for improved data exchange is significant, but realizing it requires substantial effort across the entire healthcare industry.
Resources and Support for Compliance
The HHS offers several resources to assist healthcare providers in complying with the information blocking rule. These resources include guidance documents, educational materials, and technical assistance programs. Additionally, various private sector organizations provide consulting services and technology solutions to support compliance efforts. For instance, the ONC (Office of the National Coordinator for Health Information Technology) website offers a wealth of information and tools related to interoperability and the information blocking rule.
Many vendors also offer certified health IT products that assist with compliance. These resources are critical in helping providers understand their obligations and implement necessary changes to ensure they are compliant. However, access to and utilization of these resources may vary depending on factors like provider size, technical capabilities, and financial resources.
Key Compliance Requirements and Potential Penalties
| Requirement | Penalty Type | Maximum Penalty Amount | Example of Violation |
|---|---|---|---|
| Implementing reasonable and necessary safeguards to protect patient data | Civil Monetary Penalty (CMP) | $1,000 per violation | Failing to implement appropriate security measures, resulting in a data breach. |
| Responding to requests for patient data in a timely manner | Civil Monetary Penalty (CMP) | $1,000 per violation | Unreasonably delaying or denying a patient’s request for their medical records. |
| Using certified health IT products that meet interoperability standards | Civil Monetary Penalty (CMP) | $1,000 per violation | Using a non-certified EHR system that does not support the exchange of information with other systems. |
| Ensuring that information exchange processes are not unduly burdensome | Civil Monetary Penalty (CMP) | $1,000 per violation | Requiring excessive documentation or fees for accessing patient data. |
Exceptions and Safe Harbors
The HHS Information Blocking Rule, while aiming to promote data exchange, acknowledges that complete interoperability isn’t always feasible or desirable. Therefore, it includes several exceptions and safe harbors that allow healthcare providers to restrict information access under specific circumstances. Understanding these exceptions is crucial for avoiding penalties. These exceptions aren’t loopholes; they’re carefully defined allowances for situations where blocking information is justified.The rule Artikels several exceptions, each with specific criteria.
Meeting these criteria is vital for invoking the exception and avoiding penalties. Failure to meet these criteria could result in hefty fines. The safe harbors provide additional protection for certain activities, providing further clarity on permissible information blocking practices.
Privacy Exceptions
The rule recognizes that certain information must be protected due to privacy concerns. This exception allows healthcare providers to restrict access to protected health information (PHI) when disclosure would violate privacy laws, such as HIPAA. Providers must demonstrate a good-faith effort to comply with applicable privacy regulations. For example, a provider might restrict access to PHI related to a patient’s substance abuse treatment, complying with HIPAA’s specific provisions for such information.
The provider would need to document their reasoning and demonstrate compliance with relevant privacy regulations.
Security Exceptions
This exception allows providers to restrict access to information to protect the security of their systems. Criteria include demonstrating a reasonable belief that access would compromise the security or integrity of electronic health information (EHI). This might involve restricting access to certain data elements during a security breach investigation or when dealing with vulnerabilities in their systems. A hospital, for instance, might temporarily restrict access to its patient database following a ransomware attack to prevent further damage and ensure data integrity.
Proper documentation of the security threat and the steps taken to mitigate it are crucial.
Health Information Integrity Exceptions
This exception allows for information blocking to maintain the integrity of health information. This could involve preventing access to incomplete or inaccurate data to avoid the spread of misinformation. For example, a provider might restrict access to a lab report that’s still pending verification to prevent the dissemination of potentially erroneous results. The provider would need to show that the data was incomplete or inaccurate, and that access was restricted until the information was corrected or verified.
Other Exceptions
The rule also provides for exceptions related to preventing harmful actions, protecting patient safety, and maintaining the proper functioning of the healthcare provider’s systems. These exceptions require a demonstrable connection between the information blocking and the identified need. For instance, blocking access to a patient’s medical record to prevent a known abuser from accessing sensitive information would fall under this category.
Thorough documentation justifying the need for the restriction is essential.
Safe Harbor for Preventing Harm
The rule establishes a safe harbor for activities undertaken to prevent harm to a patient or others. This safe harbor protects providers who restrict access to information if they reasonably believe that disclosure would cause harm. A hospital restricting access to a patient’s mental health records to prevent them from self-harm would be protected under this safe harbor.
The provider’s actions must be reasonable and proportionate to the potential harm.
Flowchart for Determining Applicability of Exceptions
[Imagine a flowchart here. The flowchart would begin with a decision point: “Is information access being restricted?” If yes, it would branch to another decision point: “Does a valid exception apply (Privacy, Security, Integrity, Other)?” If yes, it would lead to a final decision: “Exception applies; information blocking may be permissible.” If no, it would lead to another decision point: “Does a safe harbor apply (Preventing Harm)?” If yes, it leads to “Safe harbor applies; information blocking may be permissible.” If no to both exceptions and safe harbors, it leads to the final decision: “Exception does not apply; information blocking may be prohibited.”]
Best Practices for Compliance
Navigating the complexities of the HHS Final Rule on information blocking requires a proactive and multi-faceted approach. Healthcare providers must implement robust strategies to ensure compliance and avoid potential penalties. This involves not only understanding the rule’s intricacies but also establishing a culture of data sharing and responsible information governance.Implementing a robust information governance framework is crucial for avoiding information blocking violations.
This goes beyond simply having a policy in place; it requires a commitment to consistent execution and continuous improvement. Effective governance ensures that data is readily available, usable, and accessible while protecting patient privacy and security.
Information Governance Policies
A strong information governance program includes clearly defined policies and procedures for data access, use, and exchange. These policies should be regularly reviewed and updated to reflect changes in technology, regulations, and best practices. Key elements include defining roles and responsibilities for data management, establishing data quality standards, and outlining processes for handling data requests. For instance, a well-defined policy might specify the timeframes for responding to requests for patient information, the acceptable methods of transmission, and the individuals authorized to approve or deny access.
Furthermore, the policy should detail procedures for addressing exceptions and potential conflicts. Regular audits and assessments of the information governance program are essential to ensure ongoing compliance.
Staff Training and Education
Ongoing training and education are vital for ensuring that all healthcare staff understand and adhere to information blocking regulations. Training programs should cover the key provisions of the rule, including definitions of information blocking, permissible exceptions, and potential penalties. The training should be tailored to the specific roles and responsibilities of different staff members. For example, clinicians might need training on using certified health IT products and understanding the permissible uses of their clinical decision support systems.
Administrative staff might need training on data exchange processes and the handling of data requests. Regular refresher courses and updates are essential to keep staff abreast of any changes in regulations or best practices. This can be achieved through online modules, in-person workshops, or a combination of both.
Technology’s Role in Compliance
Technology plays a significant role in ensuring compliance with the information blocking rule. Certified health IT products can help healthcare providers automate data exchange processes, improve data quality, and reduce the risk of information blocking. These tools can facilitate secure and efficient sharing of information with other healthcare providers and patients. Implementing a robust electronic health record (EHR) system with robust interoperability capabilities is a critical step.
Furthermore, employing data analytics tools can help organizations identify potential information blocking risks and areas for improvement. Regularly monitoring the performance of these systems and addressing any issues promptly is key. For example, a healthcare provider might use a tool to monitor the time it takes to fulfill a data request, allowing them to identify bottlenecks and improve their processes.
Another example is employing automated tools to ensure data quality, flagging inconsistencies or errors before they lead to information blocking issues.
Future Implications of the Rule
The HHS information blocking rule, while designed to improve data flow and interoperability, carries significant long-term implications for the healthcare industry. Its effects will ripple through various aspects of healthcare delivery, technology development, and regulatory oversight for years to come. Understanding these potential consequences is crucial for healthcare providers and technology developers alike to adapt and thrive in the evolving landscape.The rule’s impact extends beyond immediate compliance.
Its success hinges on consistent enforcement and the adaptability of the healthcare ecosystem. While initial penalties may focus on egregious violations, the long-term effect will be a cultural shift towards data sharing and a more collaborative approach to patient care. This shift will require ongoing investment in technology, workforce training, and a re-evaluation of established business models.
Potential Future Revisions and Updates
The HHS information blocking rule is not static. Given the rapid pace of technological advancement and the evolving understanding of data sharing best practices, future revisions are highly likely. We can expect adjustments based on implementation experiences, feedback from stakeholders, and emerging technological capabilities. For instance, the definition of “information blocking” itself might need refinement as new technologies and data formats emerge.
Furthermore, future updates could clarify ambiguous areas of the rule, address unforeseen challenges, or incorporate lessons learned from enforcement actions. The experience with HIPAA, which has undergone numerous updates and clarifications over the years, serves as a precedent for ongoing evolution of this rule as well.
Impact on Innovation and Technological Advancements
The rule’s influence on innovation is complex. While some argue it could stifle innovation by imposing compliance burdens, a counterargument suggests it will accelerate the development of interoperable health IT systems. The increased demand for seamless data exchange will likely drive innovation in areas such as AI-powered diagnostic tools, predictive analytics for patient care, and streamlined clinical workflows. For example, the need for standardized APIs and data exchange protocols will likely spur the creation of more efficient and secure solutions.
However, the cost of compliance could disproportionately affect smaller healthcare providers, potentially slowing innovation in that sector.
Potential Future Challenges
The successful implementation of the information blocking rule faces several potential challenges:
The following points highlight key obstacles to successful and complete implementation:
- Maintaining Consistent Enforcement: Ensuring consistent and equitable enforcement across diverse healthcare settings will be a significant ongoing challenge. Variations in resources and technological capabilities among providers could lead to disparities in compliance levels.
- Addressing Data Security Concerns: Balancing the need for data sharing with robust data security measures is crucial. Future challenges may involve mitigating the risk of data breaches and ensuring compliance with other relevant regulations, such as HIPAA.
- Adapting to Emerging Technologies: The rapid evolution of healthcare technologies requires the rule to adapt accordingly. Future challenges will involve clarifying the rule’s application to new technologies and data formats that may not have been considered during its initial development.
- Balancing Patient Privacy with Data Sharing: Striking a balance between enabling data sharing for improved care and protecting patient privacy remains a critical ongoing challenge. This necessitates continuous refinement of data anonymization techniques and robust consent mechanisms.
- Cost of Compliance for Smaller Providers: The financial burden of compliance could disproportionately affect smaller healthcare providers, potentially hindering their ability to adopt new technologies and participate fully in the interconnected healthcare ecosystem.
Case Studies
While the HHS Final Rule on information blocking doesn’t yet boast a lengthy list of publicly available, detailed penalty cases, the potential for penalties is very real, and we can learn from the spirit of the rule and early enforcement actions. Analyzing these situations, even hypothetically, highlights the critical aspects of compliance. Remember, the goal isn’t just avoiding penalties; it’s about ensuring seamless patient care through data accessibility.
The HHS final rule on information blocking penalties for healthcare providers is a huge deal, impacting everything from data access to patient care. It’s a complex issue, and sometimes I feel like my brain needs a little break! I was reading about Karishma Mehta’s decision to freeze her eggs and the risks involved, karishma mehta gets her eggs frozen know risks associated with egg freezing , which reminded me how crucial readily accessible health information is for informed choices.
Getting back to the HHS rule, understanding these penalties is key for providers to avoid hefty fines and ensure patient well-being.
Hypothetical Case Study: Denied Access to Patient Records
Imagine a large hospital system that uses a proprietary EHR system. They deny a smaller, independent clinic access to a patient’s records, citing concerns about system compatibility and data security. This action, however, restricts the patient’s access to their own complete medical history, directly hindering their care. While the hospital may argue that it is not intentionally blocking information, the lack of a reasonable and timely solution to allow access could be construed as information blocking under the rule.
This could result in significant penalties and reputational damage.
The key takeaway here is that the focus should be on patient access, not technological limitations. Finding solutions to share data, even with systems that differ, is paramount. A proactive approach to data exchange, rather than a reactive one, is essential for compliance.
Hypothetical Case Study: Unreasonable Fees for Data Access
A radiology practice charges exorbitant fees for accessing patient imaging data, far exceeding the cost of providing the information. This practice effectively limits access, particularly for smaller clinics or individual physicians who might not be able to afford the high cost. The HHS Final Rule addresses unreasonable fees as a form of information blocking. This could lead to significant fines and potential legal action.
Charging excessive fees for accessing patient data is a clear violation of the spirit and intent of the information blocking rule. Transparency and reasonable pricing are critical for compliance. The focus should be on the cost of providing the data, not maximizing profits.
The HHS final rule on information blocking penalties is a big deal for healthcare providers, impacting everything from data sharing to patient care. Understanding timely access to critical patient data is crucial, especially considering the severity of conditions like stroke. Knowing the risk factors that make stroke more dangerous, as detailed in this article risk factors that make stroke more dangerous , highlights the importance of rapid information exchange for effective treatment.
Therefore, navigating the complexities of the HHS rule becomes even more critical for providing the best possible care in time-sensitive situations.
Hypothetical Case Study: Lack of Interoperability, Hhs final rule information blocking penalties healthcare providers
A large physician group uses an older EHR system that is not compatible with many other systems. They make little effort to update their system or find workarounds to allow for seamless data exchange with other providers. This results in significant delays in patient care as other providers struggle to access necessary information. While not necessarily intentional, this lack of interoperability could be considered information blocking if it demonstrably harms patient care.
The resulting penalties would be determined based on the severity of the impact and the lack of effort to address the interoperability issues.
The lesson here is the importance of proactive planning and system modernization. Failure to invest in interoperable systems, coupled with a lack of viable alternatives for data sharing, can lead to significant penalties. Regular system reviews and updates are crucial.
Epilogue
Navigating the HHS Final Rule on information blocking can feel overwhelming, but it’s essential for the future of healthcare interoperability and patient care. By understanding the key provisions, potential penalties, and available resources, healthcare providers can proactively implement strategies to ensure compliance and avoid costly fines. Remember, this isn’t just about avoiding penalties; it’s about fostering a more connected and efficient healthcare system that ultimately benefits patients.
Stay informed, stay compliant, and let’s work together to improve healthcare access for everyone.
Question Bank: Hhs Final Rule Information Blocking Penalties Healthcare Providers
What constitutes “information blocking” under the HHS Final Rule?
Information blocking broadly refers to practices that unreasonably interfere with or impede access, exchange, or use of electronic health information. This includes things like failing to provide data in a usable format or unnecessarily delaying access to information.
Are there any resources available to help healthcare providers comply with the rule?
Yes! ONC (Office of the National Coordinator for Health IT) offers guidance documents, webinars, and other resources to assist providers in understanding and complying with the rule. Many professional organizations also provide support and training.
How are penalties determined?
Penalty amounts vary depending on factors such as the severity and nature of the violation, the provider’s knowledge of the rule, and whether they made a good faith effort to comply. The penalties can range from warnings to substantial financial fines.
What if my practice is small? Are there different compliance requirements?
While the core requirements are the same, the ONC recognizes that smaller practices may face unique challenges. They encourage smaller providers to seek out resources and support tailored to their specific needs and circumstances.