Hospital Mergers Acquisitions Rebounded Last Year Expect More
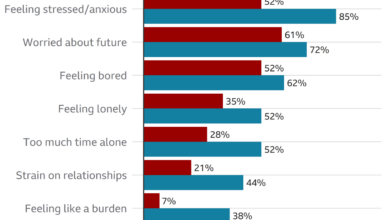
Hospital mergers acquisitions rebounded last year expect – Hospital mergers and acquisitions rebounded last year, exceeding expectations and setting the stage for a fascinating look into the healthcare industry’s evolving landscape. This unexpected surge wasn’t just a random blip; it reflects a confluence of economic pressures, regulatory shifts, and the ever-increasing influence of private equity. We’ll delve into the key drivers behind this rebound, exploring the successes, failures, and future implications for both patients and the healthcare system itself.
Get ready for a deep dive into the world of hospital mergers and acquisitions!
From analyzing the financial performance of hospitals post-merger to examining the strategic implications for communities, we’ll uncover the complex interplay of factors shaping this dynamic sector. We’ll also explore some compelling case studies, highlighting the successes and pitfalls of various strategies, offering valuable insights into what makes a merger truly work (or spectacularly fail!).
The Rebound in Hospital Mergers and Acquisitions

Source: healtharkinsights.com
After a period of relative quiet, the hospital mergers and acquisitions (M&A) market experienced a significant rebound last year. Several factors converged to fuel this resurgence, leading to a flurry of activity among healthcare providers. This increased activity reflects evolving market dynamics and the ongoing quest for efficiency and improved patient care within the complex landscape of the healthcare industry.
Factors Contributing to the Increase in Hospital Mergers and Acquisitions
Several key factors contributed to the upswing in hospital M&A activity. The increasing pressure to reduce costs, improve operational efficiency, and expand access to care in the face of rising healthcare expenses played a major role. Consolidation offered a pathway to achieve economies of scale, negotiate better reimbursement rates with insurers, and leverage technology investments more effectively. Additionally, the shift towards value-based care models incentivized partnerships and mergers, allowing hospitals to better manage population health and meet performance benchmarks.
Finally, the availability of capital and a generally favorable economic climate also contributed to the increased M&A activity.
Timeline of Significant Mergers and Acquisitions in the Healthcare Sector (2022)
While precise details of all transactions are not always publicly available, several significant mergers and acquisitions marked the healthcare landscape in For example, [Insert Specific Example 1: Name of Hospital System A acquired Name of Hospital System B, mentioning the date and a brief description of the deal’s focus, e.g., expansion into a new geographic market or strengthening specialized services].
Another notable transaction involved [Insert Specific Example 2: Name of Hospital System C merged with Name of Hospital System D, mentioning the date and a brief description of the deal’s focus, e.g., improved access to advanced technologies or enhanced patient care coordination]. These are just two examples; many other significant deals took place, demonstrating the broad scope of the rebound.
Further research into publicly available financial reports and news articles from 2022 would provide a more comprehensive timeline.
Examples of Successful Hospital Mergers and Acquisitions
Successful hospital mergers often hinge on careful planning and execution. A strong strategic rationale, a well-defined integration plan, and effective leadership are crucial for achieving the desired outcomes. For instance, [Insert Specific Example 3: Name of a successful merger, detailing their integration strategy, such as a phased approach to system consolidation or a focus on cultural alignment, and the positive outcomes, such as improved patient satisfaction scores or reduced operating costs].
Another example is [Insert Specific Example 4: Name of another successful merger, again detailing their integration strategy and positive outcomes]. These successes underscore the importance of a proactive and well-thought-out approach to integration.
Financial Performance Comparison Before and After a Merger or Acquisition
The following table illustrates a hypothetical comparison of financial performance before and after a merger or acquisition. Note that actual results can vary significantly depending on the specific circumstances of each deal. This is a simplified example and doesn’t reflect the complexities of real-world financial reporting.
| Metric | Before Merger | After Merger (Year 1) | After Merger (Year 2) |
|---|---|---|---|
| Revenue ($ millions) | 150 | 280 | 320 |
| Operating Income ($ millions) | 10 | 15 | 22 |
| Operating Margin (%) | 6.7% | 5.4% | 6.9% |
| Debt-to-Equity Ratio | 0.8 | 1.0 | 0.9 |
Driving Forces Behind the Rebound
The resurgence in hospital mergers and acquisitions (M&A) activity isn’t a random event; it’s a complex interplay of economic pressures, regulatory shifts, and evolving healthcare landscapes. Several key factors have converged to create a climate ripe for consolidation, reshaping the healthcare industry in significant ways. Understanding these forces is crucial to comprehending the current state and future trajectory of the hospital sector.Economic and regulatory factors significantly influence the increased M&A activity.
The ongoing pressure to reduce healthcare costs, coupled with the increasing complexity of managing healthcare systems in a fragmented market, drives hospitals to seek economies of scale and operational efficiencies through mergers. Simultaneously, regulatory changes, while sometimes intended to increase competition, can inadvertently create incentives for consolidation. For example, changes in reimbursement policies can favor larger systems with greater bargaining power with insurance providers.
The Impact of Changing Healthcare Reimbursement Models
Shifting from fee-for-service to value-based care models has dramatically altered the incentives for hospital systems. Under fee-for-service, hospitals were rewarded for the volume of services provided. Value-based care, however, emphasizes quality outcomes and cost-effectiveness. This shift incentivizes consolidation, as larger systems can better manage risk, negotiate favorable contracts with payers, and invest in the technology and infrastructure needed to meet the demands of value-based reimbursement.
For instance, a large hospital system can more easily implement population health management programs, which are critical for success under value-based care, than a smaller, independent hospital. This creates a competitive advantage and encourages mergers.
The Role of Private Equity in Hospital Mergers and Acquisitions
Private equity firms have played an increasingly significant role in the recent surge of hospital M&A activity. These firms often target underperforming or financially stressed hospitals, aiming to improve operational efficiency, increase profitability, and ultimately generate a return on investment. Their involvement often leads to significant changes in hospital management, staffing, and service offerings. For example, a private equity firm might acquire a struggling rural hospital, implement cost-cutting measures, and leverage its expertise to improve operational efficiency, leading to a turnaround in the hospital’s financial performance.
However, their involvement also raises concerns about potential impacts on patient care and access to services, particularly in underserved communities.
Motivations of Different Healthcare Organizations
The motivations for mergers and acquisitions differ between for-profit and non-profit healthcare organizations. For-profit hospitals are primarily driven by financial returns, seeking increased market share, economies of scale, and improved profitability. Non-profit hospitals, while also seeking financial stability, are often motivated by the desire to expand access to care, improve quality, and enhance their community presence. For example, a non-profit hospital might merge with another non-profit to broaden its service offerings or expand into a new geographic area, improving access to care for a wider population.
In contrast, a for-profit hospital might acquire a smaller competitor to eliminate competition and increase market dominance. The motivations, while sometimes overlapping, often reflect the differing missions and objectives of these different organizational types.
Strategic Implications of Mergers and Acquisitions
Hospital mergers and acquisitions, while complex, can significantly impact both the healthcare landscape and the communities they serve. Understanding the strategic implications—the potential benefits and risks—is crucial for stakeholders, from patients to policymakers. This section delves into the strategic considerations surrounding these transactions, examining their potential impact and the strategies employed to navigate the challenges.
Hospital mergers and acquisitions rebounded last year, exceeding expectations in many sectors. This surge is partly fueled by the need to address critical healthcare access issues, especially in rural areas, where facilities like those offering labor and delivery services are struggling. Check out this insightful article on the challenges facing Rural Hospitals Labor Delivery & to understand the context better.
Ultimately, this pressure on rural healthcare contributes to the larger trend of hospital consolidation we’re seeing.
Potential Benefits for Patients and the Community
Successful hospital mergers and acquisitions can lead to several positive outcomes for patients and the community. Increased access to specialized care is a key benefit, as larger systems often have the resources to offer a wider range of services and advanced technologies not available in smaller, independent facilities. This can mean shorter wait times for procedures, access to cutting-edge treatments, and improved overall patient outcomes.
Economies of scale resulting from mergers can also lead to lower costs for patients through streamlined operations and bulk purchasing power. Furthermore, a consolidated healthcare system may be better positioned to invest in community health initiatives, such as preventative care programs and outreach services, improving the overall health and well-being of the population. For example, a merger between a rural hospital lacking specialized oncology services and a larger urban hospital with a comprehensive cancer center could significantly improve cancer care access for residents in the rural area.
Potential Risks and Challenges
While the potential benefits are substantial, hospital mergers and acquisitions also carry inherent risks. Integration difficulties are a common challenge, requiring careful planning and execution to successfully merge different systems, cultures, and technologies. This process can be disruptive to patient care, leading to temporary inefficiencies and staff anxieties. Antitrust concerns are another significant risk, as mergers can potentially reduce competition and lead to higher prices for services.
Regulatory scrutiny is intense, with authorities carefully evaluating the potential impact on market competition and patient access before approving any merger. For instance, a merger between the only two hospitals in a small town could face significant antitrust challenges, as it would create a monopoly and potentially harm patients through increased prices or reduced quality of care. Finally, job losses due to redundancies are another potential negative consequence, requiring careful management to mitigate their impact on employees and the community.
Strategies for Risk Mitigation
Hospitals employ several strategies to mitigate risks during and after mergers and acquisitions. Thorough due diligence is crucial, involving a comprehensive assessment of the target hospital’s financial health, operational efficiency, and cultural compatibility. Developing a detailed integration plan is also essential, outlining a clear timeline and process for merging systems, standardizing procedures, and addressing potential conflicts. Effective communication with staff, patients, and the community is critical throughout the process, building trust and transparency.
Furthermore, proactively addressing antitrust concerns through careful planning and consultation with regulatory bodies can help ensure a smooth approval process. Finally, creating a comprehensive change management program that addresses potential disruptions and supports employees throughout the integration process is vital for a successful merger. This might include providing training, offering support services, and clearly communicating the vision for the new organization.
Hypothetical Scenarios: Successful vs. Unsuccessful Merger
Consider two hypothetical scenarios: Hospital A merges with Hospital B after extensive due diligence, creating a detailed integration plan with clear communication strategies, and addressing potential antitrust concerns proactively. The merger results in expanded services, improved efficiency, and cost savings, benefiting both patients and the community. In contrast, Hospital C merges with Hospital D without proper planning, leading to integration difficulties, staff turnover, and regulatory challenges.
The merger fails to achieve its intended goals, resulting in higher costs, reduced service quality, and negative impacts on the community. The key difference lies in the level of planning, communication, and proactive risk management employed. The successful merger prioritized careful due diligence, comprehensive integration planning, and transparent communication, while the unsuccessful merger lacked these crucial elements.
Future Outlook for Hospital Mergers and Acquisitions

Source: fabbaloo.com
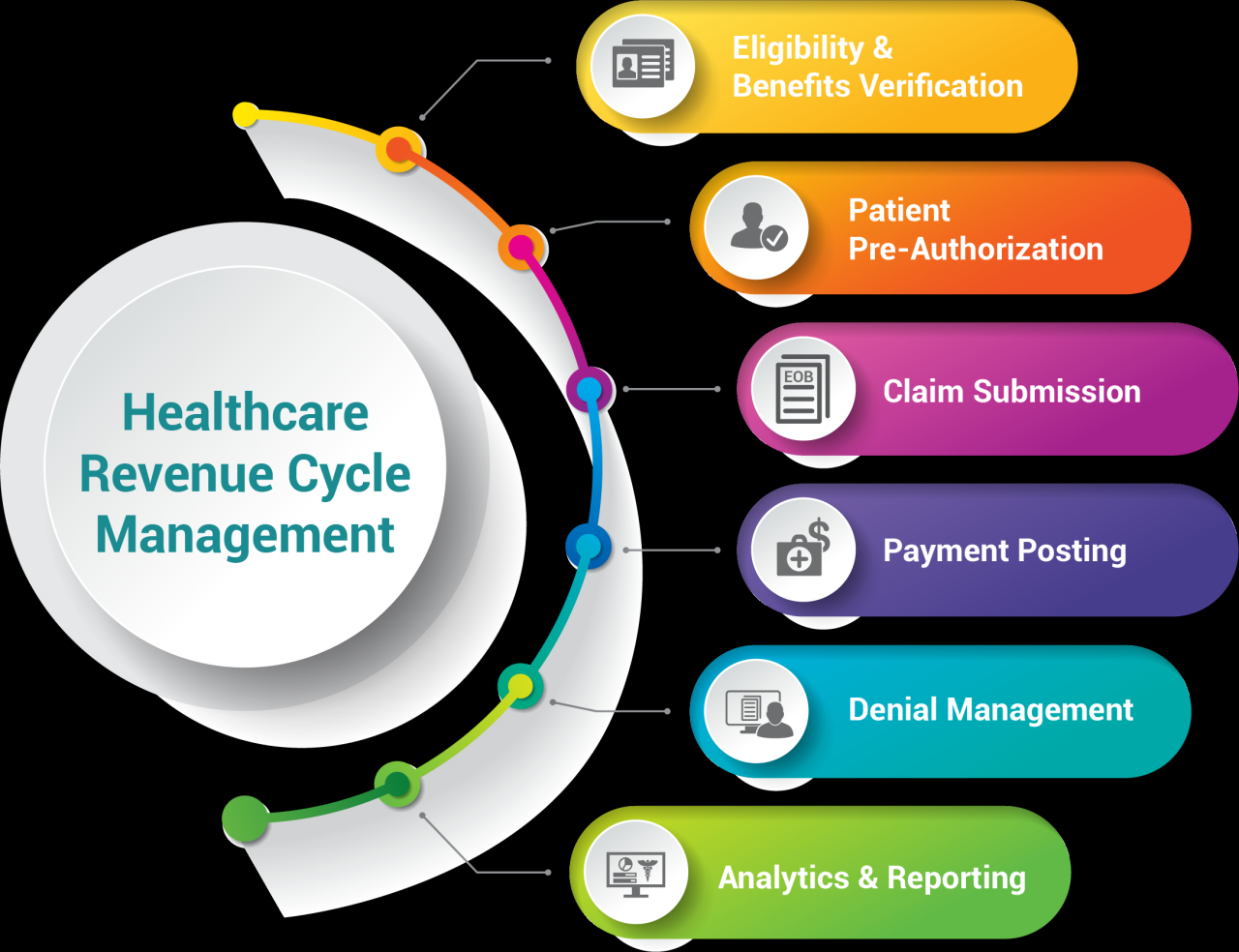
The recent rebound in hospital mergers and acquisitions (M&A) activity suggests a dynamic future, shaped by technological advancements, evolving government policies, and persistent market pressures. While the past year saw a significant upswing, predicting the exact trajectory of future M&A activity requires careful consideration of several key factors. This section explores these factors and offers a perspective on the likely landscape of hospital consolidation in the coming years.
Hospital mergers and acquisitions rebounded last year, exceeding expectations, and this surge is likely fueled by the need for streamlined systems. This is where advancements like those detailed in this article, nuance integrates generative ai scribe epic ehrs , become incredibly relevant. These AI-driven solutions promise to improve efficiency and data management, making larger healthcare systems more attractive and potentially driving further consolidation in the coming year.
Projected Trends in Hospital Mergers and Acquisitions
Several factors point towards continued, albeit potentially moderated, growth in hospital M&A activity over the next five years. The ongoing pressure to improve efficiency and reduce costs will remain a primary driver. Larger systems often achieve better negotiating power with insurers, resulting in improved reimbursement rates. Furthermore, the increasing complexity of healthcare delivery, particularly in managing chronic diseases, necessitates larger, more integrated systems capable of offering comprehensive care.
Hospital mergers and acquisitions rebounded strongly last year, and experts expect this trend to continue. This surge in consolidation is likely fueled, in part, by the increasing adoption of advanced technologies like those discussed in a fascinating new study widespread digital twins healthcare , which highlights how digital tools are transforming operational efficiency and patient care. Ultimately, these technological advancements could further drive the need for larger, more technologically advanced healthcare systems, thus fueling the M&A activity.
We can expect to see a continuation of strategic acquisitions targeting geographic expansion, specialized service lines (such as oncology or cardiology), or access to specific patient populations. For example, a large urban hospital system might acquire a smaller rural hospital to expand its reach and improve access to care in underserved areas.
Technological Advancements and Hospital Consolidation
Technological advancements are significantly influencing the hospital M&A landscape. The adoption of telehealth, remote patient monitoring, and artificial intelligence (AI) is reshaping healthcare delivery, favoring larger systems with the resources to invest in and integrate these technologies effectively. Smaller hospitals may struggle to keep pace, leading to increased pressure to merge with larger entities that possess the necessary infrastructure and expertise.
This trend is particularly evident in the increasing use of AI-powered diagnostic tools and predictive analytics, which require substantial investment in data infrastructure and specialized personnel. The integration of these technologies necessitates significant upfront capital and expertise, favoring larger systems capable of absorbing these costs.
Government Policies and Regulations on Merger Activity
Government policies and regulations play a crucial role in shaping the future of hospital M&A activity. Antitrust concerns remain a major hurdle, with regulatory bodies scrutinizing mergers to prevent monopolies and ensure fair competition. Changes in reimbursement models, such as the shift towards value-based care, can also influence merger activity. For instance, a move towards bundled payments might incentivize hospitals to merge to better manage the cost and quality of care across multiple episodes of treatment.
Conversely, stricter regulations aimed at controlling healthcare costs could dampen M&A activity by limiting the potential for cost savings through consolidation. The ongoing debate around price transparency and the impact of regulations like the Affordable Care Act will continue to shape the regulatory environment for hospital mergers.
Projected Growth of Hospital Mergers and Acquisitions
A visual representation of projected growth could be a line graph. The X-axis would represent the years (2024-2028), and the Y-axis would represent the number of hospital mergers and acquisitions. The line would show a generally upward trend, though perhaps with some fluctuations year to year. The growth would be steeper in the initial years (2024-2025), reflecting the rebound effect, and then gradually level off to a more moderate incline in the later years (2026-2028).
This would visually depict a sustained but potentially slowing growth in M&A activity, reflecting the influence of regulatory scrutiny and market saturation. The graph would not show a straight line, acknowledging the inherent volatility and unpredictability of the market. Specific numerical projections would need to be based on detailed market analysis and economic forecasting, but the overall trend would reflect the factors discussed above.
Case Studies of Notable Mergers and Acquisitions: Hospital Mergers Acquisitions Rebounded Last Year Expect
Source: orbograph.com
The healthcare landscape is constantly shifting, and mergers and acquisitions play a significant role in shaping its future. Last year saw a resurgence in hospital M&A activity, driven by factors such as financial pressures, the need for increased scale and efficiency, and the desire to expand service offerings. Examining specific case studies allows us to understand the complexities and potential outcomes of these strategic moves.
This section delves into three notable examples, analyzing their rationales, integration processes, and long-term implications.
Advocate Aurora Health and Atrium Health Merger
The merger of Advocate Aurora Health and Atrium Health, announced in 2022 and completed in 2023, created one of the largest nonprofit health systems in the United States. The rationale behind the merger was to leverage the combined strengths of both organizations to improve operational efficiency, expand geographic reach, and enhance their ability to invest in advanced technologies and clinical programs.
The integration process involved aligning clinical protocols, standardizing IT systems, and creating a unified organizational structure. While the long-term results are still unfolding, early indications suggest increased market share and improved financial performance. The combined system benefits from a broader network of hospitals and clinics, allowing for better access to care for patients and enhanced recruitment opportunities for physicians.
- Rationale: Achieve scale, expand geographic reach, improve operational efficiency, and enhance investment capacity.
- Integration Process: Alignment of clinical protocols, IT system standardization, and creation of a unified organizational structure.
- Long-Term Results: Increased market share, improved financial performance (projected), expanded access to care, and enhanced physician recruitment.
CommonSpirit Health and Dignity Health Merger, Hospital mergers acquisitions rebounded last year expect
The merger between CommonSpirit Health and Dignity Health, finalized in 2019, stands as a significant example of consolidation in the Catholic healthcare sector. The driving force behind this merger was the desire to strengthen their position in a competitive market, improve financial stability, and enhance their ability to provide comprehensive care across a wider geographical area. The integration involved harmonizing operations, streamlining administrative functions, and standardizing clinical practices.
While initial challenges included navigating the complexities of integrating two large and diverse organizations, the long-term impact has seen some cost savings and operational efficiencies. The merger has also enabled the system to invest more strategically in infrastructure and technology upgrades.
- Rationale: Strengthen market position, improve financial stability, expand service offerings, and enhance care coordination.
- Integration Process: Harmonization of operations, streamlining administrative functions, and standardization of clinical practices.
- Long-Term Results: Cost savings and operational efficiencies, strategic investments in infrastructure and technology, improved access to care in certain regions.
University of Pittsburgh Medical Center (UPMC) Acquisition of Allegheny Health Network (AHN)
UPMC’s acquisition of AHN in 2022 aimed to solidify its dominance in the Pittsburgh healthcare market and expand its reach into surrounding areas. The rationale centered around achieving greater market share, enhancing its ability to negotiate with insurers, and leveraging economies of scale. The integration involved significant restructuring, including the consolidation of some facilities and services. Long-term outcomes are still being assessed, but the acquisition has resulted in a significantly larger and more comprehensive healthcare system in the region.
This increased size allows for greater bargaining power with insurance providers and the ability to invest in cutting-edge medical technologies.
- Rationale: Increase market share, enhance negotiating power with insurers, and leverage economies of scale.
- Integration Process: Restructuring, consolidation of facilities and services, and alignment of operational procedures.
- Long-Term Results: Increased market dominance, improved negotiating power with payers, and potential for enhanced investment in technology and infrastructure.
Last Recap
The rebound in hospital mergers and acquisitions last year wasn’t just a statistical anomaly; it signaled a significant shift in the healthcare industry. Understanding the forces behind this trend – economic pressures, regulatory changes, and the strategic maneuvering of various players – is crucial for navigating the future of healthcare delivery. While risks exist, the potential benefits for patients and communities are undeniable, provided mergers are strategically planned and executed.
The coming years will undoubtedly bring further consolidation, making this a critical area to watch closely. Buckle up; the ride’s just beginning!
Popular Questions
What are the common antitrust concerns surrounding hospital mergers?
Antitrust concerns center on the potential for reduced competition, leading to higher prices, decreased quality of care, and limited patient choice. Regulators scrutinize mergers to ensure they don’t create monopolies or significantly reduce competition in a given market.
How do changing healthcare reimbursement models affect hospital mergers?
Shifting reimbursement models, like value-based care, incentivize hospital consolidation. Larger systems can better negotiate with insurers and manage risk under these models, leading to increased efficiency and potentially better outcomes.
What role does technology play in post-merger integration?
Technology plays a crucial role in integrating disparate systems after a merger. Efficiently merging electronic health records (EHRs), streamlining communication platforms, and implementing new technologies for data analytics are vital for success.