Hospitals Negative Margins High Labor Costs & Kaufman Hall
Hospitals negative margins constant high labor costs Kaufman Hall: This isn’t just another dry financial report; it’s a crisis unfolding in the heart of American healthcare. Hospitals are struggling, facing cripplingly high labor costs and consistently operating in the red. The consulting firm Kaufman Hall plays a key role in analyzing this mess, providing crucial data and insights into the factors driving these unsustainable losses.
We’ll delve into the specifics – from the escalating cost of staffing to the impact of government regulations – and explore potential solutions for a system on the brink.
This post will examine the complex interplay of factors contributing to the financial woes of US hospitals. We’ll look at the data provided by Kaufman Hall, explore the root causes of high labor costs, and discuss strategies hospitals are employing (or should be employing!) to navigate this challenging landscape. Get ready for a deep dive into the numbers, the challenges, and the potential paths forward for a healthier – and more financially stable – healthcare system.
Hospital Financial Pressures
The US healthcare system is facing a significant financial crisis, with many hospitals operating at negative margins. This isn’t a new problem, but the current economic climate, coupled with persistent staffing shortages and rising inflation, has exacerbated the situation, pushing many facilities to the brink. The confluence of these factors paints a bleak picture for the long-term viability of some hospitals, particularly those serving vulnerable populations.High Labor Costs and Their Impact on Hospital ProfitabilityHospitals are inherently labor-intensive.
The majority of their operating budget is dedicated to salaries, benefits, and associated payroll taxes for nurses, physicians, technicians, and administrative staff. Recent years have seen a dramatic increase in labor costs due to factors such as increased demand for healthcare professionals, competitive salaries offered by other industries, and the rising cost of benefits. This escalating expense directly impacts profitability, often exceeding the revenue generated from patient care, leading to negative margins.
The situation is further complicated by the increasing complexity of patient care, requiring more specialized and highly trained staff.Cost-Cutting Measures Implemented by HospitalsFaced with shrinking margins, hospitals are aggressively pursuing cost-cutting measures. These strategies range from streamlining administrative processes and negotiating better rates with suppliers to implementing more drastic measures such as reducing staff through attrition, delaying capital investments, and even closing underperforming departments or entire facilities.
Some hospitals are exploring innovative models of care, such as telehealth and outpatient services, to reduce reliance on expensive inpatient stays. For example, many hospitals are actively investing in automation to reduce administrative overhead and improve efficiency in tasks such as billing and scheduling. Others are consolidating services or merging with larger systems to achieve economies of scale and leverage greater bargaining power with suppliers.Hospital Operating Margins: A Regional ComparisonThe financial health of hospitals varies significantly across regions and systems.
Factors such as payer mix (the proportion of patients with private insurance versus government programs like Medicare and Medicaid), the prevalence of chronic diseases, and local economic conditions all play a role. The following table provides a hypothetical comparison, illustrating the range of operating margins:
| Hospital System | Region | Operating Margin (%) | Notes |
|---|---|---|---|
| System A | Northeast | -2.5 | High labor costs, significant government payer mix |
| System B | Southeast | 1.0 | Stronger private payer mix, lower labor costs |
| System C | Midwest | -1.0 | Rural hospitals facing significant challenges |
| System D | West Coast | 2.0 | High patient volume, diverse payer mix |
The Role of Kaufman Hall

Source: fastcompany.com
Kaufman Hall’s reports consistently highlight hospitals struggling with negative margins, largely due to constant high labor costs. Finding solutions is critical, and a recent study suggests a potential game-changer: check out this fascinating research on study widespread digital twins healthcare for innovative cost-saving strategies. Perhaps widespread adoption of digital twins could offer hospitals a much-needed pathway to improved financial health and address those persistent labor cost pressures.
Kaufman Hall is a leading healthcare consulting firm that plays a crucial role in helping hospitals navigate the complex financial landscape. They provide data-driven insights and strategic guidance to improve operational efficiency, enhance financial performance, and ultimately ensure the long-term sustainability of healthcare organizations. Their expertise is particularly valuable in the current climate of shrinking margins and escalating labor costs.Kaufman Hall employs a multifaceted approach to assess hospital financial health.
This involves a combination of rigorous data analysis, sophisticated modeling techniques, and a deep understanding of the healthcare industry’s regulatory and market dynamics. They leverage proprietary databases and benchmarking tools to compare a hospital’s performance against its peers, identifying areas of strength and weakness. This comprehensive analysis allows them to develop tailored strategies to address specific financial challenges.
Kaufman Hall’s Methodologies for Assessing Hospital Financial Health
Kaufman Hall utilizes several key methodologies to assess hospital financial health. These include financial modeling, which projects future financial performance based on various scenarios and assumptions. Benchmarking, a core component of their analysis, compares a hospital’s key performance indicators (KPIs) against those of similar organizations, revealing areas for improvement. Cost accounting methodologies are used to identify and analyze cost drivers within the hospital, pinpointing areas for potential cost reduction.
Finally, strategic planning services assist hospitals in developing long-term financial strategies that align with their overall mission and goals. These strategies often incorporate considerations of market trends, regulatory changes, and technological advancements.
Examples of Kaufman Hall Reports and Publications
Kaufman Hall regularly publishes reports and articles on various aspects of hospital finance, including margins and labor costs. While specific reports are often client-specific and not publicly available, their publicly accessible resources and publications frequently address trends in hospital profitability and the impact of rising labor costs. For example, their research often highlights the widening gap between hospital revenue and expenses, emphasizing the need for proactive cost management and revenue cycle optimization.
They might detail the impact of specific reimbursement changes or regulatory shifts on hospital margins, providing valuable context for understanding financial challenges. Their publications often showcase case studies illustrating how hospitals have successfully addressed financial pressures, often focusing on successful strategies related to labor cost management and workforce optimization.
Hypothetical Scenario: Kaufman Hall’s Impact on Hospital Financial Improvement
Imagine a hypothetical community hospital, “Hopewell Hospital,” struggling with consistently negative margins due to high labor costs. Hopewell Hospital engages Kaufman Hall for a comprehensive financial assessment. Kaufman Hall’s analysis reveals that Hopewell’s labor costs are significantly higher than those of comparable hospitals due to inefficient staffing patterns and a lack of standardized workflows. Further analysis identifies opportunities for streamlining processes, negotiating better contracts with staffing agencies, and implementing technology to improve efficiency.
Based on Kaufman Hall’s recommendations, Hopewell Hospital implements a new staffing model, optimizes its scheduling software, and invests in telehealth technologies to reduce the need for on-site personnel. The result is a significant reduction in labor costs, leading to improved margins and increased financial stability. This scenario illustrates how Kaufman Hall’s insights can translate into tangible improvements in a hospital’s financial health.
Labor Cost Drivers in Hospitals
Persistently high labor costs are a major challenge facing hospitals today, significantly impacting their financial stability and ability to provide quality care. Understanding the contributing factors is crucial for developing effective strategies to manage these expenses. This section delves into the key drivers of these costs, comparing different hospital settings and providing a breakdown of labor costs across various staff categories.
Several interconnected factors contribute to the persistently high labor costs in hospitals. The complexity of healthcare necessitates a highly skilled workforce, including physicians, nurses, technicians, and support staff, each requiring specialized training and education. This specialized training translates into higher salaries compared to other industries. Furthermore, the demanding nature of hospital work, often involving long hours, stressful situations, and emotional toll, necessitates competitive compensation packages to attract and retain qualified personnel.
Kaufman Hall’s reports consistently highlight hospitals struggling with negative margins, largely due to constant high labor costs. One potential solution lies in automating administrative tasks, and I was fascinated to read about how Nuance integrates generative AI scribe with Epic EHRs , which could significantly reduce the burden on already stretched hospital staff. This kind of technological advancement could be a game-changer in helping hospitals address their persistent financial challenges.
Rising healthcare insurance premiums, a significant portion of labor costs, also play a role. Finally, regulatory requirements and compliance mandates often increase administrative overhead and add to labor costs.
Labor Costs in Different Hospital Settings
Labor costs vary considerably between rural and urban hospitals. Urban hospitals, generally larger and located in areas with higher population densities and higher costs of living, tend to have higher labor costs. They often face greater competition for skilled professionals, leading to higher salaries and benefits packages to attract and retain talent. Rural hospitals, on the other hand, often struggle with workforce shortages, making it difficult to attract and retain qualified staff, yet they may offer lower salaries due to lower cost of living.
This can create a paradox where despite lower pay, rural hospitals may face higher labor costs per patient due to increased reliance on temporary or agency staffing to fill vacancies. The availability of specialized services also impacts costs; urban hospitals with a broader range of specialized services will often have a more diverse and higher-paid workforce.
Categorization of Hospital Staff by Labor Cost Contribution
To understand the distribution of labor costs, it’s helpful to categorize hospital staff based on their contribution to overall expenses. The following table provides a simplified overview, recognizing that the exact proportions will vary significantly between hospitals.
| Staff Category | Approximate Percentage of Total Labor Costs | Key Cost Drivers | Cost Mitigation Strategies |
|---|---|---|---|
| Nursing Staff (RNs, LPNs, CNAs) | 40-50% | High demand, specialized skills, shift differentials, overtime | Improved staffing models, technology integration, workforce retention programs |
| Physicians | 20-30% | High salaries, specialized training, on-call responsibilities | Negotiating contracts, optimizing physician scheduling, employing mid-level providers |
| Support Staff (Technicians, Administrative, etc.) | 20-25% | Varying skill levels, benefits costs, overtime | Streamlining processes, outsourcing non-core functions, investing in technology |
| Management & Administration | 10-15% | Salaries, benefits, regulatory compliance costs | Efficiency improvements, technology adoption, centralized services |
Labor Costs as a Percentage of Total Hospital Expenses
Labor costs typically represent the largest single expense for hospitals, often exceeding 50% of total operating expenses. This percentage can fluctuate based on hospital size, location, service offerings, and overall market conditions. The following table illustrates a potential breakdown, again acknowledging significant variation across institutions.
| Expense Category | Percentage of Total Hospital Expenses |
|---|---|
| Labor Costs | 55-65% |
| Supplies & Pharmaceuticals | 15-20% |
| Capital Expenditures | 5-10% |
| Other Operating Expenses | 10-15% |
Strategies for Improving Hospital Profitability
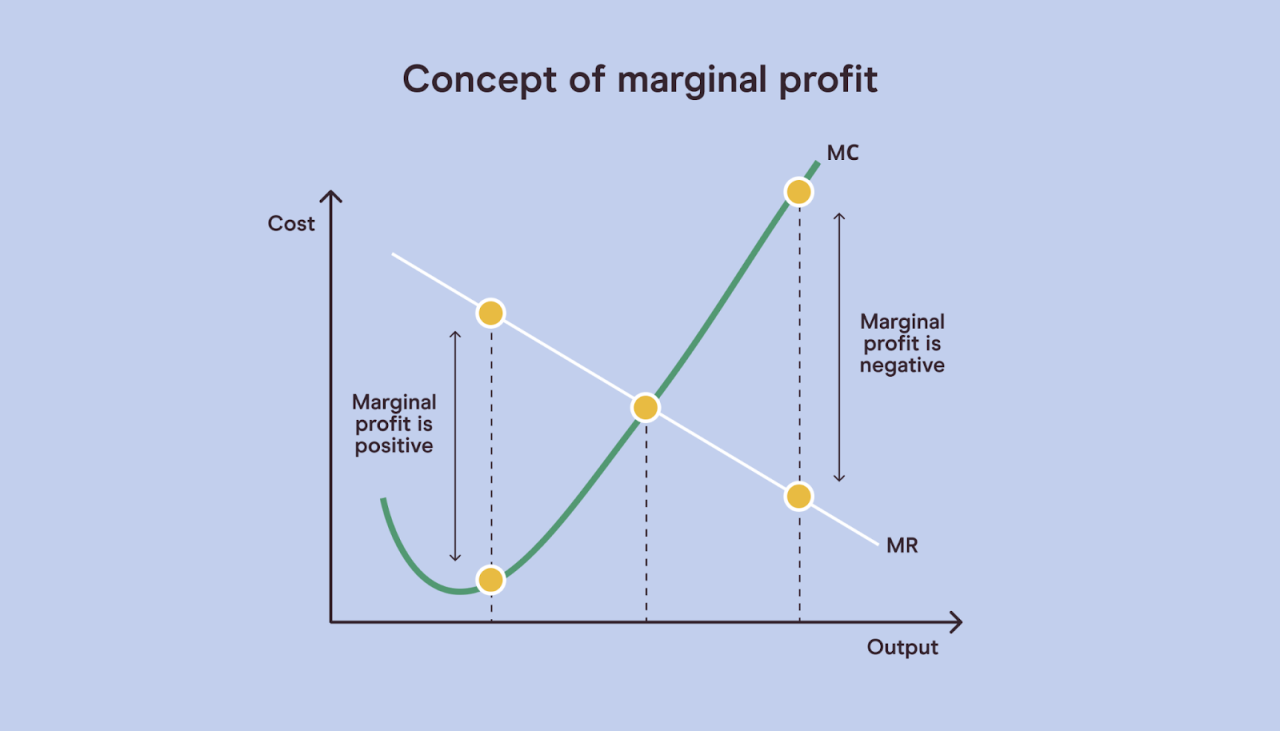
Hospitals across the nation are grappling with shrinking margins, largely driven by escalating labor costs. Addressing this challenge requires a multifaceted approach that balances cost reduction with the imperative to maintain high-quality patient care. Strategies must focus on improving efficiency, optimizing resource allocation, and exploring innovative models of care delivery.
Reducing Labor Costs Without Compromising Quality
Effectively reducing labor costs necessitates a strategic shift, not simply slashing wages or staff. One key strategy is to optimize staffing models through advanced workforce management tools that predict fluctuations in patient volume and adjust staffing levels accordingly. This prevents overstaffing during slow periods while ensuring adequate coverage during peak demand. Another approach involves investing in technology that automates tasks, freeing up staff to focus on higher-value activities like direct patient care.
For example, implementing electronic health records (EHRs) can streamline administrative tasks, reducing the time nurses and other clinicians spend on paperwork. Finally, focusing on employee retention through competitive compensation and benefits packages can minimize the costs associated with high turnover and recruitment. Reduced turnover leads to a more experienced and efficient workforce, improving overall quality of care.
Impact of Cost-Reduction Strategies
Implementing these strategies can yield significant financial improvements. For instance, a hospital system in California, by optimizing its scheduling software and improving its nurse-to-patient ratios based on real-time data, reduced overtime costs by 15% within a year. Simultaneously, patient satisfaction scores remained stable, demonstrating that cost reduction doesn’t have to come at the expense of quality. Investing in automation, like robotic process automation (RPA) for billing and coding, can free up administrative staff, reducing payroll expenses while improving accuracy and efficiency.
The potential return on investment (ROI) for such technologies can be substantial, typically ranging from 20% to 50% within three to five years, depending on the scale and complexity of implementation.
Innovative Approaches to Improve Efficiency and Reduce Expenses
The healthcare industry is embracing innovation to enhance efficiency and curtail expenses.
- Telehealth: Expanding telehealth services can significantly reduce the need for in-person visits, lowering overhead costs associated with physical infrastructure and staffing. This model is particularly effective for routine follow-up appointments and chronic disease management.
- Value-Based Care Models: Shifting from fee-for-service to value-based care incentivizes hospitals to focus on improving patient outcomes while controlling costs. This approach rewards hospitals for achieving better health outcomes rather than simply performing more procedures.
- Data Analytics and Predictive Modeling: Leveraging data analytics to identify trends and predict future needs allows hospitals to optimize resource allocation, reducing waste and improving operational efficiency. This can lead to better inventory management, more efficient scheduling, and reduced readmission rates.
- Lean Management Principles: Implementing lean management principles, focusing on eliminating waste and streamlining processes, can improve efficiency throughout the hospital system. This involves identifying and eliminating unnecessary steps in workflows, improving communication, and empowering staff to identify and solve problems.
Outsourcing Certain Hospital Services
Outsourcing non-core functions, such as laundry services, food services, or medical transcription, can offer cost savings by leveraging the economies of scale of specialized providers.
- Benefits: Reduced labor costs, improved efficiency, and access to specialized expertise are key benefits. Outsourcing can free up internal resources to focus on core competencies, like direct patient care.
- Drawbacks: Potential loss of control over service quality, security concerns regarding patient data, and potential negative impacts on employee morale are potential drawbacks. Careful selection of outsourcing partners and robust contracts are crucial to mitigate these risks.
The Impact of Government Regulations
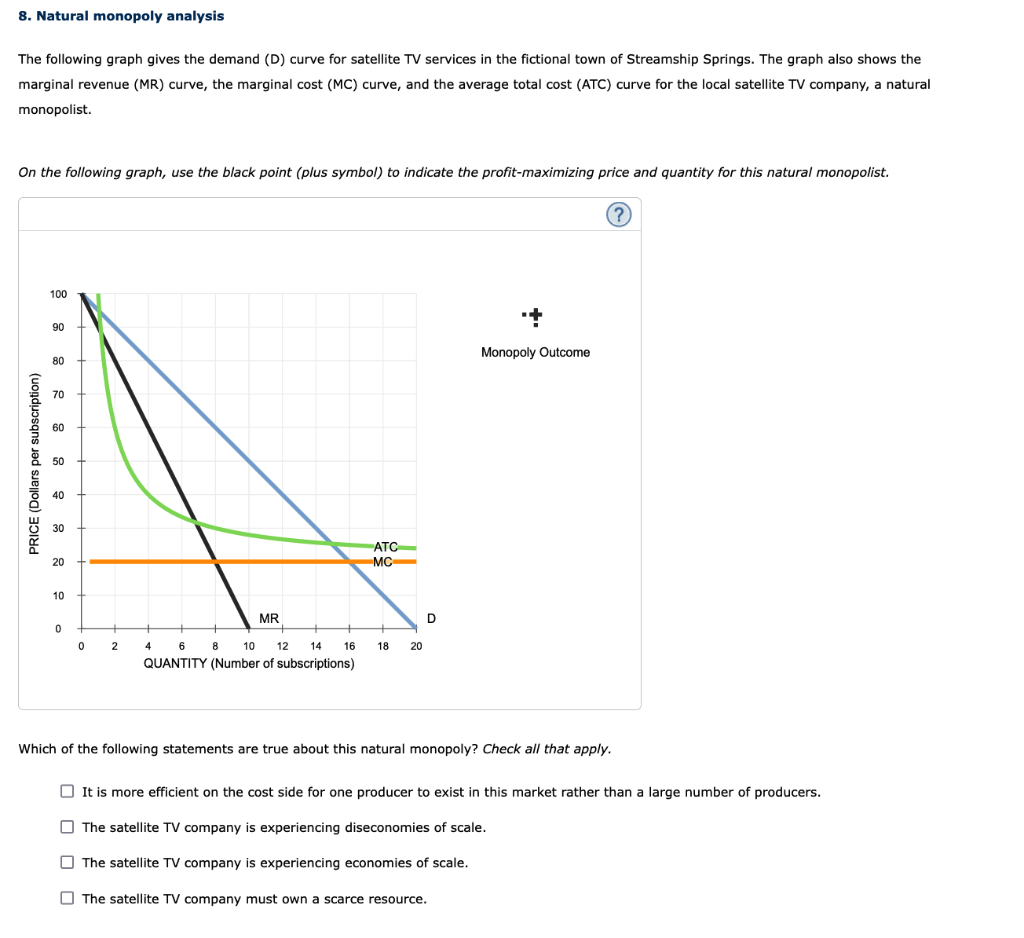
Source: cheggcdn.com
Government regulations and reimbursement policies significantly impact hospital margins, often acting as a double-edged sword. While designed to ensure quality care and equitable access, these policies can create financial strain for healthcare providers, particularly in the context of rising labor costs and other operational expenses. Understanding the intricacies of these regulations is crucial for hospitals to maintain financial stability and continue providing essential services.Government regulations influence hospital profitability primarily through their control over reimbursement rates.
Medicare and Medicaid, the two largest government-funded healthcare programs in the United States, set payment rates for services provided to their beneficiaries. These rates are often based on formulas that may not fully reflect the actual cost of providing care, leading to potential losses for hospitals. The complexities of these reimbursement systems, coupled with the increasing number of patients relying on these programs, significantly influence a hospital’s bottom line.
Medicare and Medicaid Payment Impacts on Hospital Profitability
Medicare and Medicaid payments are a critical revenue source for many hospitals, particularly those serving large populations of elderly or low-income individuals. However, the payment rates established by these programs frequently lag behind the actual cost of care. This gap, often referred to as the “cost-to-charge ratio,” can lead to significant financial challenges for hospitals, especially those with high proportions of Medicare and Medicaid patients.
For example, a hospital with a high percentage of Medicare patients might struggle to cover its operating costs if Medicare reimbursement rates do not adequately compensate for the expense of providing care to this population. This often necessitates cost-cutting measures or adjustments to service offerings to maintain profitability. The constant negotiation and adjustment required to manage reimbursements under these programs adds significant administrative burden, further impacting hospital finances.
The Impact of Different Healthcare Reform Proposals on Hospital Finances, Hospitals negative margins constant high labor costs kaufman hall
Different healthcare reform proposals have varying impacts on hospital finances. Proposals that emphasize cost containment through measures such as bundled payments or value-based care can potentially reduce hospital revenue if they are not adequately compensated for the complexities of managing these new payment models. Conversely, proposals that expand coverage or increase reimbursement rates can improve hospital finances but may also lead to increased demand for services, requiring hospitals to adapt their infrastructure and staffing levels.
The Affordable Care Act (ACA), for instance, initially expanded coverage, leading to an increase in patients, but the associated reimbursement rates didn’t always fully cover the costs of care, presenting a complex financial equation for hospitals to navigate. Proposals aimed at reducing administrative burdens through simplification of billing and coding processes can positively impact hospital profitability by freeing up resources and reducing administrative costs.
Successful Strategies for Navigating Regulatory Challenges
Hospitals have employed several successful strategies to navigate regulatory challenges and maintain financial stability. These include: improving operational efficiency to reduce costs, diversifying revenue streams through services such as outpatient clinics or telehealth, and engaging in effective advocacy to influence reimbursement policies. Strategic partnerships with other healthcare providers, such as physician groups or post-acute care facilities, can also enhance efficiency and create new revenue opportunities.
Kaufman Hall’s reports consistently highlight the crushing weight of high labor costs on hospital margins, often pushing them into the red. This is especially true in rural areas, where staffing shortages are acute, as highlighted by this insightful article on Rural Hospitals Labor Delivery & the challenges they face. The struggles detailed there only underscore the broader issue: the unsustainable financial pressures driving many hospitals towards negative margins.
Robust data analytics and cost accounting are also critical for identifying areas for improvement and making informed decisions about resource allocation. For instance, some hospitals have implemented advanced technologies to streamline processes, reduce waste, and improve patient outcomes, leading to both cost savings and enhanced quality of care. Successful navigation of regulatory challenges often hinges on a proactive approach, continuous adaptation, and a commitment to innovation.
Future Outlook for Hospital Finances
The current financial predicament facing hospitals is undeniably severe. Persistent negative margins, coupled with escalating labor costs and a tightening economic climate, paint a challenging picture for the future. Understanding the potential trajectories of hospital finances is crucial for stakeholders, from administrators and clinicians to policymakers and patients. The following analysis explores likely trends, long-term implications, and potential solutions to navigate this turbulent landscape.
Potential Future Trends in Hospital Finances
The coming years will likely witness a continuation of the current financial strains. Labor shortages will remain a significant pressure point, driving up wages and potentially impacting the quality and availability of care. Economic downturns, whether mild recessions or more severe crises, will further reduce patient volumes and potentially limit government funding. Increased regulatory burdens and the rising cost of medical technology will add to the existing financial pressures.
For example, the ongoing nursing shortage, exacerbated by burnout and aging demographics, is already forcing hospitals to offer higher salaries and benefits, squeezing their margins further. Simultaneously, inflation’s impact on supplies and operational costs adds another layer of complexity.
Long-Term Implications of Persistent Negative Margins
Sustained negative margins have dire consequences for hospital systems. Reduced access to capital for reinvestment in facilities and technology will lead to outdated equipment and infrastructure, impacting the quality of care. The ability to recruit and retain top talent will diminish, further exacerbating the labor shortage. This could result in service cuts, hospital closures, and ultimately, compromised patient care.
For instance, a hospital system consistently operating at a loss might be forced to delay upgrades to its imaging equipment, leading to diagnostic delays and potentially poorer patient outcomes. Moreover, inability to offer competitive salaries may lead to experienced nurses and physicians leaving for better opportunities, reducing the quality and availability of care.
Potential Solutions to Address the Challenges Facing Hospital Finances
Addressing the multifaceted financial crisis requires a multi-pronged approach. Hospitals must explore innovative care delivery models, such as telehealth and value-based care, to improve efficiency and reduce costs. Negotiating better contracts with insurers and pharmaceutical companies is crucial. Investing in technology to automate administrative tasks and improve operational efficiency can also yield significant savings. Furthermore, advocating for policy changes that address workforce shortages and increase government funding for healthcare is essential.
For example, implementing telehealth platforms can reduce the need for expensive in-person visits, while negotiating bundled payment arrangements with insurers can incentivize cost-effective care delivery.
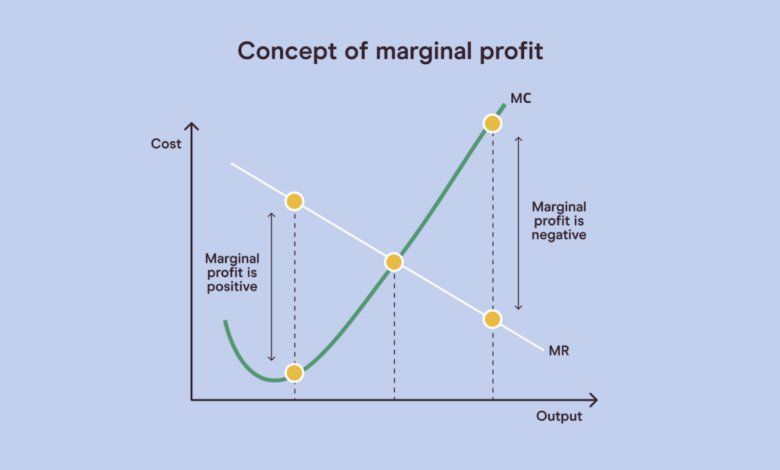
Projected Trajectory of Hospital Margins
[Imagine a line graph. The X-axis represents the years from 2024 to 2034. The Y-axis represents hospital operating margins, ranging from -5% to +5%. The line starts at approximately -2% in 2024, dips slightly lower to around -3% in 2026, remains relatively flat and negative until 2029, before showing a very gradual upward trend, reaching approximately -1% by 2034. The graph illustrates a slow and gradual improvement, highlighting the persistent challenges faced by hospitals in achieving profitability within the projected timeframe.
The graph’s overall shape reflects a persistent struggle to reach positive margins, with only a minor improvement expected over the next decade, even with the implementation of cost-saving measures and improved operational efficiencies. The slow upward trend reflects the time lag between implementing new strategies and seeing a significant impact on the bottom line. This projection assumes a moderate economic environment and a gradual resolution of labor shortages.
A more severe economic downturn or a failure to address labor issues could result in a more pessimistic trajectory.]
Final Summary
Source: paretolabs.com
The financial health of US hospitals is undeniably precarious, a situation exacerbated by persistent negative margins and skyrocketing labor costs. Kaufman Hall’s analyses offer a stark picture, highlighting the urgent need for systemic change. While cost-cutting measures are necessary, a holistic approach is required, addressing issues like fair compensation for healthcare workers, smarter resource allocation, and more equitable reimbursement policies.
The future of patient care hinges on finding sustainable solutions – and quickly.
Questions and Answers: Hospitals Negative Margins Constant High Labor Costs Kaufman Hall
What specific strategies are hospitals using to attract and retain staff in the face of labor shortages?
Hospitals are employing various strategies including increased wages and benefits, improved work-life balance initiatives, sign-on bonuses, and investment in employee development programs.
How do differences in patient populations affect hospital profitability?
Hospitals serving a higher proportion of uninsured or underinsured patients often face lower profitability due to reduced reimbursement rates.
What role does technology play in addressing hospital cost issues?
Technology can improve efficiency through automation, telehealth, and data analytics, leading to cost savings and improved care.