Impact of Environmental Toxins on Womens Reproductive Health
Impact of environmental toxins on womens reproductive health – Impact of environmental toxins on women’s reproductive health is a critical issue, often overlooked but deeply impactful. We’re surrounded by potential threats – from the pesticides on our produce to the heavy metals in our water – and these toxins can silently wreak havoc on our bodies’ ability to conceive, carry a pregnancy to term, and raise healthy children.
This post delves into the science behind this concerning reality, exploring the various ways environmental toxins affect fertility, pregnancy, and long-term health.
We’ll look at specific toxins, their sources, and how they disrupt the intricate processes of reproduction. We’ll also explore the disproportionate impact on vulnerable populations and discuss practical steps we can take to minimize our exposure and protect our reproductive health. This isn’t just about statistics; it’s about empowering ourselves with knowledge to make informed choices for a healthier future.
Types of Environmental Toxins Affecting Reproductive Health: Impact Of Environmental Toxins On Womens Reproductive Health
Environmental toxins pose a significant threat to women’s reproductive health, impacting fertility, pregnancy outcomes, and overall reproductive well-being. Exposure to these toxins can occur through various pathways, including air, water, food, and occupational settings. Understanding the types of toxins and their mechanisms of action is crucial for implementing effective preventative measures and mitigating their harmful effects.
Several classes of environmental toxins are known to disrupt the intricate processes involved in female reproduction. These toxins work through various mechanisms, often interfering with hormonal signaling, DNA replication, and cellular processes essential for healthy egg development, fertilization, implantation, and fetal development. The impact can be subtle and difficult to detect, or it can manifest as overt reproductive problems.
Heavy Metals, Impact of environmental toxins on womens reproductive health
Heavy metals, such as lead, mercury, and cadmium, are persistent environmental pollutants that can accumulate in the body over time. Lead exposure, for instance, can occur through contaminated water, paint, or soil. Mercury exposure can result from consumption of contaminated fish, while cadmium exposure is often linked to industrial pollution and cigarette smoke. These metals interfere with reproductive processes by disrupting hormone production, damaging DNA, and increasing oxidative stress, ultimately impacting fertility, increasing the risk of miscarriage, and affecting fetal development.
So many things impact women’s reproductive health, and it’s scary to think about the long-term effects of environmental toxins. We often focus on immediate health concerns, but it’s crucial to remember that these toxins can contribute to long-term health problems like cardiovascular disease. For example, understanding the connection between these toxins and increased risk factors, like those outlined in this article on risk factors that make stroke more dangerous , is vital.
Ultimately, reducing our exposure to these environmental hazards is crucial for protecting women’s overall health and reproductive well-being.
Lead, in particular, has been linked to reduced fertility, preterm birth, and low birth weight.
Pesticides
Pesticides, designed to kill pests, are widely used in agriculture and other settings. Exposure to organochlorine pesticides (like DDT) and organophosphate pesticides (like chlorpyrifos) is linked to numerous reproductive health issues. These chemicals can mimic or block hormones, interfering with endocrine function and disrupting ovulation, implantation, and fetal development. Studies have shown associations between pesticide exposure and increased risks of miscarriage, birth defects, and reduced fertility.
For example, exposure to DDT has been linked to an increased risk of endometriosis.
Endocrine-Disrupting Chemicals (EDCs)
EDCs are a diverse group of chemicals that interfere with the endocrine system, disrupting the production, transport, metabolism, binding, action, or elimination of natural hormones. Examples include bisphenol A (BPA), found in plastics and epoxy resins, and phthalates, used in many consumer products. These chemicals can mimic estrogen or other hormones, leading to hormonal imbalances that affect various aspects of reproductive health, including menstrual cycle irregularities, reduced fertility, and increased risk of certain cancers.
BPA exposure, for instance, has been linked to problems with ovulation and implantation.
| Toxin | Source | Mechanism of Action | Reproductive Health Impact |
|---|---|---|---|
| Lead | Contaminated water, paint, soil | Disrupts hormone production, damages DNA, increases oxidative stress | Reduced fertility, miscarriage, preterm birth, low birth weight |
| Mercury | Contaminated fish | Neurotoxicity, disrupts hormone signaling | Neurodevelopmental problems in offspring, reduced fertility |
| Cadmium | Industrial pollution, cigarette smoke | Oxidative stress, disrupts hormone balance | Reduced fertility, menstrual irregularities |
| DDT (Organochlorine Pesticide) | Agricultural use (now largely banned), environmental persistence | Endocrine disruption, mimics estrogen | Increased risk of endometriosis, reduced fertility, reproductive cancers |
| BPA (Bisphenol A) | Plastics, epoxy resins | Mimics estrogen, disrupts hormone signaling | Ovulation problems, implantation failure, reduced fertility |
| Phthalates | Plastics, cosmetics, personal care products | Endocrine disruption, affects hormone production | Menstrual irregularities, reduced sperm quality (in males), developmental problems in offspring |
Impact on Fertility and Conception
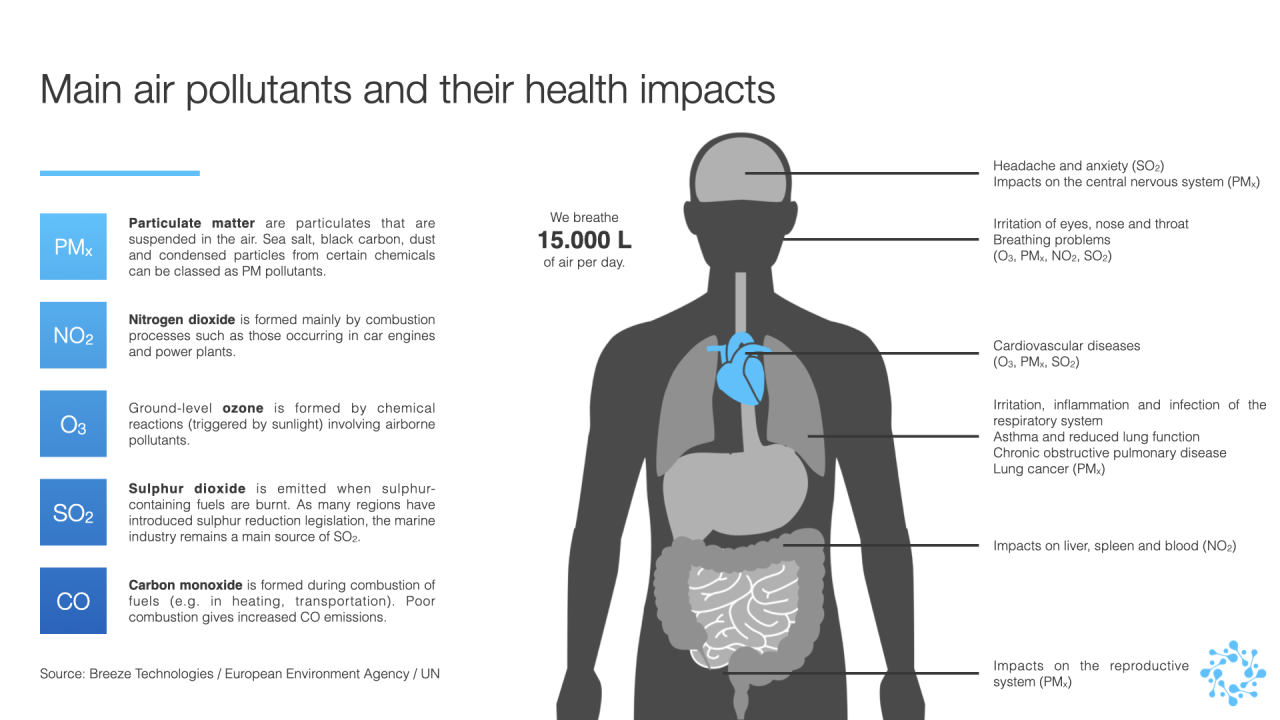
Source: breeze-technologies.de
Environmental toxins pose a significant threat to human reproductive health, impacting fertility and the ability to conceive. Exposure to these toxins can disrupt the intricate hormonal balance and cellular processes crucial for successful reproduction in both men and women. The effects can range from subtle reductions in fertility to complete infertility, highlighting the urgent need for understanding and mitigating these environmental risks.Exposure to environmental toxins can significantly affect ovarian reserve and egg quality, impacting a woman’s fertility.
These toxins can interfere with the delicate processes of follicle development, oocyte maturation, and ovulation. The resulting damage can lead to reduced numbers of healthy eggs available for fertilization, a decreased chance of conception, and an increased risk of early menopause.
Ovarian Reserve and Egg Quality
Several studies have linked exposure to endocrine-disrupting chemicals (EDCs), such as phthalates and bisphenol A (BPA), to diminished ovarian reserve and poorer egg quality. These chemicals mimic or interfere with the body’s natural hormones, disrupting the delicate hormonal cascade necessary for proper ovarian function. Animal studies have demonstrated a direct correlation between exposure to EDCs and reduced follicle counts, leading to premature ovarian aging.
In humans, epidemiological studies have shown associations between exposure to certain pesticides and reduced ovarian reserve, although more research is needed to establish definitive causal relationships. For example, women living near agricultural areas with high pesticide use might show lower ovarian reserve compared to those in less exposed areas. This reduction in egg quality can manifest as increased rates of miscarriage or a higher likelihood of needing assisted reproductive technologies (ART) like in-vitro fertilization (IVF) to conceive.
Impact on Sperm Parameters
Environmental toxins also significantly impact male fertility by affecting sperm parameters. Exposure to heavy metals like lead and cadmium, as well as pesticides and industrial chemicals, has been associated with decreased sperm count, motility (the ability to move), and morphology (shape and structure). These toxins can induce oxidative stress, damaging sperm DNA and compromising its ability to fertilize an egg.
Furthermore, some toxins can disrupt the delicate hormonal balance crucial for spermatogenesis (sperm production), leading to lower sperm production overall. A study published in the journalEnvironmental Health Perspectives* demonstrated a significant association between exposure to certain pesticides and decreased sperm concentration and motility in agricultural workers. This reduction in sperm quality can result in male infertility or reduced chances of natural conception.
Implantation and Early Embryonic Development
The impact of environmental toxins extends beyond the production of gametes (sperm and eggs) to affect implantation and early embryonic development. Exposure to toxins during the peri-conceptional period (around the time of conception) can disrupt the intricate processes involved in implantation, the process by which the fertilized egg attaches to the uterine wall. Furthermore, toxins can interfere with early embryonic development, increasing the risk of miscarriage or birth defects.
Studies have shown that exposure to certain chemicals, such as dioxins and PCBs, can alter gene expression in the developing embryo, leading to developmental abnormalities. These effects can manifest as structural birth defects, cognitive impairment, or other health issues.
Correlation Between Environmental Toxin Exposure and Infertility Rates
Numerous studies have explored the correlation between environmental toxin exposure and infertility rates. While establishing direct causation remains challenging due to the complex interplay of factors influencing fertility, several studies suggest a strong association. For instance, increased rates of infertility have been observed in populations exposed to high levels of industrial pollutants or agricultural chemicals. These studies often utilize epidemiological approaches, comparing fertility rates in exposed and unexposed populations.
The observed correlations highlight the potential role of environmental toxins in contributing to the global rise in infertility rates. More research is needed to fully elucidate the mechanisms through which specific toxins affect fertility and to develop effective strategies for prevention and mitigation.
We’re constantly bombarded by environmental toxins, and their impact on women’s reproductive health is a serious concern. Many women are proactively addressing fertility challenges, like Karishma Mehta, who chose egg freezing; you can read more about her decision and the associated risks in this article: karishma mehta gets her eggs frozen know risks associated with egg freezing.
Ultimately, understanding both the environmental risks and the options available for preserving fertility is crucial for women’s health.
Effects on Pregnancy and Fetal Development
Exposure to environmental toxins during pregnancy poses significant risks to both the mother and the developing fetus. The consequences can be severe and long-lasting, impacting fetal growth, development, and ultimately, the child’s health throughout their life. Understanding these risks is crucial for implementing preventative measures and mitigating potential harm.The developing fetus is particularly vulnerable to environmental toxins due to its rapid growth and immature detoxification systems.
Many toxins can cross the placental barrier, directly exposing the fetus to harmful substances. This transplacental transfer allows chemicals to reach the fetus, impacting various aspects of its development, from organogenesis to neurological function. The severity of the effects depends on factors such as the type and amount of toxin, the timing of exposure, and the mother’s overall health.
Miscarriage, Preterm Birth, and Birth Defects
Exposure to environmental toxins during pregnancy is linked to an increased risk of adverse pregnancy outcomes, including miscarriage, preterm birth, and various birth defects. Miscarriage, the spontaneous loss of a pregnancy before the 20th week, can be triggered by several toxins that disrupt normal embryonic development. Preterm birth, the delivery of a baby before 37 weeks of gestation, is also associated with toxin exposure, leading to low birth weight and increased health complications for the newborn.
Birth defects, structural or functional abnormalities present at birth, are a serious concern, with many linked to environmental exposures.
Environmental toxins seriously impact women’s reproductive health, affecting fertility and pregnancy outcomes. Nourishing our bodies with the right foods is crucial, and understanding nutritional needs is key; check out this article on whether are women and men receptive of different types of food and game changing superfoods for women to help mitigate these effects. A healthy diet, rich in antioxidants and nutrients, can help support reproductive health in the face of environmental challenges.
Examples of Toxin-Induced Birth Defects
Several specific birth defects have been linked to exposure to particular environmental toxins. For instance, exposure to high levels of mercury, often through consumption of contaminated fish, can lead to neurological developmental delays and cerebral palsy. Exposure to alcohol during pregnancy is well-known to cause Fetal Alcohol Spectrum Disorders (FASDs), a range of physical, mental, and behavioral disabilities.
Exposure to certain pesticides, like DDT, has been associated with increased risks of neural tube defects like spina bifida. Lead exposure can cause developmental delays, learning disabilities, and behavioral problems.
Transplacental Transfer of Toxins
The placenta, while designed to protect the fetus, is not a perfect barrier. Many lipophilic (fat-soluble) toxins can readily cross the placenta, accumulating in fetal tissues and organs. This transplacental transfer can have profound effects on fetal development. The fetus’s developing organs are particularly susceptible during critical periods of organogenesis, when cells are rapidly dividing and differentiating.
Exposure to toxins during these sensitive periods can lead to irreversible damage. The impact of toxin exposure isn’t limited to the immediate effects; epigenetic changes induced by toxins can have long-term consequences, affecting gene expression and potentially impacting the child’s health later in life.
Effects of Toxins on Fetal Development
| Toxin | Stage of Fetal Development Affected | Potential Effects |
|---|---|---|
| Mercury | Neural development (throughout pregnancy) | Neurological damage, developmental delays, cerebral palsy |
| Lead | Various stages (particularly early development) | Developmental delays, learning disabilities, behavioral problems, reduced IQ |
| Polychlorinated biphenyls (PCBs) | Immune system, nervous system, endocrine system | Impaired immune function, neurological deficits, endocrine disruption |
| Pesticides (e.g., DDT) | Neural tube closure (early pregnancy) | Neural tube defects (spina bifida, anencephaly) |
| Alcohol | All stages of development | Fetal Alcohol Spectrum Disorders (FASDs), including physical, mental, and behavioral problems |
Impact on Postnatal Health and Development
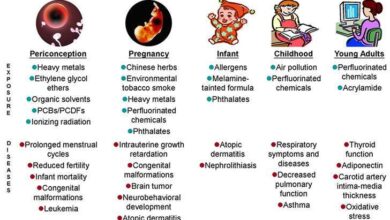
Source: mdpi-res.com
Prenatal exposure to environmental toxins can have profound and lasting consequences for a child’s health and development, extending far beyond the immediate postnatal period. The effects are complex and often subtle, making it challenging to isolate the impact of specific toxins from other contributing factors. However, a growing body of research highlights the significant role environmental toxins play in shaping a child’s future well-being.The consequences of prenatal toxin exposure are not limited to the immediate postnatal period; they can manifest throughout a child’s life, impacting various aspects of their physical and cognitive development.
Understanding these long-term effects is crucial for implementing preventative measures and developing effective interventions.
Long-Term Effects on Child Development, Including Neurodevelopmental Outcomes
Exposure to environmental toxins during pregnancy can significantly disrupt the delicate process of fetal brain development. This can lead to a range of neurodevelopmental outcomes, including intellectual disabilities, learning disorders, attention deficit hyperactivity disorder (ADHD), and autism spectrum disorder (ASD). For instance, studies have linked exposure to lead during pregnancy to lower IQ scores and behavioral problems in children.
Similarly, exposure to certain pesticides has been associated with an increased risk of ADHD. The severity of these effects often depends on the type and level of toxin exposure, as well as the individual’s genetic susceptibility. These developmental delays and disorders can have long-lasting implications for a child’s academic performance, social interactions, and overall quality of life.
Early intervention and supportive therapies are often necessary to mitigate these challenges.
Links Between Environmental Toxin Exposure and Reproductive Health Problems in Offspring
Emerging evidence suggests a potential link between prenatal exposure to environmental toxins and reproductive health problems in the offspring later in life. This connection may be particularly relevant for endocrine-disrupting chemicals (EDCs), which interfere with the body’s hormonal system. Exposure to EDCs during fetal development could alter the programming of the reproductive system, leading to problems such as infertility, irregular menstrual cycles, and endometriosis in females, and reduced sperm count and quality in males.
These effects might not become apparent until the offspring reach reproductive age, highlighting the long-term consequences of prenatal exposure. More research is needed to fully elucidate these complex relationships and identify specific toxins involved. However, the potential for transgenerational effects underscores the importance of minimizing exposure to environmental toxins during pregnancy.
The Role of Epigenetic Modifications in Mediating Long-Term Effects
Epigenetic modifications, changes in gene expression without altering the underlying DNA sequence, play a crucial role in mediating the long-term effects of environmental toxin exposure. Toxins can induce epigenetic changes, such as DNA methylation and histone modification, which can alter gene activity and influence the development and function of various organs and systems. These epigenetic alterations can be inherited across generations, meaning that the effects of prenatal toxin exposure can extend beyond the directly exposed individual to their offspring and even subsequent generations.
This transgenerational inheritance adds another layer of complexity to understanding the long-term consequences of environmental toxin exposure. Research into epigenetic mechanisms is crucial for developing strategies to prevent and mitigate the adverse health effects of environmental toxins.
Potential Postnatal Health Problems Related to Prenatal Toxin Exposure
The impact of prenatal toxin exposure extends beyond neurodevelopmental issues and reproductive health. A range of postnatal health problems have been linked to such exposure.
- Respiratory problems: Asthma, allergies, and other respiratory illnesses.
- Immune system dysfunction: Increased susceptibility to infections and autoimmune diseases.
- Cardiovascular problems: Increased risk of heart defects and hypertension.
- Metabolic disorders: Obesity, type 2 diabetes, and metabolic syndrome.
- Cancers: Increased risk of certain types of cancers later in life.
- Neurological disorders: Autism spectrum disorder, ADHD, intellectual disability.
- Behavioral problems: Aggression, anxiety, and depression.
It is important to note that the manifestation and severity of these problems can vary significantly depending on factors such as the type and level of toxin exposure, the timing of exposure during pregnancy, genetic predisposition, and environmental factors post-birth. Early detection and intervention are essential to minimize the long-term impact of these health issues.
Protective Measures and Mitigation Strategies
Protecting reproductive health from the damaging effects of environmental toxins requires a multi-pronged approach encompassing individual lifestyle choices, robust public health initiatives, and access to effective medical interventions. By understanding and implementing these strategies, we can significantly reduce exposure and mitigate the negative consequences on fertility, pregnancy, and postnatal health.
Lifestyle Modifications to Reduce Toxin Exposure
Minimizing exposure to environmental toxins begins at home and extends to our daily routines. Simple changes can make a significant difference in protecting reproductive health. These changes are particularly crucial for women of childbearing age and pregnant individuals.
- Prioritize organic food: Choosing organic produce reduces exposure to pesticides and herbicides, known endocrine disruptors. Studies have linked higher pesticide exposure to reduced fertility and increased risk of pregnancy complications.
- Filter your water: Tap water may contain contaminants like lead and chlorine. Using a high-quality water filter can significantly reduce exposure to these harmful substances.
- Limit exposure to personal care products containing endocrine disruptors: Many cosmetics, lotions, and shampoos contain phthalates and parabens, which are suspected endocrine disruptors. Opting for products labeled “phthalate-free” and “paraben-free” is a crucial step.
- Reduce exposure to household cleaning products: Many conventional cleaning products contain volatile organic compounds (VOCs) that can be harmful to reproductive health. Switching to eco-friendly, plant-based cleaning products minimizes exposure.
- Air purification: Using air purifiers with HEPA filters can significantly reduce indoor air pollution from dust, pollen, and other airborne toxins.
The Role of Public Health Policies
Effective public health policies are essential for creating a safer environment and protecting reproductive health on a larger scale. These policies should focus on prevention and regulation.
- Stricter regulations on industrial emissions: Regulations limiting the release of harmful chemicals into the air and water are critical. Examples include stricter emission standards for factories and power plants, as well as regulations on the use and disposal of hazardous waste.
- Improved waste management: Proper waste disposal and recycling programs are crucial for preventing contamination of soil and water sources. This minimizes exposure to heavy metals and other toxins often found in landfills.
- Public awareness campaigns: Educating the public about the risks of environmental toxins and providing clear guidance on how to minimize exposure is vital. This includes disseminating information on safe food choices, reducing household chemical use, and proper waste disposal.
- Monitoring and research: Continuous monitoring of environmental toxins and ongoing research to identify emerging threats are necessary for effective policymaking. This data informs the development and implementation of preventive measures.
Medical Interventions and Treatments
While prevention is the most effective strategy, medical interventions can help manage the adverse effects of environmental toxin exposure.
- Chelation therapy: This treatment can help remove heavy metals, such as lead and mercury, from the body. It is often used in cases of severe heavy metal poisoning.
- Supportive care: For conditions like infertility or pregnancy complications linked to toxin exposure, supportive care may include nutritional counseling, hormone therapy, or assisted reproductive technologies (ART).
- Early detection and intervention: Regular check-ups and prenatal care are essential for early detection of any adverse effects and timely intervention. This allows for early management and potentially improved outcomes.
Visual Representation of Strategies for Reducing Exposure
Imagine a layered diagram. The outermost layer represents the environment – air, water, and soil. Arrows point inwards, representing pathways of toxin exposure: contaminated food, water, air, and household products. The next layer depicts individual lifestyle choices: organic food selection, water filtration, eco-friendly cleaning products, and limiting exposure to personal care products containing endocrine disruptors. This layer is depicted as a protective shield partially blocking the arrows.
The innermost layer represents public health policies: stricter regulations on industrial emissions, improved waste management, and public awareness campaigns. This innermost layer acts as a further barrier, reducing the overall flow of toxins. Finally, at the very center, is the individual, well-protected from the majority of toxins due to the combined efforts of personal choices and public health measures.
The diagram emphasizes the synergistic effect of individual actions and broader societal interventions in mitigating exposure and promoting reproductive health.
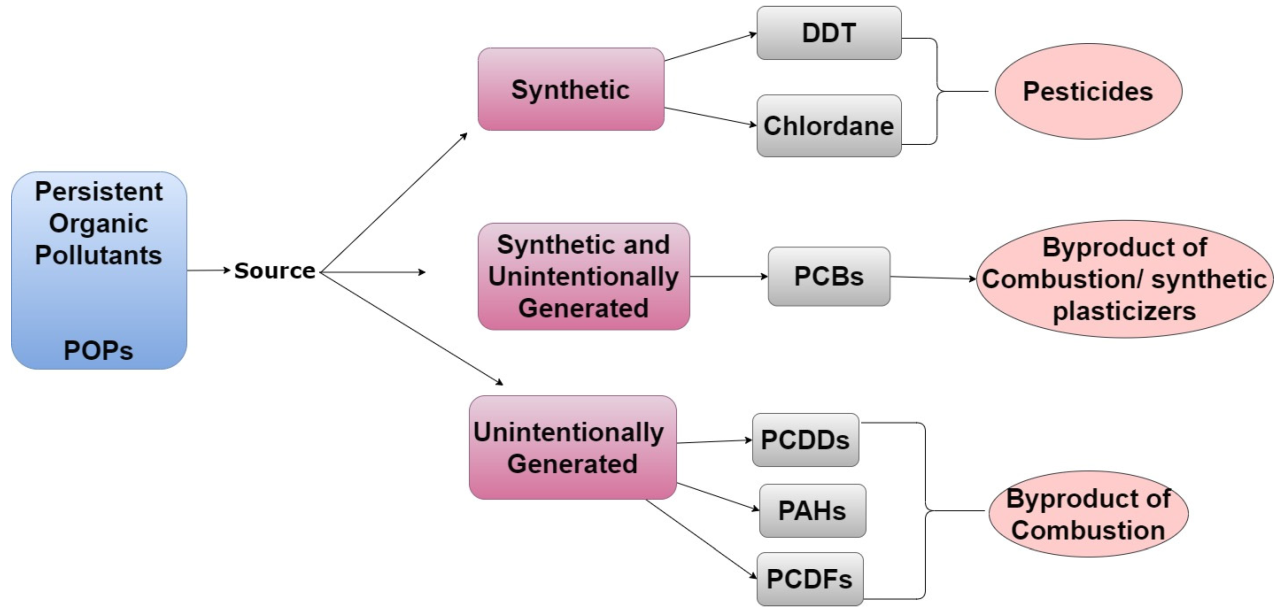
Geographic Variations and Vulnerable Populations

Source: indianexpress.com
The impact of environmental toxins on women’s reproductive health isn’t uniform across the globe. Exposure levels and the specific toxins encountered vary significantly depending on geographical location, leading to disparities in health outcomes. Understanding these variations and identifying vulnerable populations is crucial for effective prevention and intervention strategies.Exposure to environmental toxins is not evenly distributed. Industrialized nations often grapple with high levels of persistent organic pollutants (POPs) like PCBs and dioxins, linked to various reproductive problems.
Developing countries, on the other hand, may face greater challenges from exposure to heavy metals like lead and arsenic due to less stringent environmental regulations and informal waste disposal practices. Agricultural regions may see elevated pesticide exposure, impacting women working in fields or living near farms. Furthermore, proximity to industrial sites or contaminated water sources significantly increases exposure risk, regardless of national development level.
Variations in Environmental Toxin Exposure Across Geographic Regions
Industrialized nations, particularly those with a long history of industrial activity, often have legacy contamination issues. For example, areas with past PCB manufacturing or disposal practices may still have elevated levels in soil and water, leading to long-term exposure. In contrast, rapidly developing nations may experience acute exposure events due to unregulated industrial expansion or inadequate waste management systems.
For instance, lead contamination from informal lead recycling operations has been reported in several regions, posing significant risks to women and children. Coastal communities worldwide may experience higher levels of mercury contamination due to seafood consumption, with varying levels of contamination depending on local industrial activity and ocean currents.
Vulnerable Populations and Increased Risk
Women of lower socioeconomic status are disproportionately affected by environmental toxin exposure. They are more likely to live in areas with higher pollution levels, work in jobs with greater exposure risks (such as agriculture or manufacturing), and have less access to resources that could mitigate the impact of exposure. Similarly, women living in rural or remote areas may face barriers to accessing healthcare and information on environmental risks.
Indigenous populations often live in close proximity to sources of environmental contamination, experiencing higher exposure levels and limited access to preventative care. Migrant women and refugees may also be particularly vulnerable due to unstable living conditions and limited access to healthcare services.
Disparities in Healthcare Access and Resource Availability
Access to quality healthcare is crucial for managing the health consequences of environmental toxin exposure. However, significant disparities exist globally. Women in low-income countries often lack access to basic reproductive healthcare services, prenatal care, and monitoring for environmental toxin-related complications. Even in wealthier nations, access to specialized testing and treatment for environmental toxin-related reproductive issues may be limited, particularly for marginalized communities.
This lack of access leads to delayed diagnosis, inadequate treatment, and ultimately, worse health outcomes.
Addressing Environmental Justice Issues Related to Reproductive Health
Environmental justice is paramount. It necessitates equitable distribution of environmental benefits and burdens, ensuring that all communities have the right to live in healthy environments. Addressing environmental justice issues related to reproductive health requires a multi-pronged approach. This includes implementing stricter environmental regulations, promoting sustainable practices, investing in community-based interventions, improving access to healthcare services, and empowering women to advocate for their own health and well-being.
Research focused on understanding the specific risks faced by vulnerable populations is essential for developing targeted interventions. Ultimately, a commitment to environmental justice is fundamental to protecting women’s reproductive health globally.
Ultimate Conclusion
Understanding the impact of environmental toxins on women’s reproductive health is crucial for both individual well-being and public health initiatives. While the challenges are significant, there’s reason for hope. By raising awareness, supporting research, advocating for stronger environmental regulations, and making conscious lifestyle choices, we can collectively work towards a future where women are better protected from these invisible threats.
It’s time to prioritize a healthier environment for healthier generations to come. Let’s get involved and demand change!
Common Queries
What are some common symptoms linked to environmental toxin exposure affecting reproduction?
Symptoms can vary greatly and aren’t always directly attributable to toxins, making diagnosis tricky. However, some potential indicators include irregular periods, difficulty conceiving, recurrent miscarriages, and pregnancy complications. If you have concerns, consult your doctor.
Are all environmental toxins equally harmful?
No, different toxins have different mechanisms of action and varying levels of toxicity. Some are more potent endocrine disruptors than others, and the impact also depends on the level and duration of exposure.
Can I completely avoid exposure to environmental toxins?
Complete avoidance is nearly impossible, but significantly reducing exposure is achievable. Focus on making informed choices about food, water, and personal care products. Support policies that promote environmental protection.
What role does genetics play in susceptibility to environmental toxins?
Genetic factors can influence individual sensitivity to environmental toxins. Some individuals may be more genetically predisposed to adverse effects than others.