LGBTQ Healthcare Protections Blocked
LGBTQ healthcare protections blocked – that’s the harsh reality facing many in the queer community. This isn’t just about politics; it’s about lives, about access to vital care, and about the devastating consequences of systemic inequality. We’re diving deep into the fight for equitable healthcare, exploring the political battles, the personal stories, and the urgent need for change.
From the legislative battles raging in statehouses across the country to the everyday struggles faced by LGBTQ+ individuals seeking healthcare, the stakes are incredibly high. We’ll examine the unique health challenges faced by this community, the disparities in access and outcomes, and the heartbreaking stories of those denied essential care. We’ll also explore potential solutions and the crucial roles played by healthcare providers and advocacy groups in pushing for a more just and equitable future.
The Political Landscape Surrounding LGBTQ+ Healthcare
The fight for equitable healthcare access for LGBTQ+ individuals is deeply intertwined with the ever-shifting political landscape. Differing ideologies and priorities among political parties and lobbying groups significantly impact the availability and quality of healthcare services for this community, creating a complex and often contentious environment. Understanding this political context is crucial to advocating for meaningful change.
It’s infuriating that LGBTQ+ healthcare protections are being blocked, leaving vulnerable communities with fewer options. This is especially concerning considering the healthcare landscape is constantly shifting; for example, learn more about the impact of Walmart Health’s closure and the future of corporate healthcare by reading this article about despite Walmart Health’s closure, the company healthcare destination Scott Bowman.
The lack of accessible and inclusive care only exacerbates the existing inequalities faced by the LGBTQ+ community, highlighting the urgent need for stronger protective measures.
Current Political Climate and its Influence on LGBTQ+ Healthcare Access
The current political climate in many countries, including the United States, is characterized by a polarization on issues related to LGBTQ+ rights. Conservative factions often prioritize religious freedom and traditional family values, sometimes leading to arguments against policies that explicitly protect LGBTQ+ individuals. This can manifest in opposition to non-discrimination laws in healthcare settings, restrictions on gender-affirming care, and limited access to reproductive healthcare for transgender and non-binary individuals.
It’s infuriating that LGBTQ+ healthcare protections are being blocked, leaving vulnerable communities with fewer options. This feels especially cruel considering the news that Kaiser Permanente just scrapped plans for a massive new Seattle hospital tower, as reported in this article: kaiser permanente nixes 500m seattle bed tower capital spending. That’s half a billion dollars less in healthcare capacity, making the fight for inclusive healthcare access even more critical.
Conversely, progressive groups champion inclusivity and equality, advocating for comprehensive non-discrimination protections and access to a full range of healthcare services tailored to the unique needs of the LGBTQ+ community. This creates a battleground where the availability of vital healthcare services hinges on the political power dynamics at play.
Arguments For and Against Increased LGBTQ+ Healthcare Protections
Arguments in favor of increased LGBTQ+ healthcare protections often center on the principles of equality, human rights, and non-discrimination. Advocates highlight the documented disparities in healthcare access and outcomes for LGBTQ+ individuals, including higher rates of mental health conditions, substance abuse, and chronic diseases, often exacerbated by discrimination and lack of culturally competent care. They argue that providing explicit protections ensures fair treatment and access to quality healthcare, regardless of sexual orientation or gender identity.
Conversely, arguments against increased protections frequently cite concerns about religious freedom, parental rights, and the potential for what some perceive as excessive government intervention in healthcare decisions. Concerns are often raised regarding the cost of providing gender-affirming care and other specialized services. These arguments frequently fail to acknowledge the significant long-term health and economic benefits of providing equitable care.
Comparison of Political Party Approaches
Generally, left-leaning political parties tend to advocate for comprehensive LGBTQ+ healthcare protections, including non-discrimination laws, access to gender-affirming care, and reproductive healthcare services. They often support government funding and initiatives to address health disparities within the LGBTQ+ community. Right-leaning parties, conversely, often express more varied viewpoints, ranging from cautious support of some non-discrimination measures to outright opposition to gender-affirming care and other LGBTQ+-specific healthcare services.
The level of support or opposition within each party is often influenced by the specific political context and the prevailing social attitudes within the electorate. There is, however, a growing recognition among some moderate and centrist voices of the importance of ensuring access to quality healthcare for all, irrespective of sexual orientation or gender identity.
Timeline of Key Legislative Events Related to LGBTQ+ Healthcare
A detailed timeline would require significant space, but key events often include legislative victories such as the expansion of non-discrimination protections in healthcare settings (e.g., the Affordable Care Act’s non-discrimination clause in some jurisdictions) and setbacks, such as legislative attempts to restrict access to gender-affirming care in various states. The legal landscape is constantly evolving, and a comprehensive timeline would need to be regularly updated to reflect the most current legislative actions.
Lobbying Groups and Their Positions
Numerous organizations actively lobby on behalf of LGBTQ+ healthcare rights. Groups like the Human Rights Campaign (HRC) and GLAAD advocate for comprehensive non-discrimination protections and access to gender-affirming care. Conversely, some religious and conservative organizations lobby against specific aspects of LGBTQ+ healthcare protections, often focusing on religious freedom exemptions and restrictions on certain medical procedures. These lobbying groups play a significant role in shaping the political debate and influencing legislative outcomes, highlighting the complex interplay between advocacy and policy-making in this arena.
Specific Healthcare Access Issues Faced by the LGBTQ+ Community
Source: barelaw.in
The LGBTQ+ community faces significant disparities in healthcare access and quality compared to their non-LGBTQ+ counterparts. These disparities stem from a complex interplay of factors, including discrimination, lack of culturally competent care, and systemic barriers within the healthcare system itself. Understanding these unique needs and the resulting health inequities is crucial for advocating for meaningful change and improving the well-being of LGBTQ+ individuals.
LGBTQ+ individuals experience a range of health concerns that are either unique to their identities or exacerbated by societal stigma and discrimination. These include higher rates of mental health conditions like anxiety and depression, substance use disorders, and certain cancers. Furthermore, many LGBTQ+ individuals delay or avoid seeking necessary medical care due to fear of judgment, discrimination, or lack of inclusive providers.
Mental Health Disparities
The mental health of LGBTQ+ individuals is significantly impacted by experiences of discrimination, stigma, and violence. Studies consistently show higher rates of depression, anxiety, and suicidal ideation within this community compared to the general population. This is often linked to experiences of rejection from family and friends, bullying, harassment, and legal discrimination. For example, transgender individuals face particularly high rates of attempted suicide, often attributed to the stress of gender dysphoria, societal transphobia, and lack of access to gender-affirming care.
Access to mental healthcare services that are both affirming and competent in addressing the specific needs of LGBTQ+ individuals is crucial in mitigating these disparities.
It’s infuriating to see LGBTQ+ healthcare protections blocked, leaving vulnerable communities with fewer options. The recent news about hshs prevea close wisconsin hospitals health centers only exacerbates the problem, potentially reducing access to vital care even further for those already facing discrimination. This closure highlights the urgent need for stronger protections and increased access to affirming healthcare for LGBTQ+ individuals.
Disparities in Access to Gender-Affirming Care
Transgender and gender non-conforming individuals require access to gender-affirming care, which can include hormone replacement therapy, surgeries, and mental health support. However, access to this care is often limited due to insurance coverage issues, lack of providers with expertise in transgender healthcare, and discriminatory practices by healthcare professionals. Many transgender individuals face significant delays in accessing needed care, leading to negative impacts on their physical and mental health.
The lack of access can result in increased stress, depression, and feelings of isolation. For instance, a transgender woman may struggle to find a doctor willing to prescribe hormone replacement therapy, leading to delays in starting treatment and impacting their overall well-being.
HIV/AIDS and STI Rates
LGBTQ+ communities, particularly gay and bisexual men, experience disproportionately high rates of HIV and other sexually transmitted infections (STIs). This is often linked to social stigma, discrimination, and lack of access to preventative care and testing. Many individuals may avoid seeking testing or treatment due to fear of judgment or discrimination from healthcare providers. Furthermore, the lack of culturally competent sexual health education and outreach programs can contribute to higher infection rates.
For instance, a young gay man might delay getting tested for HIV due to fear of being judged by his doctor, leading to potential delays in treatment and increased risk of transmission.
Healthcare Access for Different LGBTQ+ Subgroups
| Subgroup | Access to Mental Healthcare | Access to Gender-Affirming Care | Access to HIV/STI Services |
|---|---|---|---|
| Transgender Women | Often limited due to discrimination and lack of specialized providers | Highly variable, often facing significant barriers | Can be limited due to stigma and lack of culturally competent services |
| Gay and Bisexual Men | Generally better than for some other subgroups, but still faces stigma | Not typically needed, but mental health support for related issues may be limited | More readily available, but stigma can still be a barrier |
| Lesbians and Bisexual Women | Often overlooked or minimized, leading to underdiagnosis and undertreatment | Not typically needed, but may face barriers accessing reproductive healthcare | Access can be limited due to lack of awareness and culturally competent services |
| Queer and Non-Binary Individuals | Highly variable, depending on individual experiences and intersecting identities | Access can be difficult due to lack of provider familiarity with diverse gender identities | Access varies, depending on individual experiences and intersecting identities |
The Impact of Blocked Protections on Mental and Physical Health
The denial or limitation of LGBTQ+ healthcare protections has profound and far-reaching consequences for the mental and physical well-being of this community. These consequences extend beyond simple access to care; they create systemic barriers that exacerbate existing health disparities and contribute to poorer health outcomes compared to the general population. The interconnectedness of healthcare access, mental health, and financial stability within the LGBTQ+ community cannot be overstated.
Mental Health Outcomes and Lack of Healthcare Access
Limited access to affirming and competent healthcare significantly impacts the mental health of LGBTQ+ individuals. The stress of discrimination, stigma, and fear of rejection within healthcare settings can lead to increased rates of anxiety, depression, and PTSD. Lack of access to specialized mental healthcare providers experienced in LGBTQ+ issues further compounds this problem, leaving many without the support they need to navigate complex mental health challenges.
This lack of culturally competent care can result in misdiagnosis, inappropriate treatment, and a worsening of mental health conditions. For example, transgender individuals facing gender dysphoria may experience significant distress if they cannot access gender-affirming care, leading to higher rates of suicide attempts.
Specific Physical Health Risks Due to Limited Access to Care
Beyond mental health, restricted healthcare access contributes to poorer physical health outcomes for LGBTQ+ individuals. This includes delayed or forgone preventative care, such as screenings for cancer or sexually transmitted infections (STIs). Many LGBTQ+ individuals, particularly transgender and gender non-conforming individuals, face barriers to accessing hormone replacement therapy (HRT) or gender-affirming surgeries, leading to significant health risks. Additionally, some LGBTQ+ individuals may avoid seeking care due to fear of discrimination or mistreatment, resulting in untreated or poorly managed chronic conditions.
The lack of access to comprehensive sexual health services, including HIV/AIDS testing and treatment, disproportionately affects LGBTQ+ communities, contributing to higher rates of infection.
Financial Burden of Healthcare Costs
The financial burden of healthcare is disproportionately high for LGBTQ+ individuals and families. Many lack employer-sponsored health insurance or struggle to afford premiums and deductibles. The added costs associated with gender-affirming care, specialized mental health services, and treatment for conditions related to discrimination can create significant financial hardship, forcing individuals to choose between necessary care and other essential needs.
This financial strain further contributes to stress and negatively impacts overall health and well-being. For example, the cost of hormone replacement therapy can be prohibitive for many transgender individuals, leading to delays or interruptions in treatment.
Examples of Delayed or Forgone Care and Adverse Consequences
Blocked healthcare protections directly lead to delayed or forgone care, with severe health consequences. A transgender individual unable to access gender-affirming hormone therapy may experience worsening gender dysphoria, leading to depression, anxiety, and even suicidal ideation. An LGBTQ+ individual avoiding routine preventative care due to fear of discrimination may face late-stage diagnosis of a serious illness, reducing treatment effectiveness and increasing mortality risk.
Similarly, an individual with an STI who avoids seeking treatment due to fear of judgment may experience serious long-term health complications or transmit the infection to others. These are not isolated incidents; they represent systemic failures in providing equitable healthcare access.
Resources Available to LGBTQ+ Individuals Seeking Healthcare
Despite limited protections, several resources are available to support LGBTQ+ individuals seeking healthcare:
- The Trevor Project: Provides crisis intervention and suicide prevention services for LGBTQ+ youth.
- GLAAD: Offers resources and information on LGBTQ+ health and wellness.
- National LGBTQ Task Force: Advocates for LGBTQ+ rights and provides resources on healthcare access.
- Local LGBTQ+ community centers: Often provide referrals to healthcare providers and support services.
- Federally Qualified Health Centers (FQHCs): Offer affordable healthcare services to underserved populations, including LGBTQ+ individuals.
Potential Solutions and Future Directions: Lgbtq Healthcare Protections Blocked
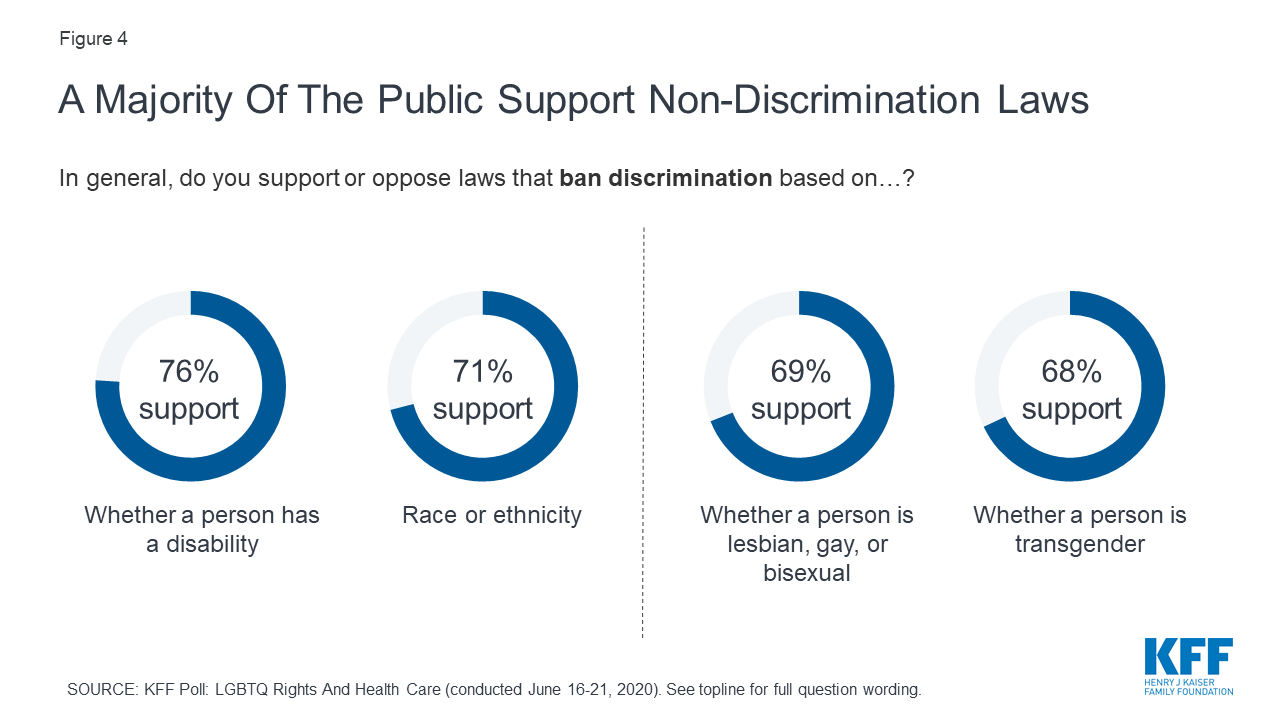
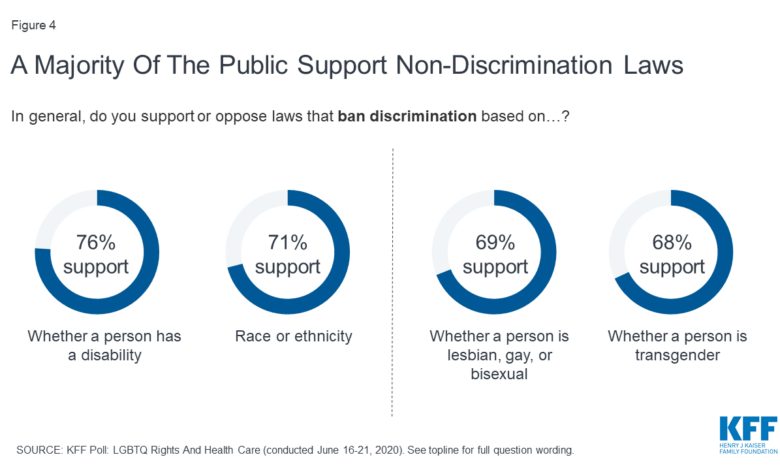
Source: kff.org
The recent setbacks in LGBTQ+ healthcare protections highlight the urgent need for proactive and comprehensive solutions. Addressing the systemic inequalities faced by this community requires a multi-pronged approach encompassing policy changes, improved healthcare models, robust advocacy, and learning from successful initiatives elsewhere. Moving forward, a commitment to creating a truly equitable healthcare system is paramount.Policy changes are crucial for improving LGBTQ+ healthcare access.
These changes must go beyond simple non-discrimination clauses and actively address the unique needs of the community.
Policy Changes to Improve LGBTQ+ Healthcare Access
Strengthening existing non-discrimination laws to explicitly include sexual orientation and gender identity in all aspects of healthcare, from insurance coverage to medical training, is a vital first step. This includes prohibiting discrimination in hiring and employment practices within healthcare settings, ensuring LGBTQ+ individuals are represented in all aspects of healthcare provision. Furthermore, policies should mandate inclusive healthcare provider training on LGBTQ+ health issues, promoting cultural competency and sensitivity.
Finally, dedicated funding streams for LGBTQ+ health initiatives should be established at both the national and local levels. This funding could support research, community-based programs, and the development of culturally appropriate healthcare services. The success of such policies can be measured by increased rates of preventative care and treatment among the LGBTQ+ community, coupled with a reduction in health disparities compared to the general population.
Models for Ensuring Equitable Healthcare
Several models can be employed to ensure equitable healthcare for all, regardless of sexual orientation or gender identity. One model involves the implementation of universal healthcare systems, such as those found in many European countries, which guarantee access to healthcare for all citizens regardless of their socioeconomic status or identity. This model prioritizes equitable access and resource allocation, reducing barriers faced by marginalized groups.
Alternatively, a strengthened regulatory framework within existing healthcare systems can ensure that all providers adhere to non-discrimination policies and provide culturally competent care. This approach relies on robust enforcement mechanisms and continuous monitoring to address any potential disparities. A comparative analysis of these models could reveal that universal healthcare systems often demonstrate better outcomes in terms of health equity for LGBTQ+ individuals, though the specific effectiveness varies depending on implementation details and existing social contexts.
For example, the Canadian healthcare system, while not perfect, generally provides better access to care for LGBTQ+ individuals than the US system due to its universal coverage.
The Role of Advocacy Groups
Advocacy groups play a pivotal role in pushing for change. They conduct research, raise public awareness, lobby policymakers, and provide direct support to LGBTQ+ individuals navigating the healthcare system. Groups like GLAAD, The Trevor Project, and numerous local organizations provide essential resources and actively campaign for legislative changes. For example, GLAAD’s work in media representation helps to normalize LGBTQ+ identities and increase public understanding of the issues they face, creating a more supportive environment for policy changes.
Their lobbying efforts, coupled with grassroots activism, significantly influence policy decisions. The effectiveness of advocacy groups is demonstrated by their impact on legislative victories, such as the expansion of non-discrimination protections in several states and cities.
Successful LGBTQ+ Healthcare Initiatives
Several countries and regions have implemented successful LGBTQ+ healthcare initiatives. The UK’s National Health Service (NHS) has made significant strides in integrating LGBTQ+ inclusive care into its services, including providing training to healthcare professionals and developing specific guidelines for transgender healthcare. Similarly, some regions in Canada have implemented comprehensive programs focusing on the mental health needs of LGBTQ+ youth, demonstrating the effectiveness of targeted initiatives.
The success of these programs is often evaluated through improvements in health outcomes, increased rates of help-seeking behavior, and reduced health disparities within the LGBTQ+ community. Analyzing these successful models provides valuable insights into strategies that can be adapted and implemented elsewhere.
An Ideal Healthcare System Protecting LGBTQ+ Rights
An ideal healthcare system would guarantee equitable access to high-quality care for all LGBTQ+ individuals, free from discrimination and prejudice. This system would incorporate comprehensive training on LGBTQ+ health for all healthcare providers, ensuring culturally competent and affirming care. It would also include proactive outreach programs to address the unique health needs of this community, such as preventative care, mental health services, and gender-affirming care.
Data collection and monitoring mechanisms would track health disparities and evaluate the effectiveness of interventions, allowing for continuous improvement. The system would also promote research focused on LGBTQ+ health, addressing knowledge gaps and developing evidence-based interventions. Such a system would be underpinned by strong anti-discrimination laws and robust enforcement mechanisms, ensuring accountability and protecting the rights of all individuals.
This model is not merely aspirational; elements of it exist in various parts of the world and can serve as building blocks for a more comprehensive and equitable system.
The Role of Healthcare Providers and Institutions
The fight for equitable LGBTQ+ healthcare is far from over, and the recent setbacks highlight the critical role healthcare providers and institutions play in ensuring all individuals receive the care they deserve, regardless of sexual orientation or gender identity. This means moving beyond simply providing medical services to actively fostering an environment of inclusivity, respect, and understanding. This section will explore the responsibilities of healthcare providers and institutions in achieving this vital goal.
Responsibilities of Healthcare Providers in Ensuring Equitable Care
Healthcare providers have a fundamental ethical and professional obligation to provide competent and compassionate care to all patients, including those in the LGBTQ+ community. This necessitates a deep understanding of the unique health concerns faced by this population, including higher rates of mental health conditions, HIV/AIDS, and certain cancers. It also requires actively challenging personal biases and actively working to create a safe and affirming environment where LGBTQ+ individuals feel comfortable disclosing their sexual orientation and gender identity.
This open communication is crucial for accurate diagnoses and effective treatment planning. Failure to provide equitable care is a breach of professional responsibility and can have serious consequences for patient health and well-being.
The Importance of Cultural Competency Training
Cultural competency training is not a one-time event but an ongoing process of learning and self-reflection. For healthcare professionals working with LGBTQ+ individuals, this training must encompass a broad understanding of LGBTQ+ identities, terminology, and experiences. It should also address the unique challenges faced by transgender and gender non-conforming individuals, including access to gender-affirming care and the potential for discrimination within the healthcare system.
Effective training should move beyond simple awareness and encourage active engagement in creating inclusive practices. This includes learning how to conduct sensitive patient interviews, use inclusive language, and appropriately address patients’ pronouns and chosen names. The ultimate goal is to foster a sense of trust and safety, enabling LGBTQ+ patients to feel comfortable seeking and receiving the care they need.
Creating Inclusive and Welcoming Environments for LGBTQ+ Patients, Lgbtq healthcare protections blocked
Creating an inclusive environment starts with the physical space. Healthcare institutions can demonstrate their commitment to inclusivity through visible signage affirming their LGBTQ+ inclusiveness, gender-neutral restrooms, and materials that reflect the diversity of the community. Beyond the physical space, institutional policies and procedures must be reviewed and updated to ensure they are non-discriminatory and affirming. This includes training staff on inclusive language, respectful communication, and the importance of patient confidentiality.
Patient intake forms should offer a range of gender identities and sexual orientations, and staff should be trained to use these forms respectfully and accurately. Furthermore, healthcare institutions should actively partner with LGBTQ+ community organizations to build trust and provide culturally appropriate services.
Best Practices for Providing Culturally Sensitive and Affirming Care
Best practices involve a multifaceted approach. This includes using inclusive language, respecting patient’s chosen names and pronouns, and creating a safe space for open communication. Providers should actively listen to patients’ concerns and experiences, validate their feelings, and ensure they feel heard and understood. It also involves understanding the unique challenges faced by different subgroups within the LGBTQ+ community, such as transgender individuals or those who identify as bisexual.
For example, providing access to gender-affirming care for transgender patients or providing culturally competent HIV/AIDS care for gay men are key elements of best practices. Healthcare providers should also actively seek feedback from LGBTQ+ patients and community organizations to continuously improve their care and services. A commitment to ongoing education and cultural humility is crucial.
Training Module for Healthcare Providers on LGBTQ+ Health Issues
A comprehensive training module should equip healthcare providers with the knowledge and skills necessary to provide equitable and affirming care. The module should be interactive and include case studies and role-playing exercises to facilitate learning and skill development.
- Module 1: Understanding LGBTQ+ Identities and Terminology: This module will cover the spectrum of sexual orientations and gender identities, common terminology, and the importance of using inclusive language. It will also address common misconceptions and stereotypes surrounding LGBTQ+ individuals.
- Module 2: Specific Health Concerns of the LGBTQ+ Community: This module will focus on the unique health risks and disparities faced by LGBTQ+ individuals, including higher rates of mental health conditions, HIV/AIDS, certain cancers, and issues related to gender-affirming care.
- Module 3: Providing Culturally Competent and Affirming Care: This module will provide practical strategies for creating inclusive environments, conducting patient interviews, using inclusive language, and addressing patients’ concerns with sensitivity and respect. It will also emphasize the importance of active listening and validation.
- Module 4: Addressing Discrimination and Bias in Healthcare: This module will explore the impact of discrimination and bias on LGBTQ+ patients’ health outcomes and provide strategies for addressing these issues within the healthcare setting. It will include discussions on implicit bias and microaggressions.
- Module 5: Working with Transgender and Gender Non-Conforming Individuals: This module will focus on the specific health needs and challenges faced by transgender and gender non-conforming individuals, including access to gender-affirming care and the importance of using correct pronouns and names.
- Module 6: Legal and Ethical Considerations: This module will address relevant laws and regulations related to LGBTQ+ healthcare, including patient confidentiality, anti-discrimination laws, and the provision of gender-affirming care.
Last Word
The fight for LGBTQ+ healthcare protections is far from over. The stories shared, the statistics revealed, and the systemic issues highlighted paint a clear picture: we need immediate and decisive action. This isn’t just a matter of policy; it’s a matter of human dignity and the right to access life-saving care. Let’s continue the conversation, amplify the voices of those affected, and demand change.
FAQ Compilation
What specific healthcare needs are unique to the LGBTQ+ community?
LGBTQ+ individuals face unique needs related to gender-affirming care, HIV/AIDS prevention and treatment, mental health concerns stemming from discrimination, and specific cancer screenings relevant to their identities.
How does the lack of healthcare protections impact LGBTQ+ individuals financially?
Many LGBTQ+ individuals face higher healthcare costs due to lack of insurance coverage for gender-affirming care, leading to financial strain and delaying or forgoing necessary treatment.
Are there any legal avenues available if healthcare protections are denied?
Depending on the location and specifics of the denial, legal recourse may be available through discrimination laws, but navigating this can be complex and require legal assistance.
What can I do to help advocate for LGBTQ+ healthcare protections?
Support LGBTQ+ advocacy organizations, contact your elected officials, and educate yourself and others about the issues. Even small actions can make a difference.
