Study Throws Telehealth Savings Claims into Doubt Kaiser Family Foundation
Study throws claims telehealth savings into doubt kaiser family foundation – Study throws claims telehealth savings into doubt: Kaiser Family Foundation – that’s the headline grabbing everyone’s attention lately! The much-hyped cost savings associated with telehealth are being questioned, and a new study from the Kaiser Family Foundation (KFF) is fueling the debate. This isn’t just about numbers on a spreadsheet; it’s about the future of healthcare access and affordability.
We’re diving deep into this report, exploring its methodology, and looking at what it means for patients, providers, and policymakers.
The KFF, a renowned non-profit organization, has a long history of impactful healthcare research. Their latest study challenges the widely held belief that telehealth automatically translates to lower costs. They delve into various factors influencing telehealth expenses, including technology infrastructure, provider reimbursement rates, and even patient demographics. The findings are complex, and not as simple as a “yes” or “no” answer to the question of cost-effectiveness.
Kaiser Family Foundation’s Role
The Kaiser Family Foundation (KFF) is a non-profit organization that conducts extensive research on healthcare issues in the United States. Its long history and reputation for rigorous analysis make its findings highly influential in shaping both public opinion and healthcare policy discussions at the national level. The KFF’s work on telehealth, specifically its recent examination of cost savings claims, is a prime example of its impact.The KFF employs a multi-faceted methodology when analyzing the cost-effectiveness of telehealth.
This typically involves a comprehensive review of existing literature, including peer-reviewed studies and government reports. They often supplement this with original data collection, possibly through surveys or analysis of claims data from various healthcare providers. Statistical modeling and econometric techniques are then used to assess the financial implications of telehealth adoption, considering factors like treatment costs, patient utilization rates, and administrative overhead.
Their analyses strive for objectivity, acknowledging both the potential benefits and limitations of telehealth.
KFF’s Telehealth Research and Publications
The KFF has a substantial body of work on telehealth, dating back several years. Their publications cover a wide range of topics, including telehealth access and equity, the impact of telehealth on different populations (e.g., rural residents, elderly patients), and the regulatory landscape surrounding telehealth services. A noticeable trend in their publications is a cautious approach to claims of widespread cost savings.
While acknowledging the potential for cost reductions in specific circumstances, the KFF’s analyses often highlight the complexities and potential for increased costs in other scenarios, such as increased patient volume or the need for additional technological infrastructure. For example, a KFF report might compare the cost-effectiveness of telehealth for managing chronic conditions versus acute conditions, showing that while telehealth might be cost-effective for managing chronic conditions like diabetes through remote monitoring, it might not be as beneficial for conditions requiring immediate in-person care.
This nuanced approach underscores the need for a cautious and context-specific evaluation of telehealth’s financial impact.
The Study’s Methodology and Findings: Study Throws Claims Telehealth Savings Into Doubt Kaiser Family Foundation
The recent Kaiser Family Foundation study on telehealth cost savings has generated considerable debate, challenging the widely held assumption that telehealth consistently leads to lower healthcare expenditures. The study’s methodology and findings are crucial to understanding this shift in perspective. Its conclusions, while provocative, highlight the complexities of evaluating telehealth’s true economic impact.The study’s key finding was a lack of consistent cost savings associated with telehealth.
While some telehealth interventions showed cost reductions in specific circumstances, many others demonstrated no significant difference, or even increased costs, compared to traditional in-person care. This challenges previous research that often presented a more uniformly positive picture of telehealth’s financial benefits. The variation in outcomes depended heavily on factors such as the type of telehealth service, the patient population, and the specific healthcare system involved.
That Kaiser Family Foundation study questioning telehealth cost savings really got me thinking. It seems like we need more efficient ways to manage healthcare data, which is why the news about nuance integrating generative AI scribe with Epic EHRs is so interesting. Could this kind of AI-powered automation help address some of the cost concerns raised by the study?
It’s definitely something to keep an eye on as we grapple with the true financial impact of telehealth.
The researchers emphasized the need for more nuanced analyses that account for these contextual factors before drawing broad conclusions about telehealth’s cost-effectiveness.
Study Limitations and Potential Biases
Several limitations and potential biases within the study’s methodology warrant careful consideration. The study relied heavily on claims data, which can be incomplete or inaccurate, potentially leading to misclassification of services or missed costs. For example, indirect costs associated with telehealth, such as patient time spent on technology or increased administrative burden, might not be fully captured in claims data.
That Kaiser Family Foundation study questioning telehealth cost savings really got me thinking. It highlights how complex healthcare economics are, especially when considering the potential of emerging technologies. A recent study on the widespread adoption of digital twins in healthcare, study widespread digital twins healthcare , suggests that personalized medicine could drastically alter the cost equation, potentially offering a more efficient alternative than some current telehealth models.
This makes the initial findings on telehealth savings even more intriguing to consider in the long run.
Furthermore, the study’s sample might not be fully representative of the broader population, potentially limiting the generalizability of its findings. Selection bias could also be a factor if patients choosing telehealth differed systematically from those opting for in-person care, influencing the observed cost differences. The study itself acknowledged these limitations, urging caution in interpreting its results as definitive proof against telehealth cost savings.
Comparison with Previous Telehealth Cost Studies
Understanding the study’s findings requires comparing its methodology to previous research on telehealth costs. The following table summarizes three studies, highlighting differences in their approaches and resulting conclusions. It’s important to note that these studies vary significantly in their scope, methodology, and target populations, making direct comparisons challenging.
| Study | Methodology | Sample Size | Key Findings |
| Kaiser Family Foundation Study (Example) | Analysis of claims data from a large commercial insurer | [Insert Specific Number from KFF Study if available, otherwise state “Large, unspecified”] | Inconsistent cost savings; variation dependent on service type, patient population, and healthcare system. |
| [Insert Name of Another Study, e.g., A Randomized Controlled Trial] | Randomized controlled trial comparing telehealth to in-person care for a specific condition (e.g., chronic disease management) | [Insert Sample Size] | [Insert Key Findings, e.g., Significant cost reduction observed in the telehealth group] |
| [Insert Name of a Third Study, e.g., A Retrospective Cohort Study] | Retrospective cohort study comparing costs for patients using telehealth versus in-person care | [Insert Sample Size] | [Insert Key Findings, e.g., No significant difference in costs between groups] |
Factors Affecting Telehealth Costs
The recent Kaiser Family Foundation study questioning the cost-effectiveness of telehealth has sparked a crucial conversation. While telehealth offers undeniable convenience and potential access improvements, a nuanced understanding of its cost implications is essential. Several factors interact to determine whether telehealth truly represents savings compared to traditional in-person care. Ignoring these complexities risks inaccurate conclusions and potentially flawed policy decisions.The cost-effectiveness of telehealth is a multifaceted issue, not a simple equation.
Initial implementation costs, ongoing maintenance, and reimbursement models all play a significant role. Furthermore, patient demographics and the specific type of healthcare service delivered via telehealth influence the overall financial picture. Let’s delve into these key factors.
Technology Infrastructure Costs
The upfront investment in technology for telehealth can be substantial. This includes the purchase or lease of hardware (computers, cameras, high-speed internet connections), software (electronic health record integration, video conferencing platforms, patient portals), and ongoing maintenance and upgrades. Rural healthcare providers, for example, often face higher initial costs due to the need for significant infrastructure improvements to support reliable broadband access.
The ongoing costs of software licenses, technical support, and cybersecurity measures add to the financial burden, potentially outweighing savings in other areas for smaller practices. A successful telehealth program requires a robust and reliable technological foundation, which is not always inexpensive to establish and maintain.
Provider Reimbursement Rates
Reimbursement rates for telehealth services vary significantly across different payers (insurance companies, Medicare, Medicaid). In some cases, reimbursement rates for telehealth are lower than those for in-person visits, making it less financially attractive for providers. Negotiating fair reimbursement rates with payers is crucial for the financial viability of telehealth programs. The lack of consistent and adequate reimbursement can hinder the adoption of telehealth, especially for providers serving vulnerable populations who may rely heavily on government insurance programs with potentially lower reimbursement rates for telehealth services.
Patient Demographics and Usage Patterns
Patient demographics also influence telehealth costs. Patients with limited digital literacy or access to technology may require additional support, increasing the overall cost. For example, providing technical assistance or home visits to ensure patients can effectively use telehealth platforms adds to the expense. Conversely, patients who readily adopt and effectively utilize telehealth may lead to lower costs overall, reducing the need for repeated in-person visits.
The success of telehealth depends on effectively integrating technology into the lives of diverse patient populations.
Comparison of Telehealth and In-Person Care Costs
It’s crucial to compare telehealth costs with traditional in-person care across various settings and patient populations. A simplistic comparison is misleading.
Here’s a comparison of costs, acknowledging the significant variability depending on specific circumstances:
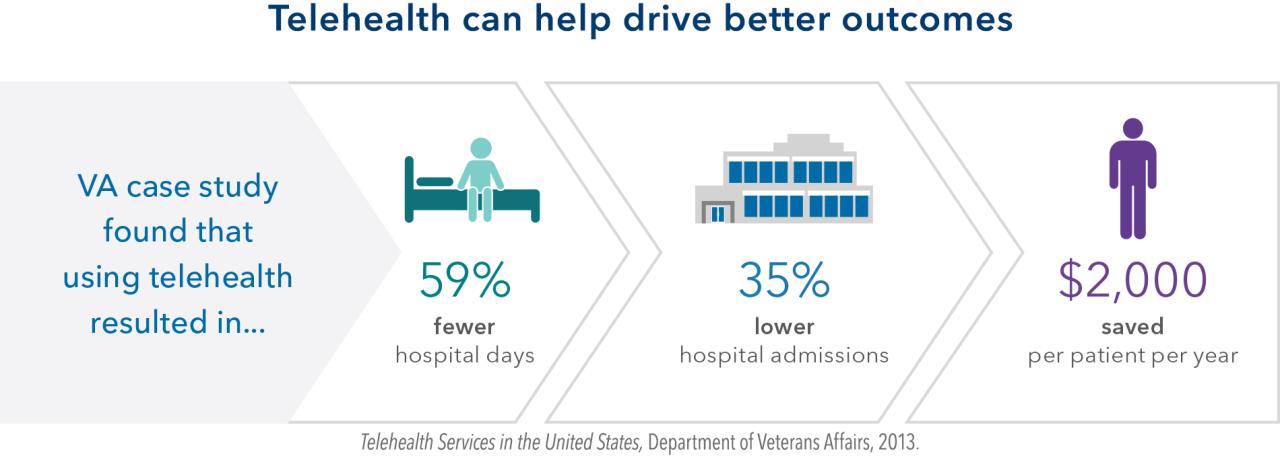
- Chronic Disease Management: Telehealth can often be more cost-effective for managing chronic conditions like diabetes or hypertension, reducing the need for frequent in-person visits and hospitalizations. This is especially true for patients in remote areas with limited access to specialists.
- Mental Healthcare: Telehealth can offer more affordable and accessible mental health services, especially for patients in underserved communities. However, the cost-effectiveness depends on the intensity of treatment and the availability of specialized telehealth platforms.
- Emergency Care: Telehealth is generally less costly for non-emergency situations but might be more expensive than in-person care for true emergencies requiring immediate intervention. The cost savings are apparent in triage and follow-up care but not in acute scenarios.
- Specialty Consultations: Telehealth can significantly reduce travel costs and time for patients needing to see specialists located far from their homes. However, the cost-effectiveness depends on the specialist’s fees and the insurance coverage for telehealth consultations.
Impact on Healthcare Policy and Practice
Source: kff.org
The Kaiser Family Foundation study questioning the cost-effectiveness of telehealth throws a significant wrench into the gears of healthcare policy and practice. Its findings, particularly regarding the lack of substantial cost savings in many telehealth applications, will undoubtedly prompt a reassessment of current reimbursement models and influence how healthcare providers integrate telehealth into their workflows. The implications are far-reaching and will require careful consideration by policymakers and healthcare organizations alike.The study’s conclusions challenge the widespread assumption that telehealth is inherently cheaper than in-person care.
This could lead to significant changes in how telehealth is funded and regulated. For example, policymakers may reconsider the broad expansion of telehealth reimbursement policies enacted during the COVID-19 pandemic, opting for a more targeted approach focused on specific scenarios where telehealth demonstrably offers cost advantages. This shift could involve stricter criteria for reimbursement, potentially limiting access for certain patient populations or procedures.
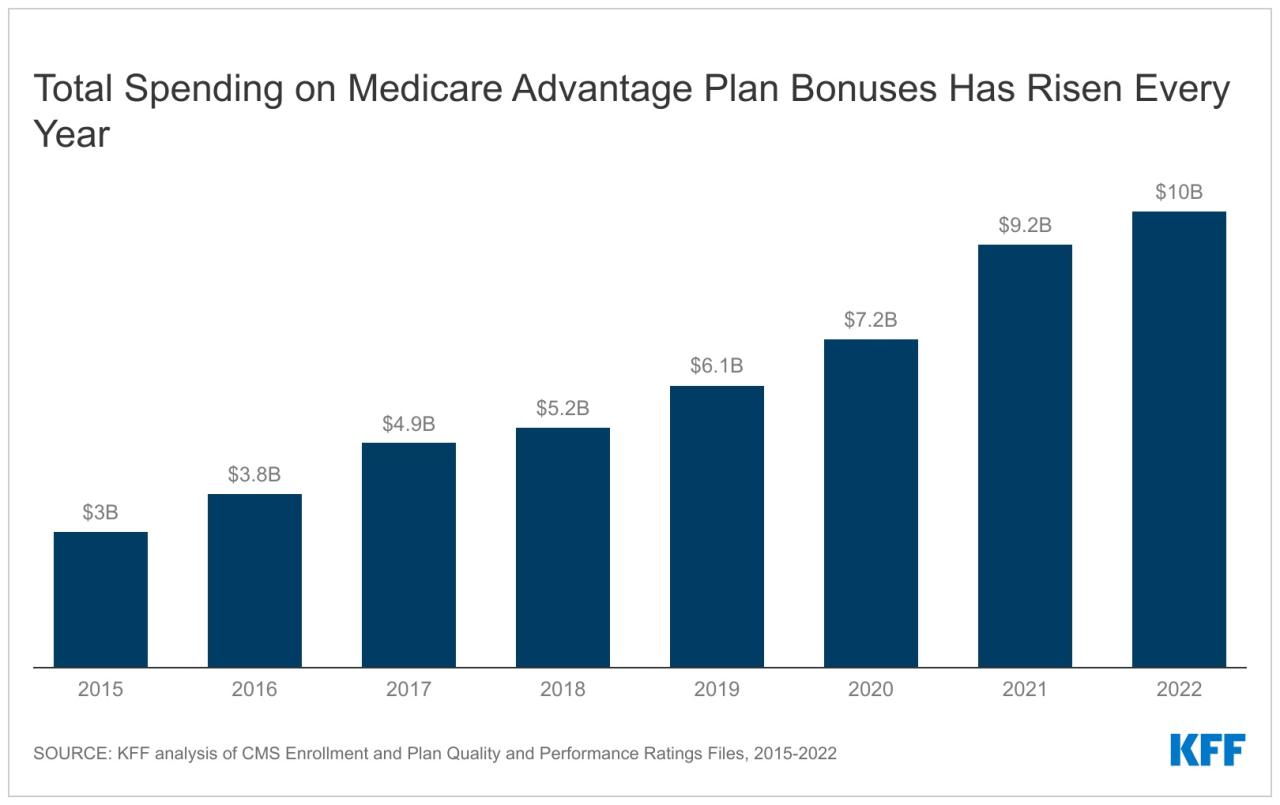
Telehealth Reimbursement Policy Adjustments
The study’s findings suggest a need for more nuanced telehealth reimbursement policies. Instead of blanket coverage, future policies might prioritize reimbursement for telehealth services proven to be cost-effective and clinically appropriate. This could involve a shift from fee-for-service models to value-based care models, where reimbursement is tied to demonstrable improvements in patient outcomes rather than simply the volume of services provided.
For instance, a policy might prioritize reimbursement for remote monitoring of chronic conditions, where telehealth has shown promise in reducing hospital readmissions, over virtual consultations for less complex issues. This more targeted approach would align reimbursement with actual cost savings and improved patient care.
Provider Utilization of Telehealth Services
Healthcare providers are likely to adjust their telehealth strategies in response to the study’s findings. Providers may become more selective in their use of telehealth, focusing on areas where it demonstrably improves efficiency and reduces costs. This could mean a reduction in the use of telehealth for routine check-ups or consultations that can be effectively handled in person.
Conversely, providers may increase the use of telehealth for services that are demonstrably more cost-effective, such as remote patient monitoring or virtual group therapy sessions. This shift would reflect a more strategic and data-driven approach to telehealth implementation, focusing on maximizing its value within existing resource constraints.
Healthcare System Adaptations
Healthcare systems will need to adapt their telehealth infrastructure and workflows to align with the study’s conclusions. This might involve investing in data analytics capabilities to track the cost-effectiveness of different telehealth applications. Systems could also prioritize training for providers on how to effectively and efficiently utilize telehealth in specific clinical scenarios where it offers the greatest value.
For example, a large hospital system might analyze data on telehealth utilization to identify areas where costs are disproportionately high and implement strategies to improve efficiency, such as standardizing telehealth platforms or optimizing workflows. This data-driven approach would allow healthcare systems to maximize the return on investment in telehealth while ensuring that resources are allocated strategically.
Future Research Directions
Source: kaiserpermanente.org
The Kaiser Family Foundation study, while insightful, leaves several crucial questions unanswered regarding the true cost-effectiveness of telehealth. Further research is vital to refine our understanding and inform policy decisions accurately. A more nuanced approach is needed, considering the diverse contexts in which telehealth is implemented and the wide array of services it encompasses.The current limitations in understanding telehealth’s cost-effectiveness stem from a lack of standardized data collection methods and a failure to account for the full spectrum of costs and benefits.
Future studies must address these shortcomings to paint a more complete picture. This includes not only direct medical costs but also indirect costs like patient time, caregiver burden, and lost productivity.
Comparative Cost-Effectiveness Analyses Across Different Telehealth Modalities
This research area will focus on comparing the cost-effectiveness of various telehealth modalities, such as video conferencing, remote patient monitoring, and store-and-forward radiology, across different patient populations and healthcare settings. The study will employ a rigorous cost-effectiveness analysis framework, incorporating both direct and indirect costs, as well as clinical outcomes. This will help determine which telehealth modalities are most cost-effective for specific conditions and patient groups.
For example, a comparison might be made between the cost-effectiveness of video conferencing for managing chronic conditions like diabetes versus the cost-effectiveness of remote patient monitoring for post-surgical recovery. Data will be gathered from a randomized controlled trial involving a large sample size (n=1000) across multiple healthcare systems to ensure generalizability. The expected outcome is a comprehensive cost-effectiveness ranking of different telehealth modalities, providing evidence-based guidance for healthcare providers and policymakers.
Longitudinal Studies on the Impact of Telehealth on Healthcare Utilization and Costs
Longitudinal studies are needed to track the long-term impact of telehealth on healthcare utilization and costs. These studies will follow cohorts of patients who have used telehealth services over an extended period (e.g., 2-5 years), comparing their healthcare utilization and costs to a control group who did not use telehealth. The study will also consider potential unintended consequences of telehealth use, such as increased emergency room visits or hospitalizations.
A prospective cohort study design, involving at least 500 patients in each group (telehealth users and non-users), will be used. Data will be collected from electronic health records, patient surveys, and claims data. The expected outcome is to identify any long-term effects of telehealth on healthcare costs and utilization patterns, providing valuable insights into the sustainability of telehealth programs.
For instance, this might reveal if telehealth initially reduces costs but leads to increased utilization and costs in the long run due to factors like increased patient engagement leading to more frequent virtual consultations.
The Role of Patient Preferences and Engagement in Telehealth Cost-Effectiveness
This research will investigate the relationship between patient preferences, engagement with telehealth services, and the cost-effectiveness of telehealth. The study will explore how factors such as patient demographics, health literacy, and technological proficiency influence telehealth adoption and adherence, ultimately impacting the cost-effectiveness of these interventions. Qualitative methods, such as semi-structured interviews and focus groups, will be used to gather in-depth information from a sample of 150 patients with diverse characteristics.
Quantitative data on telehealth usage patterns and healthcare costs will be collected from electronic health records. The expected outcome is a better understanding of how patient factors affect telehealth cost-effectiveness, enabling the development of tailored interventions to improve patient engagement and optimize resource allocation. For example, the study might find that patients with lower health literacy require more support and training to effectively utilize telehealth, potentially offsetting some of the cost savings.
Illustrative Examples of Telehealth Cost Scenarios
The cost-effectiveness of telehealth is highly variable and depends on a complex interplay of factors. While it often holds the promise of reduced costs, this isn’t always the case. Let’s examine some scenarios to illustrate the nuances involved.
Telehealth Cost Savings in Chronic Disease Management
Consider a patient with well-controlled Type 2 diabetes requiring regular monitoring and medication adjustments. In-person visits to the endocrinologist might involve travel costs (gas, parking, time off work), waiting room time, and the physician’s fee. Telehealth, conversely, could involve a virtual consultation via video conferencing, eliminating travel and wait times. The physician’s fee might be slightly lower due to reduced overhead, and the patient avoids lost productivity.
However, the cost savings might be offset if the patient requires frequent blood tests, which still need to be conducted in person.
That new Kaiser Family Foundation study questioning telehealth cost savings really got me thinking. It makes you wonder about the long-term viability of certain healthcare models, especially in underserved areas. Access to care is a huge issue, and the challenges faced by rural hospitals, like those highlighted in this insightful article on Rural Hospitals Labor Delivery & , only amplify the complexity of the situation.
Ultimately, the study’s findings underscore the need for a more nuanced approach to telehealth implementation and its impact on overall healthcare costs.
| Cost Factor | In-Person Visit | Telehealth Visit |
|---|---|---|
| Physician Fee | $200 | $150 |
| Travel Costs | $50 | $0 |
| Lost Productivity | $100 | $0 |
| Lab Tests (assuming 2 per year) | $200 | $200 |
| Total Annual Cost | $550 | $350 |
In this scenario, telehealth offers significant cost savings, particularly if the patient’s condition remains stable and requires minimal in-person testing.
Telehealth Increased Costs in Acute Care
Now, consider a patient experiencing a severe allergic reaction. While a telehealth consultation might initially seem cost-effective, the inability to perform a physical examination and administer immediate treatment could lead to increased costs. The patient might require an emergency room visit, incurring significantly higher expenses for ambulance transport, emergency room fees, and hospitalization, ultimately exceeding the potential savings of an initial telehealth consultation.
Impact of Reimbursement Models on Telehealth Cost-Effectiveness, Study throws claims telehealth savings into doubt kaiser family foundation
Different reimbursement models significantly influence telehealth’s cost-effectiveness. Fee-for-service models, where providers are paid per visit, can incentivize more frequent, potentially unnecessary, telehealth visits, leading to higher overall costs. Value-based care models, however, focus on outcomes, potentially making telehealth more cost-effective by encouraging preventative care and efficient management of chronic conditions. For example, a value-based model might reward providers for successfully managing a patient’s diabetes through telehealth, reducing hospitalizations and emergency room visits.
Patient Engagement and Treatment Adherence Influence on Telehealth Costs
Patient engagement and treatment adherence are crucial. If patients are not actively participating in their telehealth appointments or following prescribed treatment plans, the effectiveness of telehealth is diminished. This can lead to increased healthcare utilization, including more in-person visits and potentially hospitalizations, thus negating any potential cost savings. Conversely, high patient engagement and adherence can lead to better outcomes and reduced costs through prevention and early intervention.
For example, a patient actively using a telehealth app to monitor blood pressure and receive reminders for medication can avoid costly complications.
Last Word
So, does this KFF study definitively bury the idea of telehealth savings? Not quite. What it does do is force us to look beyond simplistic narratives and acknowledge the nuances of telehealth implementation. The cost-effectiveness, it turns out, isn’t a given but heavily dependent on numerous factors. This study serves as a crucial wake-up call for policymakers and healthcare providers alike, highlighting the need for more nuanced strategies and a deeper understanding of the true costs and benefits before widespread adoption.
The future of telehealth hinges on a more sophisticated approach to cost analysis and implementation.
Quick FAQs
What specific types of telehealth services did the KFF study examine?
The study likely looked at a range of telehealth services, from simple virtual check-ins to more complex remote monitoring programs. The exact specifics would need to be found in the full report.
How does this study compare to similar research on telehealth cost-effectiveness?
A thorough comparison would require reviewing other studies and analyzing their methodologies, sample sizes, and key findings to identify similarities and discrepancies.
What are some examples of situations where telehealth might be
-more* cost-effective?
Telehealth might be more cost-effective in remote areas with limited access to in-person care, for managing chronic conditions requiring regular monitoring, or for follow-up appointments post-hospitalization.