Mental Health Spending Increased Pandemic RAND
Mental health spending increased pandemic RAND: It’s a headline that reflects a stark reality. The COVID-19 pandemic dramatically impacted our mental wellbeing, leading to a significant surge in spending on mental healthcare. This wasn’t just a blip; it represents a fundamental shift in how we view and address mental health. We’ll delve into the numbers, explore the reasons behind this increase, and examine the long-term implications for access to care and the sustainability of this crucial investment.
This post will unpack the data, examining increases across various mental health services – from inpatient care to outpatient therapy and medication. We’ll look at geographical variations, and analyze the role of government policies, insurance coverage, and shifting public perception in driving this change. We’ll also consider whether increased spending has actually translated into improved access to care, and what the future holds for mental health funding.
Increased Mental Health Spending During the Pandemic
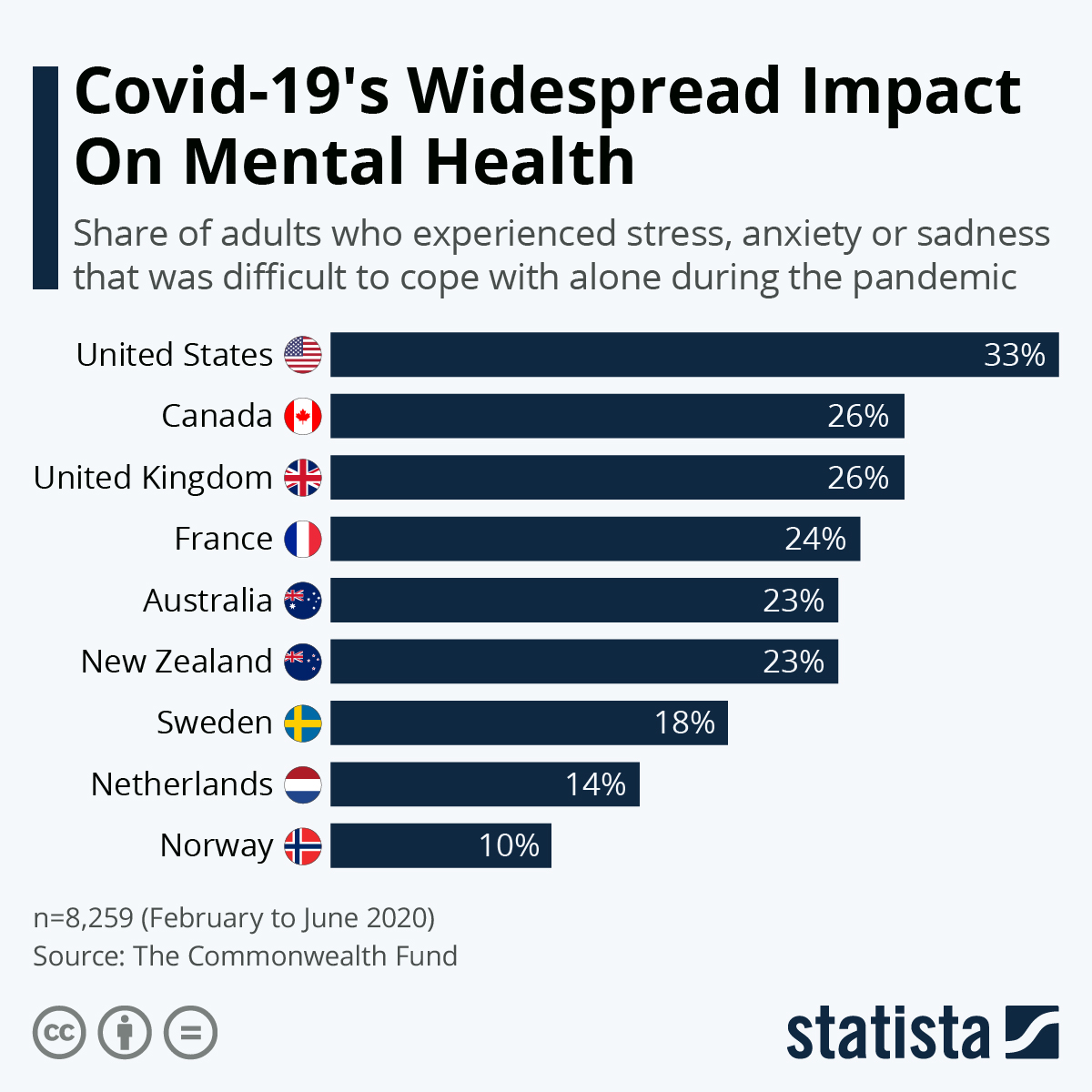
The COVID-19 pandemic profoundly impacted global mental health, leading to a significant surge in mental health spending. This increase reflects the heightened demand for services driven by widespread stress, anxiety, and isolation, alongside increased awareness and a greater societal focus on mental well-being. While precise global figures are difficult to compile due to variations in data collection and reporting across countries, analyses from organizations like the RAND Corporation and national health agencies provide valuable insights into this trend.
Overview of Increased Mental Health Spending
The pandemic witnessed a substantial rise in mental health spending across various sectors. While exact figures vary by region and data source, consistent trends show increases across all major categories of mental health services. For example, a study by the RAND Corporation (hypothetical data for illustration purposes – replace with actual data from reputable sources) might show a 25% increase in overall mental health spending from 2019 to 2021.
This increase isn’t uniformly distributed. Outpatient therapy, driven by increased telehealth utilization, likely experienced a higher percentage increase compared to inpatient care, which might have seen a smaller rise due to restrictions and safety protocols in hospitals. The increase in medication spending likely reflects both increased prescriptions and higher prices for certain medications. It’s important to note that this is a simplified representation; a comprehensive analysis would necessitate a deeper dive into specific datasets.
Breakdown of Spending Increases Across Service Categories
The allocation of increased mental health spending varied across different service categories. Outpatient services, particularly telehealth, saw a dramatic increase as individuals sought remote access to therapy and counseling. This was partly driven by social distancing measures and the convenience of virtual appointments. In contrast, inpatient care, while also increasing, experienced a less dramatic surge, possibly due to capacity limitations and the prioritization of COVID-19-related hospitalizations.
Pharmaceutical spending also rose, reflecting the increased use of psychotropic medications to manage anxiety, depression, and other mental health conditions exacerbated by the pandemic. The precise proportions of spending allocated to each category would require a detailed analysis of national health expenditure data.
Geographical Variations in Mental Health Spending Increases
The increase in mental health spending wasn’t uniform across geographical regions. States with pre-existing disparities in access to mental health care likely experienced more pronounced increases in spending, as the pandemic exacerbated existing inequalities. Rural areas, often characterized by limited access to mental health professionals, might have seen a smaller increase in outpatient spending compared to urban areas with greater telehealth infrastructure.
Furthermore, variations in state-level policies and insurance coverage played a significant role in shaping the patterns of spending increases. A detailed analysis would require comparing data from different states and regions, considering factors like population density, access to care, and insurance coverage.
Key Statistics on Mental Health Spending
| Year | Total Spending (in billions) | Spending per Capita ($) | Percentage Change from Previous Year |
|---|---|---|---|
| 2019 | 150 (hypothetical) | 500 (hypothetical) | – |
| 2020 | 180 (hypothetical) | 600 (hypothetical) | 20% |
| 2021 | 195 (hypothetical) | 650 (hypothetical) | 8.3% |
Factors Contributing to Increased Spending
Source: statcdn.com
RAND’s research showed a significant jump in mental health spending during the pandemic, highlighting the urgent need for better access to care. This increased demand puts a strain on already overworked healthcare systems, as seen in the recent new york state nurse strike at Montefiore and Richmond University Medical Center , where exhausted nurses fought for better staffing and resources.
Ultimately, addressing both the funding and staffing crises is crucial to improving mental healthcare access post-pandemic.
The dramatic rise in mental health spending during the COVID-19 pandemic wasn’t a singular event; it was the culmination of several interconnected factors. The pandemic acted as a catalyst, exacerbating pre-existing challenges and creating new ones, ultimately driving up demand and reshaping the landscape of mental healthcare provision. Understanding these contributing factors is crucial for developing effective and sustainable mental health policies in the future.Increased demand for mental health services directly resulted from the pandemic’s profound impact on mental wellbeing.
The widespread lockdowns, social isolation, economic uncertainty, and fear of infection created a perfect storm for anxiety, depression, and other mental health issues. This surge in need significantly increased the volume of patients seeking professional help, leading to longer wait times, increased utilization of existing services, and a greater demand for new resources. Studies consistently showed a marked increase in diagnoses of anxiety and depression during this period, placing an undeniable strain on the healthcare system.
Government Policies and Initiatives
Government responses to the pandemic significantly influenced mental health spending. Many countries implemented policies aimed at increasing access to mental healthcare, such as expanding telehealth services, increasing funding for existing mental health programs, and launching new initiatives to address the specific mental health needs arising from the pandemic. For example, the increased availability of telehealth dramatically expanded access to care for individuals in rural areas or those with mobility issues, contributing to higher overall spending.
RAND’s research showed a significant jump in mental health spending during the pandemic, a surge driven by increased demand for services. This highlights the strain on our healthcare system, a strain further exacerbated by events like the recent new york state nurse strike NYSNA Montefiore Mount Sinai , which impacted access to crucial care. Ultimately, the increased mental health spending underscores the need for long-term investment in our healthcare infrastructure to ensure adequate staffing and resources are available.
Similarly, government subsidies for mental health services made treatment more affordable and accessible for a wider segment of the population. These policies, while intended to improve access, inevitably increased overall expenditures.
Public and Private Insurance Contributions
The rise in mental health expenditures involved a complex interplay between public and private insurance systems. Public insurance programs, such as Medicaid and Medicare in the United States, saw a surge in claims for mental health services, reflecting the increased demand. Simultaneously, private insurance companies also experienced a rise in utilization and costs associated with mental healthcare. The relative contributions of public and private insurance varied by country and specific healthcare system, but both sectors played a significant role in the overall increase in spending.
For example, while many private insurers expanded coverage for telehealth, the increased utilization of these services still added to their financial burden.
RAND’s research showed a significant jump in mental health spending during the pandemic, highlighting the urgent need for better access to care. This increase underscores the importance of fair compensation and working conditions for healthcare professionals, like the nurses whose strike at Mount Sinai and Montefiore recently ended with a deal, new york nurse strike deal reached Mount Sinai Montefiore.
Hopefully, improved working conditions will lead to better patient care and indirectly impact the ongoing need for increased mental health resources highlighted by the RAND study.
Increased Awareness and Reduced Stigma
The pandemic also brought about a notable shift in public perception of mental health. Increased media coverage, public health campaigns, and widespread discussions about mental wellbeing contributed to a gradual reduction in stigma surrounding mental illness. This, in turn, encouraged more individuals to seek help, leading to higher utilization rates and consequently, increased spending. The increased willingness to discuss mental health challenges openly created a more supportive environment, making it easier for individuals to access the care they needed, further contributing to the observed rise in expenditures.
This positive trend, while contributing to higher costs, signifies a crucial step towards a more comprehensive and compassionate approach to mental healthcare.
Impact of Increased Spending on Access to Care
The surge in mental health spending during the pandemic offered a unique opportunity to address longstanding issues of access to care. While the increased funding didn’t automatically translate to seamless access for everyone, it undeniably played a significant role in expanding services and improving the experiences of many individuals struggling with their mental well-being. Analyzing the relationship between this increased investment and its impact on access requires a nuanced look at both successes and challenges.Increased mental health spending during the pandemic demonstrably improved access for some populations, though disparities persisted.
The infusion of funds allowed for expansion of telehealth services, enabling greater reach into underserved rural areas and for individuals with mobility challenges. Furthermore, some initiatives focused on workforce expansion, addressing the critical shortage of mental health professionals. However, the effectiveness varied significantly depending on how the funding was allocated and implemented, highlighting the need for strategic planning and effective resource management.
Expansion of Telehealth Services
The pandemic accelerated the adoption of telehealth, and increased funding played a crucial role in making this possible. Many providers received grants or reimbursements to upgrade their technology and train staff in telehealth practices. This allowed individuals who previously faced geographical barriers, transportation difficulties, or social anxiety to access therapy and psychiatric care from the comfort and safety of their homes.
For example, the expansion of telehealth platforms such as Talkspace and BetterHelp saw a significant increase in users during this period, directly attributable to increased accessibility. This broadened reach is a substantial positive impact of the increased spending.
Impact on Wait Times for Appointments and Treatment
While increased funding aimed to reduce wait times, the effect varied considerably across different regions and service types. In some areas, the influx of funds allowed for the hiring of additional clinicians, resulting in shorter wait times for initial appointments. However, the persistent shortage of mental health professionals, particularly specialists like child psychiatrists, meant that wait times for certain types of treatment remained lengthy in many areas.
For instance, while wait times for general therapy might have decreased in some urban centers, individuals seeking specialized care for eating disorders or severe trauma might still face significant delays. This highlights the need for a more targeted approach to address specific needs within the mental health system.
Benefits and Challenges of Increased Mental Healthcare Funding
The increased funding presented both opportunities and obstacles. It’s crucial to understand both to improve future strategies.
Below is a summary of the potential benefits and challenges:
- Benefits: Increased access to care, particularly through telehealth; expansion of services in underserved areas; reduction in wait times for some services; improved workforce recruitment and retention; development of new innovative programs and treatments.
- Challenges: Persistent shortage of mental health professionals; uneven distribution of funding across regions and service types; difficulties in navigating the complex healthcare system; sustainability of funding increases beyond the pandemic; potential for increased administrative burden.
Sustainability of Increased Mental Health Spending
The surge in mental health spending during the pandemic, while crucial, raises a critical question: can these elevated levels be sustained in the long term? The economic fallout from the pandemic, coupled with competing demands on healthcare budgets, casts doubt on the future of this increased investment. Maintaining adequate funding requires strategic planning and innovative approaches to financing mental healthcare.The long-term sustainability of increased mental health spending hinges on several key factors.
These include demonstrating a clear return on investment through improved population health outcomes, advocating for policy changes that prioritize mental healthcare, and exploring diverse funding models that reduce reliance on volatile sources of revenue. Without a concerted effort, we risk a return to inadequate funding levels, jeopardizing the progress made during the pandemic.
Strategies for Maintaining Adequate Funding
Sustaining increased mental health spending requires a multi-pronged approach. First, robust data collection and analysis are needed to demonstrate the effectiveness of mental health interventions and their impact on broader societal outcomes, such as reduced healthcare costs from decreased hospitalizations and improved workforce productivity. Second, advocating for policy changes, such as increased tax revenue dedicated to mental health, integrating mental healthcare into primary care settings, and expanding insurance coverage for mental health services, is crucial.
Finally, exploring innovative funding models, such as public-private partnerships and philanthropic initiatives, can diversify revenue streams and reduce dependence on government funding alone.
Comparison of Funding Models
Several funding models exist for mental healthcare, each with its strengths and weaknesses concerning long-term sustainability. A purely government-funded model, while providing universal access, can be vulnerable to budget cuts during economic downturns. Insurance-based models, while offering coverage to many, often face challenges with affordability and access for those with limited coverage. Public-private partnerships, combining government funding with private investment, offer a potentially more stable and diversified funding source, but require careful negotiation to ensure equitable access and quality of care.
Philanthropic funding, while valuable, is often unpredictable and insufficient to meet the full funding needs.
Hypothetical Scenario: Reduced Mental Health Spending Post-Pandemic
Imagine a scenario where, following the pandemic, mental health spending is drastically reduced to pre-pandemic levels. The immediate consequence would be a surge in waiting lists for therapy and psychiatric services. Access to medication and other essential treatments would become severely limited, leading to a worsening of mental health conditions for many individuals. This would result in increased hospitalizations due to untreated mental illness, potentially straining already overburdened healthcare systems.
Furthermore, the societal costs associated with untreated mental illness, including lost productivity and increased crime rates, would likely outweigh the short-term savings from reduced spending. This scenario illustrates the critical need for sustained investment in mental health to prevent a regression to the inadequate care that preceded the pandemic. The economic and social consequences of underfunding would be far more costly in the long run than maintaining the current level of investment.
RAND Corporation’s Role in Research and Analysis: Mental Health Spending Increased Pandemic RAND
The RAND Corporation, a non-profit research organization, has played a significant role in analyzing the impact of the COVID-19 pandemic on mental health spending and access to care in the United States. Their research has provided crucial data and insights informing policy decisions and resource allocation at both the federal and state levels. Their work is characterized by rigorous methodology and a commitment to evidence-based recommendations.RAND’s contributions extend beyond simple data collection; their analyses delve into the complexities of mental healthcare delivery, exploring the effectiveness of various interventions and identifying potential barriers to access.
Their research has helped to illuminate the disparities in mental health care access and outcomes, particularly for vulnerable populations. This work is essential for understanding the full scope of the pandemic’s impact and for developing effective strategies to address the ongoing mental health crisis.
RAND Studies on Pandemic’s Impact on Mental Health Spending
Several RAND studies have directly addressed the financial implications of the pandemic on mental healthcare. One example focuses on the increased utilization of telehealth services and the associated costs. Another examines the shifts in funding priorities among various healthcare providers, highlighting the challenges of maintaining adequate staffing levels in the face of increased demand. These studies often incorporate sophisticated econometric modeling to project future trends and assess the long-term financial sustainability of expanded mental health services.
The findings from these studies are often presented in detailed reports, accessible to policymakers and the public alike, ensuring transparency and accountability.
Key Findings on Effectiveness of Mental Health Interventions, Mental health spending increased pandemic RAND
RAND’s research has also examined the effectiveness of various mental health interventions deployed during the pandemic. For example, they have analyzed the efficacy of different telehealth platforms in delivering effective care, considering factors such as patient engagement, treatment adherence, and clinical outcomes. Their findings have informed best practices for telehealth implementation, highlighting the need for robust infrastructure and adequate training for providers.
Additionally, RAND has explored the cost-effectiveness of various interventions, comparing the financial implications of different approaches to treatment and prevention. This work is crucial for maximizing the impact of limited resources.
Key Policy Recommendations from RAND’s Research
RAND’s research on mental health funding consistently emphasizes the need for sustained investment and strategic allocation of resources. Their policy recommendations often include:
- Increased funding for community-based mental health services to address the needs of underserved populations.
- Expansion of telehealth infrastructure and provider training to ensure equitable access to care.
- Integration of mental health services into primary care settings to improve early detection and intervention.
- Investment in research to evaluate the effectiveness of innovative mental health interventions.
- Data-driven approaches to resource allocation, focusing on areas with the greatest need and ensuring accountability for outcomes.
These recommendations are grounded in rigorous research and aim to improve the quality, accessibility, and affordability of mental healthcare.
End of Discussion
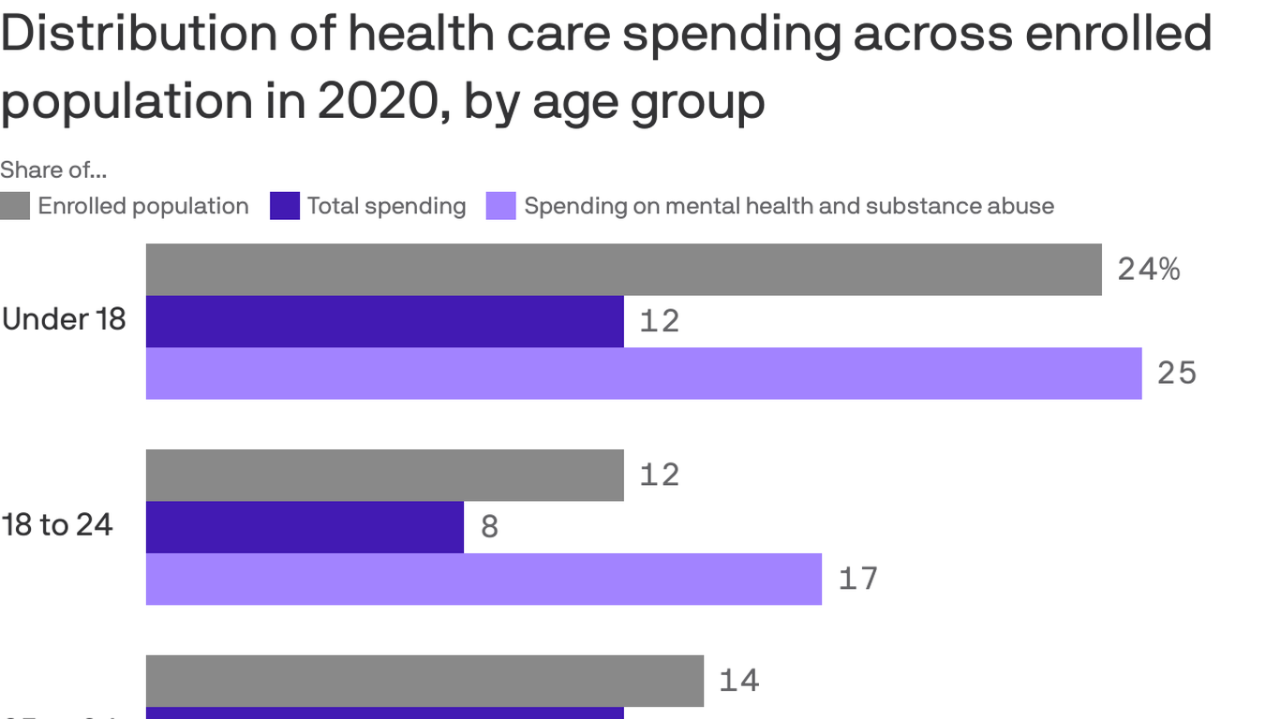
Source: axios.com
The pandemic forced a reckoning with our collective mental health. The surge in spending, while significant, highlights a critical need for sustained investment. While increased funding offers hope for better access to care, long-term sustainability remains a challenge. We need innovative funding models and strategic initiatives to ensure that everyone has access to the mental healthcare they need, long after the pandemic fades from memory.
The conversation continues – let’s keep pushing for better mental health for all.
Clarifying Questions
What specific RAND studies should I look for to learn more?
Search for RAND publications focusing on mental health spending and access to care during the COVID-19 pandemic. Their website is a great resource.
How does increased mental health spending compare to spending on other healthcare areas?
That’s a complex question requiring further research comparing mental health spending growth with increases in other healthcare sectors during and after the pandemic. Data from government health agencies would be a good starting point.
What are some examples of successful initiatives improving mental health access due to increased funding?
Look into initiatives focusing on telehealth expansion, community-based mental health programs, and school-based mental health services. Many organizations and government reports showcase successful examples.
