No Appointments Available Americas Escalating Primary Care Shortage
No appointments available americas escalating primary care shortage – No Appointments Available: Americas’ escalating primary care shortage – that’s the stark reality facing millions. It’s not just about inconvenience; it’s a crisis impacting health, finances, and overall well-being across the continent. From bustling cities to remote villages, accessing timely primary care is becoming increasingly difficult, leaving many vulnerable to preventable health issues. This isn’t just a problem; it’s a story of overworked doctors, strained systems, and patients caught in the middle.
This post delves into the heart of this crisis, exploring the reasons behind the shortage, the devastating consequences for patients, and potential solutions that could bring much-needed relief. We’ll look at the factors driving this problem – everything from physician burnout to systemic inefficiencies – and explore innovative approaches like telehealth and team-based care. Get ready to uncover the truth behind the empty appointment slots and the fight to ensure everyone has access to the healthcare they deserve.
The Current State of Primary Care in the Americas
Access to primary care in the Americas is a complex and pressing issue, varying significantly across countries and regions. While some areas boast robust healthcare systems, others struggle with severe shortages, leading to long wait times, limited access to specialists, and compromised patient outcomes. This uneven distribution necessitates a comprehensive understanding of the challenges and contributing factors to effectively address this escalating crisis.
Accessibility Challenges in Primary Care Across the Americas
Patients in the Americas face a wide range of barriers to accessing primary care. Rural and underserved communities often lack sufficient numbers of primary care physicians, resulting in longer travel distances to healthcare facilities and limited access to preventative care. Financial constraints, including high healthcare costs and lack of insurance coverage, also significantly restrict access for many individuals and families.
It’s getting harder and harder to find a doctor’s appointment, a stark reflection of America’s escalating primary care shortage. News that Kaiser Permanente just scrapped plans for a $500 million Seattle bed tower, as reported in this article , only underscores the problem. This decision highlights the financial pressures impacting healthcare expansion, further exacerbating the already dire situation of limited access to primary care for many.
Language barriers and cultural differences can further complicate the patient-physician relationship and hinder effective communication. Additionally, bureaucratic hurdles and complex healthcare systems can create significant delays and frustrations in obtaining necessary care. These challenges disproportionately affect vulnerable populations, including low-income individuals, ethnic minorities, and the elderly.
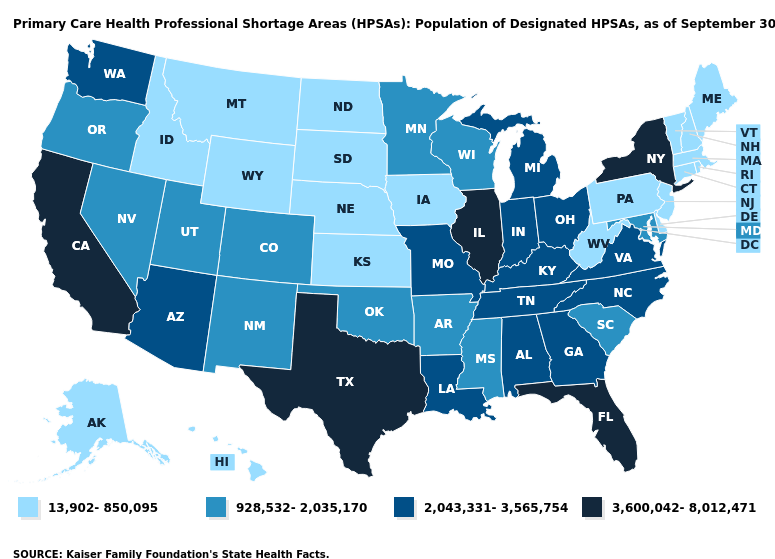
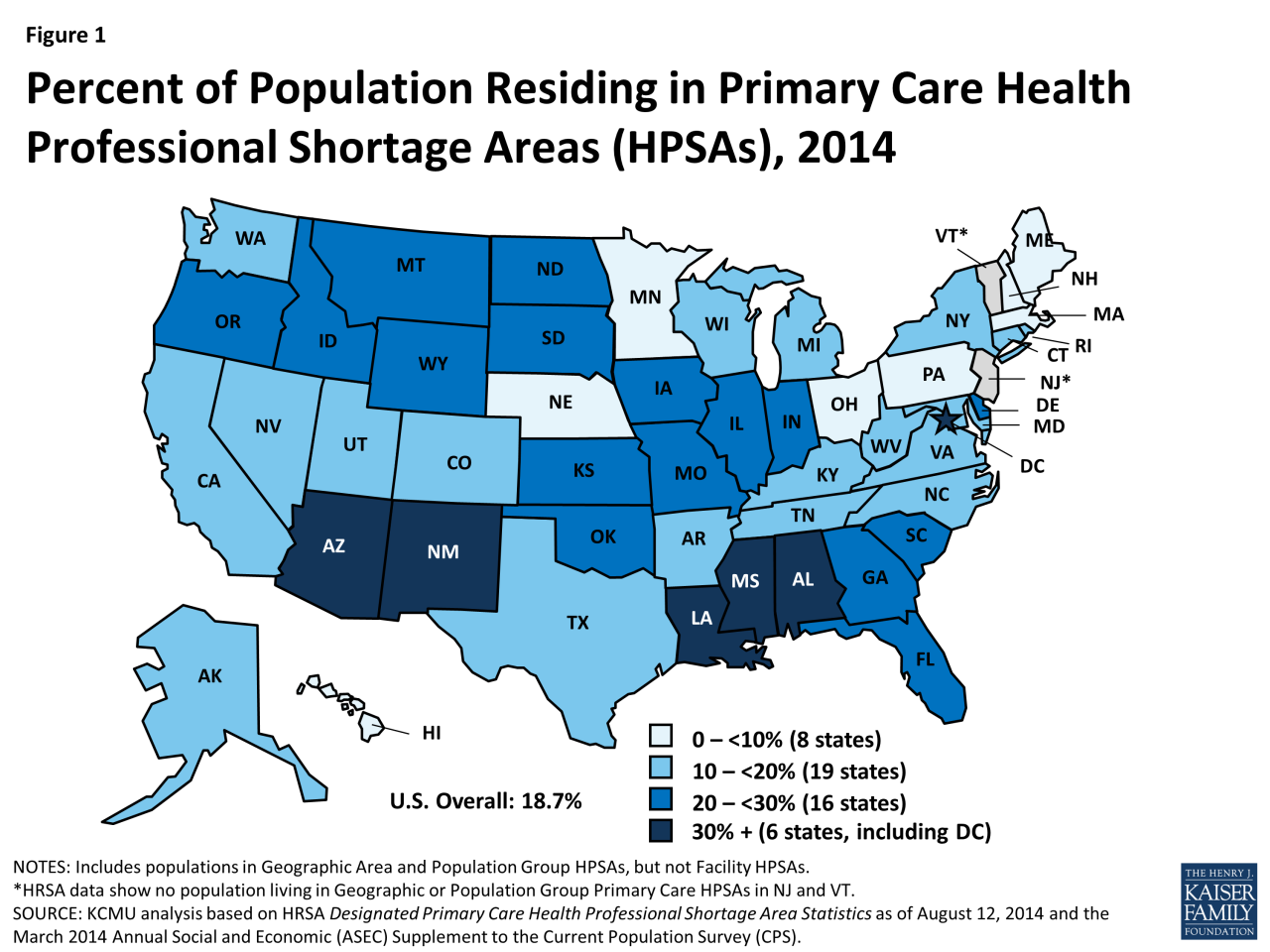
Geographic Distribution of Primary Care Physicians
The geographic distribution of primary care physicians in the Americas is highly uneven. Many urban centers have a relatively high concentration of physicians, while rural and remote areas often suffer from severe shortages. Countries in Central America and the Caribbean frequently experience greater disparities in physician distribution compared to North American nations. This uneven distribution contributes to significant health inequities, as individuals in underserved areas have limited access to preventative care, early diagnosis, and timely treatment.
Consequently, this leads to poorer health outcomes and increased healthcare costs in the long run. For example, vast stretches of the Amazon rainforest in South America have extremely limited access to any medical professionals, let alone primary care physicians.
Contributing Factors to the Primary Care Shortage
Several factors contribute to the escalating primary care shortage across the Americas. Physician burnout, driven by increasing administrative burdens, long working hours, and emotional toll of patient care, is a major concern. The aging population in many American countries increases demand for primary care services, further exacerbating the shortage. Inefficiencies within healthcare systems, including fragmented care models and lack of investment in primary care infrastructure, also play a significant role.
Furthermore, a lack of financial incentives and attractive career paths for aspiring primary care physicians contributes to the problem. The imbalance between the supply of physicians and the growing demand for primary care services creates a critical situation requiring immediate and comprehensive solutions.
Primary Care Access Metrics Across Several Countries in the Americas
| Country | Physician-to-Patient Ratio (per 10,000) | Average Wait Time for Appointment (weeks) | % Population with Health Insurance |
|---|---|---|---|
| United States | 24 | 2-4 | 91% |
| Canada | 28 | 1-3 | 99% |
| Mexico | 16 | 4-8 | 53% |
| Brazil | 18 | 6-12 | 78% |
Note
Data is approximate and may vary depending on the source and specific region within each country. These figures represent general trends and should not be considered definitive. More detailed and regionally specific data is needed for a complete picture.
Impact on Patient Health and Well-being
The escalating primary care shortage in the Americas has profound and far-reaching consequences for patient health and well-being. Delayed or inaccessible primary care leads to a cascade of negative effects, impacting not only individual health outcomes but also placing significant strain on healthcare systems and personal finances. This section will explore the multifaceted ways in which this shortage directly harms patients.The lack of timely access to primary care significantly increases the risk of adverse health outcomes.
Preventive measures are neglected, leading to the worsening of chronic conditions and the delayed diagnosis of serious illnesses. Simple infections can escalate into severe complications, and early detection of cancers and other life-threatening diseases is missed, drastically reducing the chances of successful treatment and survival. This delayed or absent preventative care and early diagnosis directly impacts patient quality of life and longevity.
Delayed Diagnoses and Worsening Chronic Conditions
Delayed diagnoses are a direct consequence of limited access to primary care. Individuals with symptoms may experience prolonged periods of uncertainty and suffering before receiving a proper diagnosis. This delay can lead to more advanced stages of disease, making treatment more complex, less effective, and potentially more costly. For example, a delay in diagnosing diabetes can lead to serious complications like kidney disease, blindness, and heart disease.
Similarly, a delayed diagnosis of cancer can significantly reduce the chances of successful treatment and survival. The consequences of these delays are substantial and often irreversible.
Financial Burden on Patients
The inability to access timely primary care creates a significant financial burden for patients. Without routine check-ups and preventative care, minor health issues can escalate into major crises requiring expensive emergency room visits and hospitalizations. The costs associated with these interventions are far higher than the cost of regular primary care visits. Furthermore, unmanaged chronic conditions can lead to lost productivity due to illness and disability, impacting income and exacerbating financial hardship.
Many patients, particularly those with limited insurance coverage or those uninsured, face catastrophic medical debt due to the lack of accessible primary care.
Illustrative Cases of Negative Impact
Consider the case of Maria, a 60-year-old woman with a history of hypertension. Due to a lack of available appointments, she was unable to get her blood pressure medication refilled for several weeks. This resulted in a hypertensive crisis requiring hospitalization, incurring significant medical expenses and time off from her job. Another example is John, a 45-year-old man who experienced persistent chest pain for months.
Unable to secure a timely appointment with a primary care physician, he eventually ended up in the emergency room with a heart attack, resulting in a prolonged and costly recovery process. These are just two examples of how the primary care shortage has devastating effects on individual patients’ lives.
Hypothetical Case Study: The Garcia Family
The Garcia family, consisting of two working parents and two young children, exemplifies the challenges posed by the primary care shortage. Their primary care physician recently retired, and finding a replacement has proven impossible due to the shortage. The parents struggle to secure appointments for routine check-ups for their children, resulting in missed vaccinations and delayed diagnosis of a minor ear infection in their youngest child which later developed into a more serious issue requiring antibiotics and further medical attention.
The mother has a chronic condition that requires regular monitoring, and without consistent access to her physician, her condition has worsened, leading to increased medical expenses and time off work. The family is now facing substantial financial and emotional strain due to their inability to access timely and adequate primary care.
Contributing Factors
Source: medium.com
The escalating primary care shortage in the Americas is a complex issue stemming from a confluence of systemic, economic, and educational factors that impact physician supply and demand. Understanding these factors is crucial to developing effective solutions to address this critical healthcare challenge. This section will delve into the specifics of physician training, compensation, and the influence of healthcare policy on the distribution of primary care physicians across the region.
Training Pathways and Compensation Models
Significant variations exist in the training pathways and compensation models for primary care physicians across the Americas. In the United States, for example, the path to becoming a primary care physician involves four years of medical school followed by a three-year residency in family medicine, internal medicine, or pediatrics. Compensation for primary care physicians in the US is generally lower compared to specialists, often influenced by factors like reimbursement rates from insurance companies and the relative demand for services.
In contrast, Canada’s system, while also employing a residency model, might offer different financial incentives or loan forgiveness programs that could influence the choice of primary care as a specialty. Countries in Latin America often have different medical school lengths and residency structures, leading to diverse training timelines and ultimately, affecting the number of physicians entering primary care.
Compensation structures vary widely, influenced by both public and private healthcare systems. For instance, some countries might rely more heavily on public funding, leading to potentially lower salaries but greater job security, while others have more market-driven compensation models.
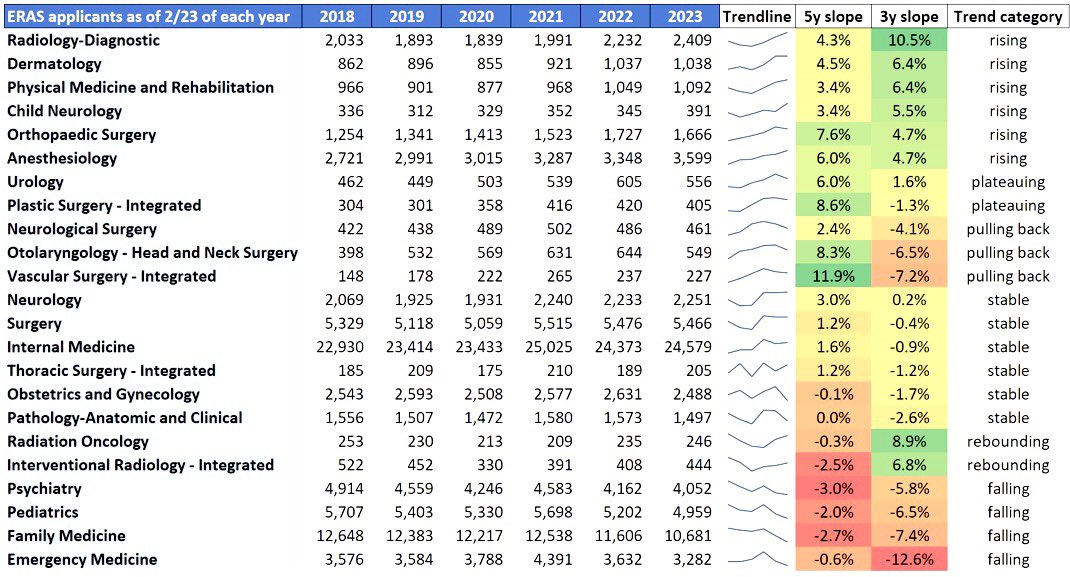
Factors Influencing Specialty Choice, No appointments available americas escalating primary care shortage
Medical students’ decisions to specialize in primary care versus other medical fields are complex and multifaceted. High student loan debt in many countries is a significant deterrent to choosing lower-paying primary care specialties. The perception of long working hours, high patient volume, and comparatively lower prestige compared to specialties like surgery or cardiology also discourages some students. Conversely, factors such as a strong interest in patient relationships, a desire for a more holistic approach to care, and the opportunity for community engagement can attract students to primary care.
The availability of mentorship opportunities from established primary care physicians also plays a crucial role in shaping career aspirations. The prospect of a better work-life balance, while often debated, can also influence the choice of specialty.
Impact of Healthcare Policy and Regulations
Healthcare policies and regulations significantly influence the supply and distribution of primary care physicians. Government funding for medical education, residency training programs, and loan repayment initiatives can directly impact the number of physicians entering primary care. Regulations regarding scope of practice, reimbursement rates, and the licensing of physicians also play a vital role. For instance, policies that restrict the scope of practice for nurse practitioners or physician assistants can increase the demand for primary care physicians, exacerbating the shortage.
Conversely, policies that promote telehealth or allow for broader scope of practice for other healthcare providers could alleviate some of the pressure on primary care physicians. The distribution of physicians is often influenced by geographical location policies, such as incentives for physicians to practice in underserved rural areas.
Categorization of Contributing Factors
The contributing factors to the primary care physician shortage can be categorized as follows:
- Systemic Factors: Uneven distribution of physicians across geographic regions; inadequate infrastructure in rural and underserved areas; bureaucratic hurdles in licensing and credentialing; lack of integration between different levels of care.
- Economic Factors: High medical school debt; lower compensation for primary care physicians compared to specialists; inadequate reimbursement rates from insurance companies; lack of financial incentives for practicing in underserved areas.
- Educational Factors: Limited exposure to primary care during medical school; lack of mentorship opportunities in primary care; perceived lower prestige of primary care compared to other specialties; inadequate training programs in areas of high need.
Potential Solutions and Strategies
The escalating primary care shortage in the Americas demands a multifaceted approach encompassing education, compensation, technology, and policy reform. Addressing this crisis requires innovative strategies that simultaneously increase the number of primary care physicians, improve their working conditions, and enhance patient access to care. The solutions Artikeld below represent a combination of immediate and long-term strategies crucial for building a more resilient and equitable healthcare system.
Expanding Medical Training Programs
Increasing the number of primary care physicians requires a significant expansion of medical training programs focused on primary care. This involves increasing the number of residency slots dedicated to family medicine, general internal medicine, and pediatrics. Furthermore, investments in medical schools and affiliated teaching hospitals are necessary to accommodate this growth. This expansion should also prioritize training programs in underserved rural and urban areas to ensure equitable distribution of physicians.
For example, incentivizing medical students to pursue primary care through loan forgiveness programs or scholarships targeted at students committing to practice in underserved areas could significantly impact physician distribution.
Improving Physician Compensation and Working Conditions
Physician burnout and dissatisfaction are significant contributors to the primary care shortage. Improving compensation and working conditions is essential to attract and retain physicians in primary care. This includes competitive salaries, reduced administrative burdens, and improved work-life balance. Implementing models that reduce the administrative tasks faced by physicians, such as employing dedicated medical assistants to handle paperwork, could dramatically improve job satisfaction.
For instance, the implementation of electronic health record systems that are user-friendly and efficient can significantly reduce physician workload.
Enhancing Telehealth Access
Telehealth offers a powerful tool to expand access to primary care, particularly in rural and underserved areas. Expanding telehealth infrastructure, including broadband access and reimbursement policies that cover telehealth services, is crucial. This includes providing training for physicians on effective telehealth practices and ensuring patient privacy and data security. A successful example of telehealth implementation is the expansion of virtual consultations during the COVID-19 pandemic, which demonstrated the feasibility and effectiveness of telehealth in providing routine primary care.
Government Policies and Healthcare Reforms
Government policies play a critical role in addressing the primary care shortage. This includes increased funding for medical education and training, expansion of health insurance coverage, and implementation of policies that incentivize primary care practice. For example, government initiatives that provide financial incentives for physicians to practice in underserved areas or offer loan repayment programs for those who choose primary care specialties can significantly impact the physician supply in these regions.
Furthermore, reforms that streamline the regulatory process for opening and operating primary care clinics can facilitate the expansion of healthcare access.
Innovative Models of Primary Care Delivery
Team-based care, incorporating nurses, physician assistants, and medical assistants, can significantly improve the efficiency and effectiveness of primary care delivery. This model allows physicians to focus on complex cases while other members of the team handle routine tasks. Community health clinics, located in underserved areas, provide essential primary care services to populations with limited access to healthcare. These clinics often employ a team-based approach and offer a range of services, including preventive care, chronic disease management, and mental health services.
For example, the successful model of community health centers in the United States demonstrates the effectiveness of this approach in improving access to care for vulnerable populations.
Visual Representation: Implementation of Team-Based Care
Imagine a flowchart. The starting point is a patient seeking primary care. The first step involves a triage system, managed by a nurse or medical assistant, who assesses the patient’s needs and determines the appropriate level of care. Simple issues, like prescription refills or follow-up on chronic conditions, are handled by the nurse or medical assistant. More complex cases are then routed to a physician.
This system reduces physician workload by delegating routine tasks, allowing physicians to focus on patients requiring specialized attention. The impact is visualized by two separate columns: one showing the pre-implementation scenario with long wait times and high physician workload, represented by overflowing inboxes and a stressed physician icon; the other showing the post-implementation scenario with shorter wait times, efficient workflow, and a less stressed physician icon with a manageable workload, all illustrated by improved patient flow and less cluttered inboxes.
The overall effect is improved patient access, reduced wait times, and increased physician satisfaction, leading to better quality of care.
The Role of Technology and Telehealth
Source: twimg.com
The escalating primary care shortage in the Americas demands innovative solutions, and telehealth emerges as a powerful tool to bridge the access gap and improve patient outcomes. By leveraging technology, we can extend the reach of healthcare providers, particularly to underserved populations in rural and remote areas, where access to in-person care is severely limited. This exploration delves into how telehealth can reshape primary care delivery, examining its advantages, limitations, and practical implementation strategies.Telehealth’s Capacity to Enhance Primary Care Access in Underserved AreasTelehealth offers a compelling solution for overcoming geographical barriers to primary care.
It’s getting harder and harder to find a doctor’s appointment, a symptom of America’s escalating primary care shortage. This crisis is only worsened by hospital closures, like the recent news about Steward Health Care; check out this article on steward ohio hospitals closures pennsylvania facility at risk to see what I mean. Fewer hospitals directly translate to fewer doctors and even longer wait times for patients already struggling to access basic care.
High-speed internet access, although not universally available, is steadily expanding, enabling virtual consultations, remote monitoring, and other telehealth services to reach individuals in previously inaccessible areas. For instance, a telehealth program in rural Montana successfully reduced wait times for specialist consultations by connecting patients with specialists located in urban centers via video conferencing. This allowed patients to receive timely care without the need for lengthy and expensive travel.
Furthermore, telehealth can improve access for patients with mobility limitations or those living in areas with limited public transportation.Benefits and Limitations of Telehealth in Addressing the Primary Care ShortageThe benefits of using telehealth to address the primary care shortage are multifaceted. It increases the efficiency of healthcare providers by allowing them to see more patients in a given timeframe.
It also expands the reach of specialists, making their expertise available to a wider patient population. Reduced travel time and costs for patients are significant advantages, leading to improved adherence to treatment plans. However, limitations exist. The digital divide – unequal access to technology and reliable internet – presents a major hurdle. Furthermore, telehealth may not be suitable for all patients, particularly those with complex medical needs requiring hands-on examination.
The effectiveness of telehealth also depends heavily on the quality of the technology and the training of healthcare providers in its use. Concerns around data privacy and security must also be addressed.Telehealth Models and Their SuitabilityVarious telehealth models cater to different needs and settings. Store-and-forward telehealth involves the transmission of patient data (e.g., medical images) to a specialist for review.
This model is well-suited for situations where immediate interaction isn’t necessary. Real-time telehealth, on the other hand, involves live video conferencing between patients and providers, ideal for consultations and follow-ups. Remote patient monitoring (RPM) uses wearable sensors and other devices to collect patient data, enabling proactive intervention and management of chronic conditions. The choice of model depends on factors such as the type of care required, the patient’s technological literacy, and the availability of resources.
For instance, RPM might be particularly beneficial for managing chronic conditions like diabetes in rural settings, while real-time video consultations are suitable for routine primary care visits.Implementing a Telehealth System to Address the Primary Care Shortage in a Specific RegionA step-by-step guide for implementing a telehealth system in a specific region, say, a rural county in Arizona, might look like this:
1. Needs Assessment
Conduct a thorough assessment to identify the specific primary care needs of the population and the existing healthcare infrastructure. This includes identifying areas with limited access to care, the types of services most needed, and the technological capabilities of the community.
2. Technology Selection
Choose appropriate telehealth technology based on the needs assessment. This might involve selecting video conferencing platforms, remote patient monitoring devices, and electronic health record (EHR) systems that are compatible and secure.
3. Provider Training
Train healthcare providers on the use of the selected technology and the protocols for providing telehealth services. This includes training on patient communication, data security, and the management of remote patient monitoring data.
4. Patient Education
It’s getting harder and harder to snag a doctor’s appointment these days, a stark reminder of America’s escalating primary care shortage. This crisis highlights the urgent need for innovative solutions, and I was intrigued by this article on reimagining collaboration in senior care a technology-driven approach , which suggests tech could help streamline healthcare access. Perhaps similar tech could help alleviate the pressure on primary care physicians and get more people the appointments they desperately need.
Educate patients on how to use the telehealth system, including how to access services, participate in virtual consultations, and use remote patient monitoring devices.
5. Infrastructure Development
Invest in expanding broadband internet access in underserved areas to ensure reliable connectivity for both providers and patients. This might involve partnerships with local internet service providers or government initiatives.
6. Integration with Existing Healthcare Systems
Integrate the telehealth system with existing healthcare systems to ensure seamless data sharing and coordination of care. This involves establishing secure data transfer protocols and ensuring interoperability between different systems.
7. Ongoing Monitoring and Evaluation
Continuously monitor and evaluate the effectiveness of the telehealth system, making adjustments as needed to optimize its performance and address any challenges. This includes tracking key metrics such as patient satisfaction, access to care, and health outcomes.
Final Summary: No Appointments Available Americas Escalating Primary Care Shortage
Source: kff.org
The primary care shortage in the Americas isn’t just a statistic; it’s a human story of struggle and resilience. While the challenges are immense, the potential for positive change is equally significant. By addressing physician burnout, investing in healthcare infrastructure, and embracing innovative solutions like telehealth, we can begin to alleviate this crisis and ensure that everyone has access to the essential primary care they need to thrive.
The path forward requires collaboration, innovation, and a commitment to prioritizing the health and well-being of communities across the Americas. Let’s work together to fill those empty appointment slots.
Query Resolution
What are the long-term effects of delayed primary care?
Delayed primary care can lead to worsened chronic conditions, increased risk of complications, and even premature death. Early detection and management of health issues are crucial for better outcomes.
How can I find a primary care physician even with the shortage?
Check your insurance provider’s directory, search online for local clinics, and consider using telehealth services to expand your options. Be persistent and patient in your search.
Is the shortage impacting specific demographics more than others?
Yes, underserved communities, rural populations, and low-income individuals often face disproportionately greater challenges accessing primary care.
What role do preventative care measures play in this crisis?
Investing in preventative care reduces the burden on the system by preventing many health issues from escalating and requiring more expensive interventions later.