What is Grade 3 Fatty Liver and How to Manage It?
What is grade 3 fatty liver and how to manage it? That’s the burning question many face when diagnosed with this serious condition. Grade 3 fatty liver disease represents the most advanced stage of non-alcoholic fatty liver disease (NAFLD), where a significant portion of your liver is infiltrated with fat, impacting its function. This isn’t just about a few extra pounds; it’s about potential long-term health consequences, ranging from liver failure to cirrhosis.
Understanding the causes, diagnosis, and, most importantly, the management strategies is crucial for improving your prognosis and overall well-being. Let’s dive in and explore how you can take control of your liver health.
This post will cover everything from the defining characteristics of grade 3 fatty liver disease and its comparison to earlier stages, to the detailed causes, including lifestyle factors and underlying medical conditions. We’ll explore diagnostic methods, a comprehensive management plan (including a sample meal plan!), lifestyle modifications, medical treatments, and the importance of monitoring and follow-up care. We’ll even look at a hypothetical patient journey to illustrate the realities of living with and managing this condition.
Ready to learn more? Let’s get started!
Definition of Grade 3 Fatty Liver Disease
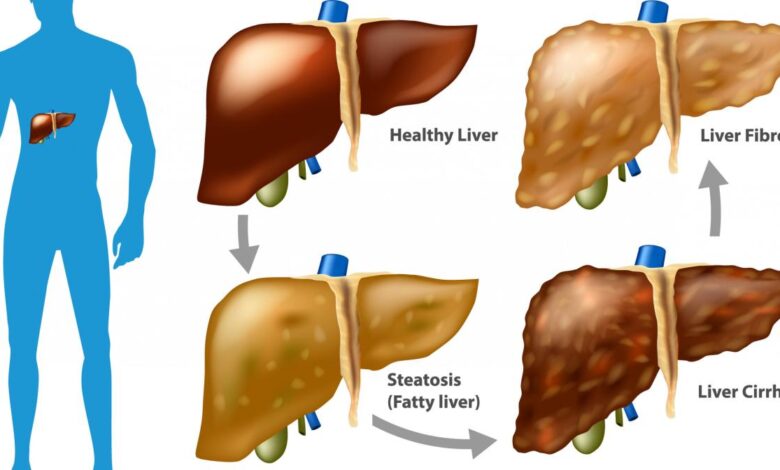
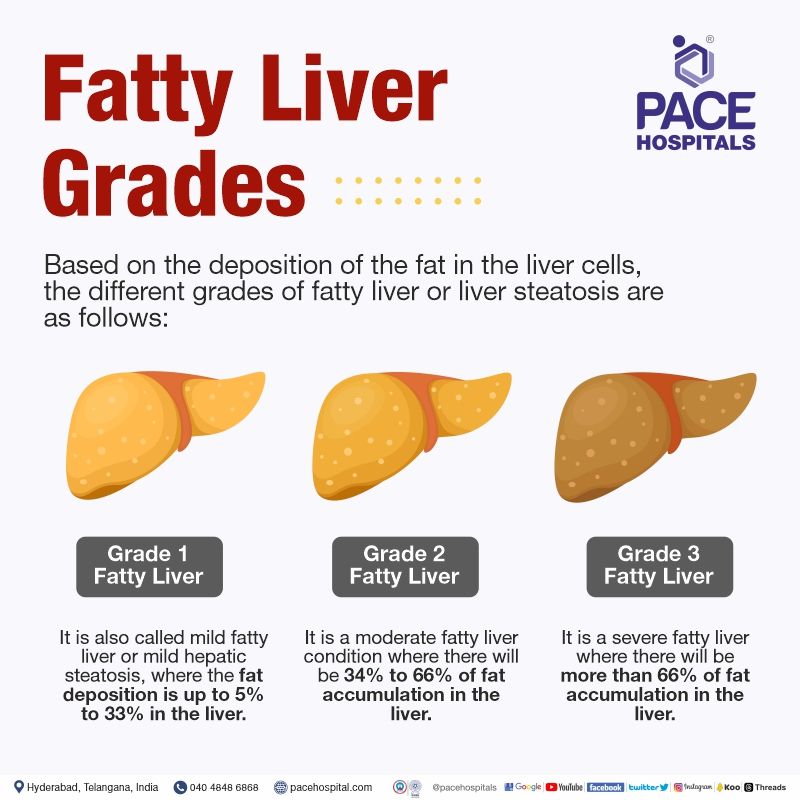
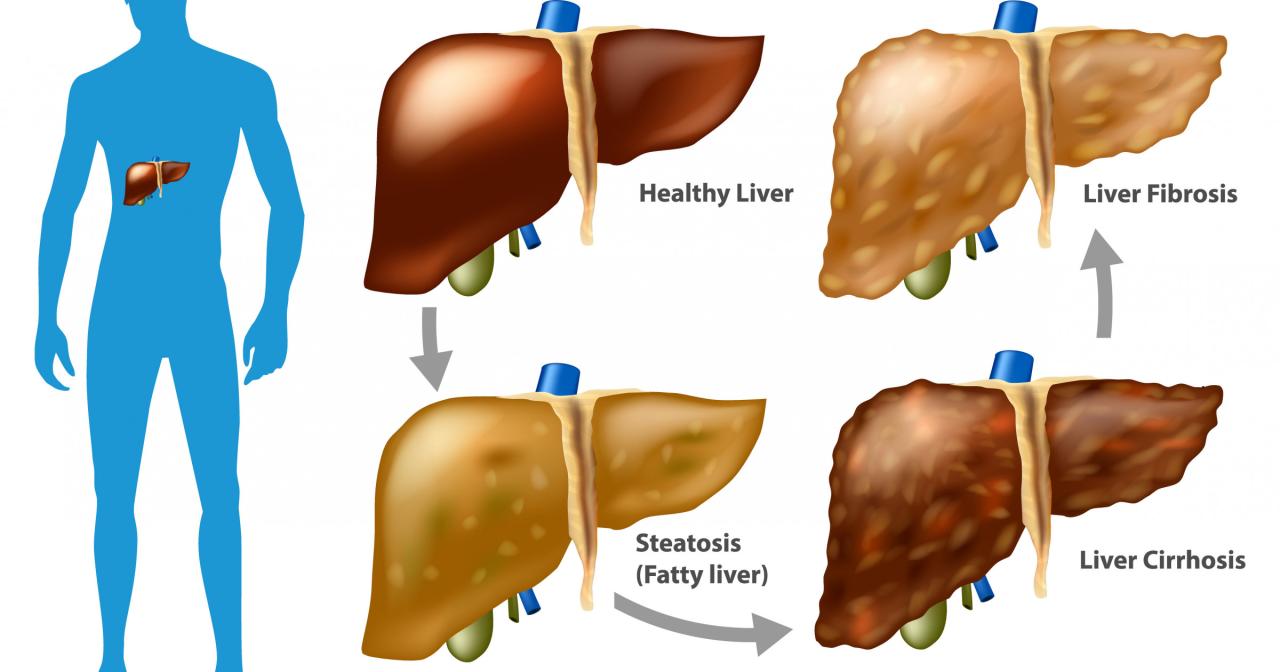
Grade 3 fatty liver disease, also known as severe non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH), represents the most advanced stage of fat accumulation in the liver. It signifies significant damage beyond simple fat buildup, indicating the presence of inflammation, cell death, and fibrosis (scarring) within the liver tissue. This stage carries substantial health risks and requires careful medical management.Grade 3 fatty liver disease is characterized by extensive fat infiltration exceeding 66% of the liver, along with significant inflammation and fibrosis.
Microscopically, hepatocytes (liver cells) show ballooning degeneration, indicating cellular injury and death. The liver’s architecture is significantly disrupted by the presence of fibrous tissue, leading to a hardened and less functional organ. This fibrosis is a critical factor, as it can progress to cirrhosis, a late-stage liver disease where the liver is severely scarred and unable to function properly.
Grade 3 fatty liver is serious, requiring lifestyle changes like diet and exercise. Managing it effectively is crucial because conditions like this often share risk factors with other serious health problems, including stroke; understanding the risk factors that make stroke more dangerous helps highlight the importance of proactive health management. Therefore, tackling grade 3 fatty liver head-on is vital for overall well-being and reducing the risk of related complications.
Comparison with Earlier Stages
In contrast to earlier stages of NAFLD (grades 1 and 2), grade 3 shows a dramatic increase in both fat accumulation and liver damage. Grade 1 NAFLD exhibits mild fat accumulation with minimal inflammation, while grade 2 demonstrates a moderate increase in fat and some inflammation. Grade 3, however, is marked by substantial fat infiltration, pronounced inflammation, and significant fibrosis, indicating a much more serious condition requiring aggressive intervention.
The progression from grade 1 to grade 3 is not necessarily linear; some individuals may experience rapid progression, while others may remain in earlier stages for extended periods.
Potential Health Risks Associated with Grade 3 Fatty Liver Disease
The advanced nature of grade 3 fatty liver disease poses several significant health risks. The most concerning is the progression to cirrhosis, a condition where scar tissue replaces healthy liver tissue, impairing liver function. Cirrhosis can lead to liver failure, requiring a liver transplant. Further complications associated with grade 3 NAFLD include:
- Portal hypertension: Increased pressure in the portal vein, which can lead to esophageal varices (swollen veins in the esophagus), increasing the risk of bleeding.
- Hepatocellular carcinoma (HCC): Liver cancer. Cirrhosis significantly increases the risk of developing HCC.
- Ascites: Accumulation of fluid in the abdominal cavity.
- Hepatic encephalopathy: A neurological disorder caused by the buildup of toxins in the blood due to liver failure.
- Jaundice: Yellowing of the skin and eyes due to bilirubin buildup.
The severity of these complications varies depending on the extent of liver damage and the individual’s overall health. Early detection and management are crucial to minimize the risk of these life-threatening complications. For example, a patient with grade 3 NAFLD might experience fatigue, abdominal pain, and unexplained weight loss, prompting medical investigation and ultimately leading to a diagnosis.
Without intervention, these symptoms could progress to more severe manifestations like ascites or hepatic encephalopathy.
Causes of Grade 3 Fatty Liver Disease
Grade 3 fatty liver disease, the most severe form of non-alcoholic fatty liver disease (NAFLD), doesn’t appear overnight. It’s the culmination of various factors, often interacting in complex ways, that gradually damage the liver. Understanding these causes is crucial for prevention and effective management.
The primary drivers of grade 3 NAFLD are a combination of lifestyle choices and underlying health conditions. While genetics play a role, lifestyle modifications often significantly impact the disease’s progression. Let’s delve into the specific contributors.
Lifestyle Factors and Grade 3 NAFLD
Lifestyle significantly influences the development and progression of grade 3 fatty liver disease. Unhealthy habits often act synergistically, accelerating liver damage.
Dietary factors play a central role. A diet high in saturated and trans fats, refined carbohydrates, and fructose (found in sugary drinks and processed foods) contributes to excess fat accumulation in the liver. Conversely, a diet rich in fruits, vegetables, whole grains, and lean proteins supports liver health. For example, consistently consuming fast food and sugary sodas increases the risk considerably compared to a balanced diet emphasizing whole, unprocessed foods.
Lack of physical activity exacerbates the problem. Exercise helps regulate metabolism, reducing fat accumulation in the liver and improving insulin sensitivity. Individuals leading sedentary lives are at a much higher risk of developing NAFLD, and the severity tends to be greater in those who are completely inactive. Regular exercise, even moderate activity like brisk walking for 30 minutes most days of the week, can make a noticeable difference.
Excessive alcohol consumption is a major risk factor for alcoholic fatty liver disease (AFLD), a closely related condition. While NAFLD is specifically
-non-alcoholic*, even moderate alcohol intake can worsen existing NAFLD and accelerate its progression to grade 3. Chronic heavy drinking significantly increases the likelihood of developing severe liver damage.
So, you’re wondering about grade 3 fatty liver and how to manage it? It’s a serious condition requiring lifestyle changes like diet and exercise. Interestingly, research is exploring links between overall health and other conditions, like I recently read an article on how can eye test detect dementia risk in older adults , highlighting the interconnectedness of our systems.
Getting a handle on your liver health is crucial, and that often includes addressing underlying metabolic issues. Remember to consult your doctor for personalized advice on managing grade 3 fatty liver disease.
Underlying Medical Conditions and Grade 3 NAFLD
Several medical conditions significantly increase the risk of developing grade 3 NAFLD or contribute to its worsening. These conditions often share underlying metabolic disturbances that promote fat accumulation in the liver.
Type 2 diabetes is strongly associated with NAFLD. Insulin resistance, a hallmark of type 2 diabetes, impairs the liver’s ability to process fats, leading to increased fat storage. This is why individuals with poorly controlled diabetes are at substantially increased risk for advanced stages of NAFLD, including grade 3. Effective diabetes management is vital in mitigating this risk.
Obesity, particularly abdominal obesity (excess fat around the waist), is another significant risk factor. Excess visceral fat releases fatty acids into the bloodstream, overwhelming the liver’s capacity to metabolize them. This leads to a build-up of fat within the liver cells, triggering inflammation and damage. Weight loss, even modest amounts, can significantly improve liver health in obese individuals with NAFLD.
Other conditions, such as metabolic syndrome (a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels), dyslipidemia (abnormal lipid levels), and polycystic ovary syndrome (PCOS), also increase the risk of developing grade 3 NAFLD. These conditions often share underlying metabolic imbalances that contribute to the development of fatty liver disease.
Diagnosis of Grade 3 Fatty Liver Disease
Diagnosing grade 3 fatty liver disease, a severe form of non-alcoholic fatty liver disease (NAFLD), requires a multi-pronged approach combining medical history, physical examination, blood tests, and imaging techniques. The goal is not only to confirm the presence of significant fat accumulation in the liver but also to assess the extent of liver damage and rule out other potential causes.
Blood Tests
Blood tests play a crucial role in the initial assessment and ongoing monitoring of grade 3 fatty liver disease. These tests help evaluate liver function, identify potential complications, and screen for other conditions that might mimic the symptoms of NAFLD. Abnormal results, however, don’t definitively diagnose grade 3; further investigation is necessary.
- Liver function tests (LFTs): These tests measure the levels of enzymes released by the liver into the bloodstream. Elevated levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) can indicate liver damage, but the degree of elevation doesn’t always correlate with the severity of fatty liver disease. Other LFTs, such as alkaline phosphatase (ALP) and bilirubin, provide additional information about liver function.
For example, a patient with grade 3 fatty liver might present with significantly elevated ALT and AST levels, perhaps 3-5 times the upper limit of normal, indicating substantial liver cell injury.
- Lipid profile: This panel assesses cholesterol and triglyceride levels, which are often elevated in individuals with NAFLD. High levels of triglycerides are particularly associated with increased fat accumulation in the liver. For instance, a patient might have a triglyceride level of 300 mg/dL or higher, contributing to the diagnosis.
- Other blood tests: Additional tests may be ordered to rule out other causes of liver disease, including viral hepatitis, autoimmune hepatitis, and hemochromatosis. These might include tests for viral markers, autoantibodies, and iron levels.
Imaging Techniques
Imaging techniques are essential for visualizing the liver and assessing the extent of fat accumulation and any associated liver damage. These tests provide a visual representation of the liver’s structure and help determine the severity of the disease.
- Ultrasound: This non-invasive and readily available technique is often the first imaging test performed. Ultrasound can detect increased echogenicity (brightness) of the liver, indicating fat accumulation. However, ultrasound alone cannot reliably differentiate between different grades of fatty liver disease. A grade 3 liver on ultrasound would appear significantly brighter than a normal liver, often described as having a hyperechoic appearance.
- Computed tomography (CT) scan: CT scans provide more detailed images of the liver than ultrasound, although they involve exposure to ionizing radiation. CT scans can help assess the extent of fatty infiltration and identify other liver abnormalities, such as fibrosis (scarring) or masses. In a grade 3 fatty liver, the CT scan would likely show diffusely increased liver density, reflecting the high fat content.
- Magnetic resonance imaging (MRI): MRI offers superior soft tissue contrast and doesn’t involve ionizing radiation. Specific MRI techniques, such as proton density fat fraction (PDFF) measurement, can quantitatively assess the percentage of fat in the liver, providing a more precise assessment of the severity of fatty liver disease. A high PDFF value would be consistent with grade 3 fatty liver disease.
Interpretation of Results Indicating Grade 3 Fatty Liver Disease
The diagnosis of grade 3 fatty liver disease is typically made based on a combination of clinical findings, blood test results, and imaging studies. The presence of significant fat accumulation in the liver (demonstrated by imaging), along with elevated liver enzymes and other risk factors (such as obesity, diabetes, and dyslipidemia), strongly supports the diagnosis. The specific interpretation of results depends on the individual patient’s clinical presentation and the results of all the tests.
For example, a combination of markedly elevated ALT and AST levels, a hyperechoic liver on ultrasound, and a high PDFF value on MRI would strongly suggest grade 3 fatty liver disease. The severity of liver damage (fibrosis) is often assessed through liver biopsy, although this is becoming less common with the advancements in non-invasive techniques.
Management Strategies for Grade 3 Fatty Liver Disease
Grade 3 fatty liver disease, characterized by significant fat accumulation in the liver, necessitates a comprehensive management plan focusing on lifestyle modifications and, in some cases, medical interventions. The goal is to reduce liver fat, improve liver function, and prevent the progression to more severe liver diseases like cirrhosis. This requires a committed approach involving dietary changes, increased physical activity, and potentially medication.
A Step-by-Step Guide to Managing Grade 3 Fatty Liver Disease
Managing grade 3 fatty liver disease is a journey, not a sprint. It requires consistent effort and a multi-pronged approach. The following table Artikels key interventions, their benefits, and potential side effects. Remember to consult your healthcare provider before starting any new treatment plan.
| Intervention | Description | Benefits | Potential Side Effects |
|---|---|---|---|
| Dietary Changes | Reducing overall calorie intake, focusing on a balanced diet rich in fruits, vegetables, whole grains, and lean protein. Limiting saturated and trans fats, refined carbohydrates, and added sugars. | Weight loss, reduced liver fat, improved insulin sensitivity, better blood sugar control. | Nutrient deficiencies if not carefully planned, initial hunger pangs, potential for disordered eating if not approached thoughtfully. |
| Weight Loss | Achieving and maintaining a healthy weight through a combination of diet and exercise. Even modest weight loss can significantly improve liver health. | Reduced liver fat, improved liver function, decreased risk of liver disease progression. | Fatigue, muscle loss (if weight loss is too rapid or extreme), potential for nutritional deficiencies. |
| Regular Exercise | Engaging in at least 150 minutes of moderate-intensity aerobic exercise per week, along with strength training exercises twice a week. | Weight loss, improved insulin sensitivity, increased energy levels, improved cardiovascular health. | Muscle soreness, joint pain (initially), risk of injury if not done properly. |
| Medication | Certain medications, such as vitamin E or medications to manage underlying conditions like diabetes or high cholesterol, may be prescribed. | Improved liver function, reduced inflammation, management of associated conditions. | Various side effects depending on the specific medication, ranging from mild to severe. Always discuss potential side effects with your doctor. |
| Alcohol Avoidance | Complete abstinence from alcohol is crucial, as alcohol consumption exacerbates liver damage. | Reduced liver inflammation, improved liver function, prevention of further liver damage. | Withdrawal symptoms (if a heavy drinker) requiring medical supervision. |
Sample Meal Plan for Grade 3 Fatty Liver Disease
This is a sample meal plan and should be adapted to individual needs and preferences. Consult a registered dietitian or nutritionist for personalized guidance. Portion sizes should be adjusted based on individual caloric needs.
Day 1
Breakfast: Oatmeal with berries and a sprinkle of nuts.
Lunch: Salad with grilled chicken or fish, mixed greens, and a light vinaigrette.
Dinner: Baked salmon with roasted vegetables (broccoli, carrots, peppers).
Snacks: A handful of almonds, a piece of fruit (apple, banana).
Day 2
Breakfast: Scrambled eggs with whole-wheat toast and avocado.
Lunch: Lentil soup with a side salad.
Dinner: Chicken stir-fry with brown rice and plenty of vegetables.
Snacks: Greek yogurt, a small portion of air-popped popcorn.
Day 3
Breakfast: Whole-wheat pancakes with fruit and a small amount of maple syrup.
Lunch: Turkey breast sandwich on whole-wheat bread with lettuce and tomato.
Dinner: Vegetarian chili with a side of brown rice.
Snacks: Baby carrots and hummus, a small orange.
Lifestyle Modifications for Grade 3 Fatty Liver Disease: What Is Grade 3 Fatty Liver And How To Manage
Source: cdn-website.com
Living with grade 3 fatty liver disease requires a significant commitment to lifestyle changes. These modifications aren’t just about managing symptoms; they’re about actively reversing the damage and improving your overall health. The good news is that even small, consistent changes can make a big difference in the long run. This section focuses on dietary adjustments, physical activity recommendations, and the crucial role of weight management.
Dietary Changes to Improve Liver Health
Adopting a healthy diet is paramount in managing grade 3 fatty liver disease. The goal is to reduce inflammation, improve liver function, and support overall weight loss. Focusing on nutrient-rich foods and limiting those that put extra strain on your liver is key.
- Reduce saturated and trans fats: These fats are found in red meat, processed foods, and fried foods. Replacing them with unsaturated fats from sources like avocados, nuts, and olive oil is beneficial.
- Limit added sugars and refined carbohydrates: Sugary drinks, pastries, and white bread contribute to weight gain and worsen liver inflammation. Opt for whole grains, fruits, and vegetables instead.
- Increase fiber intake: Fiber promotes healthy digestion and helps regulate blood sugar levels. Good sources include fruits, vegetables, and whole grains.
- Consume lean protein: Lean protein sources, such as fish, poultry, and beans, support liver repair and help maintain muscle mass.
- Choose healthy fats: Unsaturated fats from sources like olive oil, avocados, nuts, and seeds are beneficial for overall health and liver function.
Recommendations for Increasing Physical Activity Levels, What is grade 3 fatty liver and how to manage
Regular physical activity plays a vital role in managing grade 3 fatty liver disease. Exercise helps with weight loss, improves insulin sensitivity, and reduces inflammation. It’s crucial to start slowly and gradually increase intensity and duration.
- Aim for at least 150 minutes of moderate-intensity aerobic exercise per week: This could include brisk walking, cycling, or swimming. Break it up into smaller sessions if needed.
- Incorporate strength training exercises twice a week: Strength training helps build muscle mass, which boosts metabolism and improves overall health. Focus on major muscle groups.
- Find activities you enjoy: This is key to maintaining consistency. Whether it’s dancing, hiking, or gardening, choose activities that keep you motivated.
- Consult your doctor before starting any new exercise program: This is especially important if you have any underlying health conditions.
Weight Management in Grade 3 Fatty Liver Disease
Weight loss is often a critical component of managing grade 3 fatty liver disease. Even a modest weight reduction can significantly improve liver health. This is because excess weight contributes to the accumulation of fat in the liver.
Losing even 5-10% of your body weight can make a substantial difference in reducing liver fat and improving liver function.
The approach to weight loss should be gradual and sustainable. Combining a healthy diet with regular exercise is the most effective strategy. Consider working with a registered dietitian or a healthcare professional to develop a personalized weight management plan. This plan should consider your individual needs, preferences, and any other health conditions you might have. Remember that rapid weight loss is generally not recommended and can be detrimental to your health.
Medical Treatments for Grade 3 Fatty Liver Disease
Grade 3 fatty liver disease, representing significant liver damage, often necessitates medical intervention beyond lifestyle changes. Treatment focuses on addressing underlying causes and managing associated complications to slow disease progression and prevent serious consequences like cirrhosis or liver failure. The approach is highly individualized, depending on the patient’s overall health, the severity of their liver disease, and the presence of other conditions.
Medications for Managing Underlying Conditions
Effective management of grade 3 fatty liver disease frequently involves treating co-existing conditions that contribute to its development. These conditions often include type 2 diabetes, high cholesterol, and high blood pressure. Addressing these issues directly can significantly improve liver health.
Grade 3 fatty liver is serious, requiring significant lifestyle changes. Managing it effectively often involves a tailored diet, and understanding nutritional needs is key. This is where the article on are women and men receptive of different types of food and game changing superfoods for women becomes relevant, as dietary choices are crucial. Focusing on the right foods, as highlighted in the article, can significantly support recovery and prevent further liver damage.
- Diabetes Management: Medications like metformin, insulin, or other glucose-lowering agents are crucial for controlling blood sugar levels. Well-controlled blood sugar reduces fat accumulation in the liver and minimizes inflammation. For example, a patient with poorly controlled type 2 diabetes might experience a significant reduction in liver fat percentage after several months of consistent metformin therapy, combined with dietary changes.
- Lipid-Lowering Therapy: Statins, fibrates, or other cholesterol-lowering drugs can help reduce high cholesterol and triglyceride levels. High levels of these fats contribute to liver damage. A patient with high LDL cholesterol (bad cholesterol) and triglycerides might see a decrease in liver fat and improvement in liver enzyme levels after initiating statin therapy, combined with lifestyle modifications.
- Blood Pressure Management: Medications such as ACE inhibitors, angiotensin receptor blockers (ARBs), or diuretics help manage hypertension. High blood pressure can exacerbate liver damage. A patient with high blood pressure who begins taking an ACE inhibitor may experience a decrease in blood pressure, leading to reduced stress on the liver and a potential slowing of disease progression.
Specific Medications for Liver Health
While there isn’t a medication that directly reverses grade 3 fatty liver disease, some medications show promise in improving liver function and reducing inflammation. The choice of medication depends on individual circumstances and the presence of other health problems.
- Pentoxifylline: This medication improves blood flow to the liver, potentially reducing inflammation and improving liver function. However, its effectiveness in grade 3 fatty liver disease is still under investigation and results can be variable.
- Vitamin E: High doses of vitamin E have shown some benefit in reducing liver inflammation and improving liver enzymes in certain patients with non-alcoholic steatohepatitis (NASH), a more severe form of fatty liver disease. However, it’s not suitable for all patients, especially those with bleeding disorders or other contraindications. The effectiveness of Vitamin E also varies considerably between individuals.
- Other Investigational Drugs: Several new medications are under investigation for their potential to treat NASH and reduce fibrosis (scarring) in the liver. These include drugs targeting specific pathways involved in liver inflammation and fat accumulation. Examples include FXR agonists and GLP-1 receptor agonists, which are showing promise in clinical trials but are not yet widely available for routine use in grade 3 fatty liver disease.
The Role of Weight Loss in Treatment
Significant weight loss, even modest amounts, can often be the most effective treatment for grade 3 fatty liver disease. This is because weight loss directly addresses the underlying cause of fat accumulation in the liver. While medication can help manage associated conditions, weight loss is often the cornerstone of treatment and frequently leads to improvements in liver function tests and reduces the risk of disease progression.
The success of weight loss interventions depends on factors such as the individual’s adherence to the diet plan and the chosen method of weight loss (e.g., diet, exercise, or bariatric surgery).
Monitoring and Follow-up Care
Regular monitoring is crucial for effectively managing grade 3 fatty liver disease. Consistent check-ups allow healthcare providers to track disease progression, assess the effectiveness of treatment, and make necessary adjustments to the management plan. This proactive approach helps prevent complications and improve long-term outcomes.Effective management of grade 3 fatty liver disease requires a commitment to regular follow-up appointments.
These appointments provide opportunities for ongoing assessment and adjustments to the treatment strategy. Failure to attend these appointments can lead to missed opportunities for early intervention and potentially more serious health consequences.
Frequency and Types of Follow-up Appointments
The frequency of follow-up appointments varies depending on individual circumstances, including the severity of the disease, the presence of complications, and the patient’s response to treatment. Generally, initial appointments may be more frequent, perhaps every few months, to closely monitor progress and make any needed adjustments. As the condition stabilizes, appointments might become less frequent, perhaps annually or even biannually, provided the patient maintains good health and adheres to the treatment plan.
These appointments typically involve a combination of physical examinations, blood tests (to assess liver function, cholesterol levels, and blood sugar), and imaging studies (such as ultrasound or MRI) to evaluate liver health. In some cases, a liver biopsy might be repeated to monitor the extent of liver damage.
Importance of Adherence to the Prescribed Treatment Plan
Strict adherence to the prescribed treatment plan is paramount for successful management of grade 3 fatty liver disease. This includes diligently following lifestyle modifications, such as dietary changes and regular exercise, as well as taking any prescribed medications as directed. Non-compliance can hinder treatment effectiveness, potentially leading to disease progression and the development of serious complications, such as cirrhosis or liver failure.
For example, a patient prescribed medication to manage high cholesterol but fails to take it regularly may experience a worsening of their liver condition due to continued high cholesterol levels. Similarly, a patient who does not adhere to a recommended low-fat diet risks increasing their liver fat content, thereby hindering their progress. Open communication with the healthcare provider is essential to address any challenges in adhering to the treatment plan and to explore strategies for improved compliance.
This might involve discussing potential barriers to adherence and developing realistic and sustainable strategies to overcome them.
Illustrative Example of Grade 3 Fatty Liver
Let’s consider the case of Sarah, a 48-year-old woman who presented with persistent fatigue, abdominal discomfort, and a feeling of fullness even after small meals. These symptoms had been gradually worsening over the past two years, coinciding with a significant weight gain and lifestyle changes.Sarah’s medical history revealed a family history of type 2 diabetes and hypertension. She admitted to a diet high in processed foods, sugary drinks, and saturated fats, coupled with a sedentary lifestyle.
Physical examination revealed hepatomegaly (enlarged liver), and blood tests showed elevated liver enzymes (AST and ALT), along with high cholesterol and triglyceride levels. An abdominal ultrasound confirmed the presence of significant fatty infiltration of the liver, consistent with grade 3 fatty liver disease.
Sarah’s Liver Appearance
Imagine Sarah’s liver. Instead of its normal reddish-brown, smooth surface, it appeared enlarged and pale, almost yellowish in color. The texture was noticeably firmer than a healthy liver, and the surface felt somewhat irregular, indicating significant fat accumulation throughout the organ. This fatty infiltration has disrupted the liver’s normal architecture and function.
Sarah’s Diagnostic Journey
The diagnosis of grade 3 fatty liver disease was made based on the combination of her symptoms, physical examination findings, abnormal blood tests, and the ultrasound results. Further investigations, such as a liver biopsy, were not deemed necessary in her case given the clear imaging findings and clinical picture.
Sarah’s Treatment and Management
Sarah’s treatment plan focused on lifestyle modifications and medical management. She started a comprehensive weight-loss program with a registered dietitian, focusing on a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, while eliminating processed foods, sugary drinks, and saturated fats. She also began a regular exercise program, starting with moderate-intensity activities like brisk walking and gradually increasing the intensity and duration.
Her physician prescribed medication to help manage her elevated cholesterol and triglyceride levels. Regular monitoring of her liver enzymes, weight, and overall health was scheduled to track her progress and adjust the treatment plan as needed. She was also educated on the importance of alcohol avoidance, given its potential to exacerbate liver damage.
Final Review
Source: poz.com
Navigating a grade 3 fatty liver diagnosis can feel overwhelming, but remember you’re not alone. By understanding the complexities of this condition and actively engaging in a comprehensive management plan, you can significantly improve your liver health and quality of life. This involves a commitment to lifestyle changes, close collaboration with your healthcare team, and consistent monitoring. Remember, proactive steps today can lead to a healthier tomorrow.
Don’t hesitate to reach out to your doctor for personalized guidance and support – taking control of your health is the most empowering step you can take.
FAQ Explained
What are the early symptoms of grade 3 fatty liver disease?
Many people with grade 3 fatty liver disease have no noticeable symptoms in the early stages. As the disease progresses, you might experience fatigue, abdominal pain, and jaundice (yellowing of the skin and eyes). It’s important to get regular checkups.
Is grade 3 fatty liver reversible?
While complete reversal isn’t always possible in advanced stages, significant improvement is achievable through lifestyle changes and medical intervention. The goal is to slow or halt disease progression.
What kind of specialist should I see?
A gastroenterologist or hepatologist (liver specialist) is best equipped to diagnose and manage grade 3 fatty liver disease.
Can I drink alcohol with grade 3 fatty liver disease?
No. Alcohol consumption should be strictly avoided as it can severely worsen the condition.
