Can Fatty Muscles Raise Heart Disease Risk? Expert Tells All
Can fatty muscles raise heart disease risk expert tells – Can fatty muscles raise heart disease risk? Expert tells all! That’s the burning question we’re tackling today. We often hear about belly fat and its link to heart problems, but what about the fat that accumulates
-within* our muscles? It turns out, intramuscular fat – the fat hidden inside our muscle tissue – might be a sneaky player in the heart disease game.
This post dives into the science, exploring how this often-overlooked fat contributes to cardiovascular risk and what we can do about it.
We’ll unpack the mechanisms linking intramuscular fat to conditions like inflammation, insulin resistance, and high blood pressure. We’ll also look at how to measure this type of fat, discuss lifestyle factors that influence its accumulation, and explore potential avenues for future research and clinical interventions. Get ready to learn something new about your heart health!
Defining “Fatty Muscles” and its Relationship to Heart Disease: Can Fatty Muscles Raise Heart Disease Risk Expert Tells
The term “fatty muscles,” or more accurately, intramuscular fat (IMF), refers to the accumulation of fat within the muscle tissue itself. While some IMF is normal and even potentially beneficial, excessive accumulation is linked to various metabolic disorders, including an increased risk of heart disease. Understanding the mechanisms behind this relationship is crucial for developing effective preventative strategies.Intramuscular fat accumulation is a complex process influenced by several factors.
Genetic predisposition plays a role, as some individuals are naturally more prone to storing fat within their muscles. Lifestyle choices, such as a diet high in saturated and trans fats and a sedentary lifestyle, significantly contribute to increased IMF. Insulin resistance, a hallmark of metabolic syndrome, also promotes fat storage in muscle tissue. Essentially, when the body’s cells become less responsive to insulin, excess glucose and fatty acids are less efficiently used for energy and instead are stored as fat, including within the muscles.
Types of Intramuscular Fat and Their Impact on Cardiovascular Health
Intramuscular fat isn’t a homogenous entity. Different types exist, and their impact on cardiovascular health varies. Subcutaneous fat, located beneath the skin, is generally considered less harmful than visceral fat, which surrounds organs like the heart and liver. Similarly, IMF can be categorized based on its location and cellular composition, impacting its metabolic effects. Research suggests that certain types of IMF are more closely associated with inflammation and insulin resistance, contributing to the development of atherosclerosis (hardening of the arteries), a major risk factor for heart disease.
The precise mechanisms through which specific IMF types contribute to cardiovascular risk are still being investigated, but the link is increasingly clear.
Comparison of Fatty Muscles with Other Heart Disease Risk Factors
Fatty muscles represent one piece of a complex puzzle in heart disease risk. It’s not an isolated factor but rather interacts with other established risk factors, such as high blood pressure, high cholesterol, diabetes, and smoking. While elevated IMF may not be as overtly impactful as severely elevated cholesterol, for example, it acts synergistically with other risk factors, amplifying the overall cardiovascular risk.
An individual with high IMF, high blood pressure, and diabetes faces a considerably higher risk than someone with only one of these factors. This highlights the importance of a holistic approach to cardiovascular health, addressing all contributing factors rather than focusing on just one.
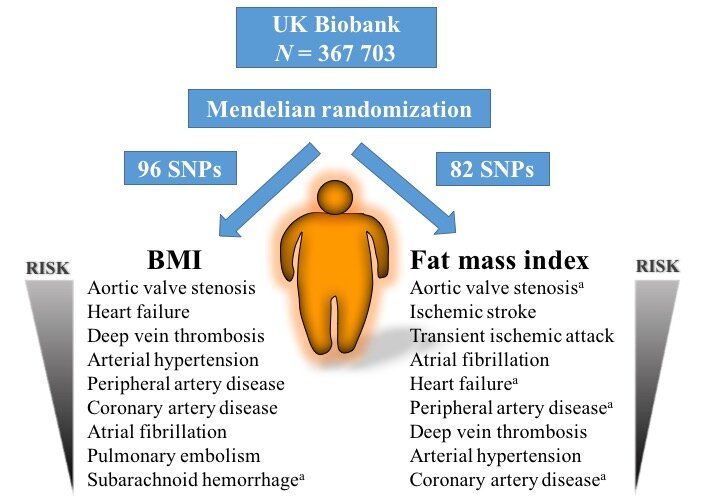
Studies Investigating the Link Between Fatty Muscles and Heart Disease Risk
Numerous studies have explored the relationship between IMF and cardiovascular disease. For example, studies using magnetic resonance imaging (MRI) have shown a positive correlation between increased IMF and markers of cardiovascular risk, such as increased levels of inflammatory cytokines and reduced insulin sensitivity. Other research has linked high IMF to an increased incidence of coronary artery disease and heart failure.
While more research is needed to fully elucidate the causal pathways, the accumulating evidence consistently points towards a significant association between excessive intramuscular fat and heightened heart disease risk. These studies underscore the importance of considering IMF as a potentially modifiable risk factor for cardiovascular disease.
Mechanisms Linking Fatty Muscles to Increased Heart Disease Risk
The presence of excess intramuscular fat, often termed “fatty muscles,” isn’t simply an aesthetic concern; it’s increasingly recognized as a significant contributor to cardiovascular disease risk. This isn’t a direct causal relationship, but rather a complex interplay of several metabolic and physiological processes. Understanding these mechanisms is crucial for developing effective preventative strategies.
Intramuscular fat accumulation disrupts the delicate balance within muscle tissue, triggering a cascade of events that negatively impact cardiovascular health. This disruption involves inflammation, insulin resistance, altered lipid profiles, and impaired vascular function, all of which significantly elevate the risk of heart disease.
The Role of Inflammation in Fatty Muscles and Cardiovascular Disease
Intramuscular fat accumulation leads to chronic low-grade inflammation within the muscle. This inflammation isn’t just localized; it spills over into the systemic circulation, contributing to a pro-inflammatory state throughout the body. Adipocytes (fat cells) within the muscle release inflammatory cytokines, such as TNF-α and IL-6. These cytokines promote endothelial dysfunction, a critical early step in the development of atherosclerosis (hardening of the arteries).
The persistent inflammation damages blood vessel walls, making them more susceptible to plaque formation and ultimately increasing the risk of heart attack and stroke. Studies have shown a positive correlation between intramuscular fat content and elevated levels of circulating inflammatory markers in individuals with cardiovascular disease.
The Contribution of Fatty Muscles to Insulin Resistance and Metabolic Syndrome
Fatty muscles often accompany insulin resistance, a condition where the body’s cells don’t respond effectively to insulin, leading to elevated blood sugar levels. The excess fat within muscle tissue interferes with insulin signaling pathways, reducing the muscle’s ability to take up glucose from the bloodstream. This impaired glucose uptake contributes to hyperglycemia (high blood sugar), a key feature of metabolic syndrome.
Metabolic syndrome is a cluster of conditions – including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels – that increase the risk of heart disease, stroke, and type 2 diabetes. The link between intramuscular fat, insulin resistance, and metabolic syndrome highlights the multifaceted nature of this risk factor.
The Impact of Intramuscular Fat on Blood Lipid Profiles
Intramuscular fat can negatively influence blood lipid profiles, further increasing cardiovascular risk. Studies suggest that higher intramuscular fat content is associated with elevated levels of triglycerides (a type of fat found in the blood) and decreased levels of high-density lipoprotein (HDL) cholesterol (“good” cholesterol). These alterations in lipid profiles contribute to the development of atherosclerosis, as increased triglycerides and decreased HDL cholesterol promote plaque formation within the arteries.
For example, a study might find that individuals with high intramuscular fat have triglyceride levels averaging 200 mg/dL, compared to 150 mg/dL in individuals with lower intramuscular fat, representing a significant increase in cardiovascular risk.
The Effects of Fatty Muscles on Blood Pressure and Vascular Function
The presence of excess intramuscular fat can directly impact blood pressure and vascular function, contributing to cardiovascular disease. The chronic low-grade inflammation associated with fatty muscles damages the endothelium (the inner lining of blood vessels), impairing its ability to regulate blood flow and blood pressure. This endothelial dysfunction leads to vasoconstriction (narrowing of blood vessels), increasing blood pressure.
Additionally, the stiffness of the arteries can increase due to the inflammatory process, further contributing to elevated blood pressure and increased risk of cardiovascular events. Research suggests a strong correlation between intramuscular fat and increased arterial stiffness, indicating a direct pathway by which fatty muscles can negatively impact cardiovascular health.
Assessing and Measuring Intramuscular Fat
Source: b-cdn.net
Measuring intramuscular fat (IMF) isn’t a simple task. Several techniques exist, each with its own strengths and weaknesses, impacting the accuracy and feasibility of assessing IMF levels in individuals. The choice of method often depends on factors like cost, availability, and the level of detail required. Understanding these methods is crucial for researchers and clinicians working to understand the link between IMF and heart disease risk.
Several methods are currently employed to quantify intramuscular fat. These range from non-invasive imaging techniques to more invasive procedures like muscle biopsies. Each method offers a different balance of precision, invasiveness, and cost-effectiveness.
Intramuscular Fat Measurement Techniques
The following techniques are commonly used to assess intramuscular fat content. Understanding their advantages and disadvantages is essential for selecting the most appropriate method for a given research question or clinical scenario.
- Magnetic Resonance Imaging (MRI): MRI provides high-resolution images of muscle tissue, allowing for precise quantification of IMF. Different MRI sequences can be used to specifically target fat within the muscle. For example, Dixon imaging techniques can effectively separate fat and water signals, improving the accuracy of IMF measurement.
- Computed Tomography (CT) Scans: CT scans are another imaging modality that can be used to assess IMF. While not as precise as MRI for distinguishing fat from other tissues, CT scans are more widely available and generally less expensive. However, CT scans expose patients to ionizing radiation, limiting their use, especially in repeated assessments.
- Muscle Biopsies: Muscle biopsies involve the surgical removal of a small sample of muscle tissue. This tissue can then be analyzed in a laboratory to determine the percentage of fat by weight or volume. While this is considered the gold standard for IMF measurement, it’s an invasive procedure, limiting its applicability in large-scale studies.
Comparison of Intramuscular Fat Assessment Techniques
The table below summarizes the advantages and disadvantages of the three main methods for assessing intramuscular fat.
| Method | Advantages | Disadvantages | Cost |
|---|---|---|---|
| MRI | High precision, non-invasive, detailed anatomical information | Expensive, long scan times, may be contraindicated in some patients (e.g., those with metal implants) | High |
| CT Scan | Relatively inexpensive, widely available, faster scan times than MRI | Lower precision than MRI, exposes patients to ionizing radiation | Moderate |
| Muscle Biopsy | Gold standard for accuracy, allows for histological analysis | Invasive, risk of complications, limited sample size, not suitable for large-scale studies | Moderate to High |
Precision, Invasiveness, and Cost-Effectiveness of Measurement Techniques
The following points summarize the key characteristics of each technique, considering their precision, invasiveness, and cost-effectiveness. These factors are crucial in determining the suitability of a particular method for a given application.
- MRI: High precision, non-invasive, high cost.
- CT Scan: Moderate precision, minimally invasive (radiation exposure), moderate cost.
- Muscle Biopsy: Highest precision, invasive, moderate to high cost.
Lifestyle Factors and Fatty Muscles
Intramuscular fat, that fat nestled within our muscles, isn’t just a cosmetic concern; it’s increasingly linked to cardiovascular health. While genetics play a role, our lifestyle choices significantly influence the amount of intramuscular fat we accumulate. Understanding these lifestyle factors is crucial for mitigating heart disease risk.
Diet’s Impact on Intramuscular Fat Accumulation
The food we consume directly impacts intramuscular fat levels. A diet high in saturated and trans fats, readily found in processed foods, red meat, and some dairy products, promotes fat storage throughout the body, including within muscles. Conversely, a diet rich in fruits, vegetables, whole grains, and lean proteins supports healthy muscle composition and minimizes intramuscular fat accumulation.
For example, studies have shown a correlation between a high intake of processed foods and increased levels of intramuscular fat in obese individuals, while diets emphasizing Mediterranean-style eating patterns have been associated with lower levels. This highlights the importance of focusing on nutrient-dense foods and limiting highly processed items.
Physical Activity’s Role in Preventing or Reducing Intramuscular Fat
Regular physical activity is a powerful tool in combating intramuscular fat accumulation. Aerobic exercise, such as running, swimming, or cycling, helps burn calories and improves overall metabolic health, thereby reducing fat storage. Resistance training, involving weightlifting or bodyweight exercises, increases muscle mass and improves muscle quality, potentially displacing intramuscular fat. Studies have demonstrated that individuals who engage in regular, moderate-intensity exercise tend to have lower levels of intramuscular fat compared to their sedentary counterparts.
So, experts are saying fatty muscles might up your heart disease risk – a pretty scary thought! It makes you wonder about organ health in general, and the amazing news that the FDA just approved clinical trials for pig kidney transplants in humans – check out this article for the details: fda approves clinical trials for pig kidney transplants in humans.
This breakthrough highlights how crucial organ health is, reminding us to focus on our overall well-being, including managing muscle health to reduce heart disease risks.
For instance, a study involving middle-aged adults showed a significant reduction in intramuscular fat after six months of combined aerobic and resistance training.
Influence of Sleep Quality and Stress on Intramuscular Fat Levels
Sleep deprivation and chronic stress disrupt hormonal balance, impacting metabolic processes and potentially leading to increased intramuscular fat. Insufficient sleep is associated with elevated levels of cortisol, a stress hormone that can promote fat storage. Chronic stress also contributes to increased cortisol levels and can negatively affect insulin sensitivity, further facilitating intramuscular fat accumulation. Research indicates a correlation between poor sleep quality and higher intramuscular fat levels, especially in individuals with existing metabolic disorders.
Similarly, studies have linked chronic stress to increased visceral and intramuscular fat accumulation. Prioritizing adequate sleep and implementing stress-management techniques, such as mindfulness or yoga, are crucial for maintaining healthy intramuscular fat levels.
Hypothetical Infographic: Lifestyle Factors and Intramuscular Fat
Imagine an infographic with a central image depicting a healthy muscle fiber contrasted with an unhealthy one laden with intramuscular fat. Arrows emanating from the healthy muscle point towards icons representing healthy lifestyle choices: a balanced plate of fruits, vegetables, and lean protein; a person exercising; a peaceful sleeping figure; and a relaxed individual practicing yoga. Conversely, arrows pointing towards the unhealthy muscle show icons representing unhealthy lifestyle choices: processed foods, a sedentary individual, a person experiencing stress, and a person with poor sleep.
The infographic would clearly illustrate the positive correlation between healthy lifestyle choices and reduced intramuscular fat, and the negative correlation between unhealthy choices and increased intramuscular fat. Data points, such as percentage changes in intramuscular fat based on different lifestyle choices, could further strengthen the visual representation.
Clinical Implications and Future Research
Understanding the link between intramuscular fat (IMF) and heart disease risk has significant clinical implications, demanding further research to refine diagnostic tools, treatment strategies, and preventative measures. Current research highlights a correlation, but the causal relationship and the precise mechanisms involved require more investigation. This necessitates well-designed clinical studies and a multi-faceted approach to address this emerging health concern.A crucial next step is translating research findings into practical applications for patient care.
This includes developing effective strategies for assessing IMF levels, implementing targeted interventions, and improving risk stratification for cardiovascular disease.
So, experts are saying fatty muscles might up your heart disease risk – scary stuff, right? Understanding how to fuel our bodies properly is key, and that’s where nutrition comes in. To really optimize heart health, checking out this article on are women and men receptive of different types of food and game changing superfoods for women might be helpful.
Knowing what foods best support our individual needs is crucial in managing heart health risks linked to things like fatty muscle build-up.
A Hypothetical Clinical Study Design
A prospective cohort study could effectively investigate the relationship between IMF and heart disease. This study would recruit a large and diverse group of participants, measuring their IMF levels using advanced imaging techniques such as MRI or CT scans. Participants would be followed for a defined period (e.g., 10 years), with regular assessments of cardiovascular health markers, including blood pressure, cholesterol levels, and incidence of cardiovascular events (heart attacks, strokes, etc.).
The study would adjust for confounding factors like age, sex, BMI, physical activity levels, and dietary habits to isolate the effect of IMF on cardiovascular outcomes. Statistical analysis would then determine the strength of the association between IMF levels and the risk of developing heart disease. A control group with low IMF levels would provide a crucial benchmark for comparison.
Informing Clinical Practice and Patient Management
Findings from such a study could significantly alter clinical practice. For example, if a strong association is confirmed, IMF measurement could become a routine part of cardiovascular risk assessments, alongside traditional risk factors. This could lead to earlier interventions, including lifestyle modifications (diet, exercise) or pharmacological treatments to reduce IMF and mitigate cardiovascular risk. Patients with elevated IMF levels might be offered personalized interventions, including targeted exercise programs and nutritional counseling, to address their specific needs and improve their cardiovascular health.
The integration of IMF assessment into clinical practice would allow for a more comprehensive and personalized approach to cardiovascular risk management.
Knowledge Gaps and Areas for Future Research, Can fatty muscles raise heart disease risk expert tells
Despite growing evidence, significant knowledge gaps remain. Further research is needed to understand the specific mechanisms by which IMF contributes to heart disease. For instance, the role of inflammation, insulin resistance, and ectopic lipid deposition within the heart muscle warrants further investigation. Additionally, the optimal methods for measuring IMF and the long-term effects of interventions aimed at reducing IMF need to be established.
So, experts are saying fatty muscles might up your heart disease risk – scary stuff, right? It makes you think about long-term health choices, and how we need to be proactive. It’s a bit like the decisions Karishma Mehta made when she chose to freeze her eggs, as detailed in this article karishma mehta gets her eggs frozen know risks associated with egg freezing , highlighting the importance of understanding the risks involved in those kinds of choices.
Ultimately, managing health risks, whether from fatty muscles or fertility decisions, requires careful consideration and planning.
Studies focusing on specific populations (e.g., individuals with metabolic syndrome or family history of heart disease) are also crucial to refine risk prediction models and tailor interventions. Finally, cost-effective and widely accessible methods for IMF assessment are needed to facilitate large-scale population screening and preventative strategies.
Recommendations for Public Health Interventions
Public health initiatives should focus on promoting lifestyle changes that reduce IMF accumulation. This includes promoting a healthy diet rich in fruits, vegetables, and whole grains, while limiting processed foods, saturated fats, and added sugars. Regular physical activity, including both aerobic and strength training exercises, is essential. Public health campaigns can educate the public about the importance of maintaining a healthy weight and the link between IMF and cardiovascular health.
National health guidelines could incorporate recommendations for IMF assessment and management as part of routine cardiovascular health checks. Furthermore, community-based programs can provide support and resources for individuals seeking to adopt healthier lifestyles and reduce their risk of heart disease through IMF reduction. The long-term success of these interventions will depend on sustained commitment and collaborative efforts from healthcare professionals, policymakers, and the public.
Epilogue
Source: eatthis.com
So, can fatty muscles raise your heart disease risk? The answer, according to experts, is a resounding “yes, potentially.” While more research is needed, the evidence suggests a strong correlation. Understanding the role of intramuscular fat is crucial for a comprehensive approach to heart health. By focusing on a healthy diet, regular exercise, stress management, and adequate sleep, we can actively work towards minimizing intramuscular fat accumulation and safeguarding our cardiovascular well-being.
Let’s make informed choices today for a healthier tomorrow!
Commonly Asked Questions
What are the symptoms of high intramuscular fat?
There aren’t specific symptoms for high intramuscular fat itself. Often, it’s discovered through imaging tests done for other reasons. However, if you have other risk factors for heart disease (like high blood pressure, high cholesterol, or family history), it’s important to get checked.
Can losing weight reduce intramuscular fat?
Yes, weight loss, especially through a combination of diet and exercise, can help reduce intramuscular fat. Focus on a balanced diet and regular physical activity for optimal results.
Is there a specific diet to reduce intramuscular fat?
While there isn’t one magic diet, a diet rich in fruits, vegetables, whole grains, and lean protein, while limiting processed foods, saturated fats, and added sugars, is beneficial. Consult a nutritionist for personalized guidance.
