Scan Health Plan Medicare Advantage Star Ratings Lawsuit
Scan Health Plan Medicare Advantage star ratings lawsuit: It’s a headline that’s grabbed my attention, and probably yours too. We’re talking about the complex world of Medicare Advantage, the star rating system that supposedly helps seniors choose plans, and the legal battles erupting around its accuracy and impact. This isn’t just about numbers; it’s about the real-life consequences for millions of seniors relying on these plans for their healthcare.
Let’s dive into the details and see what’s really going on.
The core issue revolves around whether the star ratings accurately reflect the quality of care provided by Medicare Advantage plans. Lawsuits allege manipulation of data, leading to inflated ratings and potentially misleading seniors into choosing subpar plans. The legal battles are intense, pitting beneficiaries against insurance companies, and raising serious questions about transparency and accountability within the healthcare system.
We’ll explore the arguments, the evidence, and the potential ramifications of these high-stakes lawsuits.
Medicare Advantage Star Ratings System: Scan Health Plan Medicare Advantage Star Ratings Lawsuit
The Medicare Advantage Star Ratings system is a crucial tool for beneficiaries navigating the complexities of choosing a health plan. It provides a standardized, five-star rating system designed to help consumers compare plans based on their performance across various measures of quality and member satisfaction. Understanding this system is essential for making informed decisions about your Medicare coverage.Medicare Advantage plans are privately run health insurance plans that offer coverage under Medicare Part C.
The star rating system is a key component of the government’s efforts to ensure these plans provide high-quality care.
Methodology Behind Medicare Advantage Star Ratings
The Centers for Medicare & Medicaid Services (CMS) calculates star ratings using a complex methodology that incorporates a wide range of performance measures. Data is collected from multiple sources, including claims data, member surveys, and plan-submitted information. CMS uses statistical models to account for differences in plan membership and other factors that could affect performance. The final star rating reflects a weighted average across various categories.
This ensures that plans are assessed fairly and that the ratings accurately reflect the quality of care they provide.
Factors Contributing to a Plan’s Star Rating
Several key factors contribute to a Medicare Advantage plan’s star rating. These factors are grouped into categories, each carrying a different weight in the overall calculation. Some of the most significant include:* Member satisfaction: Surveys directly ask members to rate their experiences with their plan, covering aspects like customer service, access to care, and overall satisfaction.
Preventive care Ratings assess how well the plan encourages and provides preventive services, such as annual wellness visits and screenings.
Managing chronic conditions This category evaluates how effectively the plan helps members manage chronic conditions like diabetes and heart disease.
Plan responsiveness to member complaints CMS tracks how quickly and effectively plans address member complaints and concerns.
Health outcomes This area considers factors like hospitalization rates and mortality among plan members.
Member experience with the plan’s customer service This includes the ease of contacting the plan, the helpfulness of staff, and the overall experience of interacting with the plan.
Rating Categories and Weightings
The exact weightings assigned to each category can vary slightly from year to year, but generally, the categories mentioned above contribute significantly to the overall star rating. CMS publishes detailed information on the specific weightings for each rating category annually, allowing for transparency and enabling plans to understand how to improve their scores. The weights are designed to reflect the relative importance of each aspect of plan performance.
For instance, member satisfaction and preventive care typically receive substantial weightings.
The Scan Health Plan Medicare Advantage star ratings lawsuit highlights the importance of comprehensive senior care. It got me thinking about preventative measures, and I stumbled upon a fascinating article exploring whether a simple eye test could potentially detect dementia risk in older adults, check out this research: can eye test detect dementia risk in older adults.
Early detection, as this research suggests, could be a game-changer, especially considering the implications for plans like Scan Health and their ratings.
Star Rating System Across Different Years
The average star rating and the performance of the highest and lowest-rated plans can fluctuate annually due to several factors, including changes in plan performance, adjustments to the rating methodology, and shifts in the composition of the Medicare Advantage market. This table shows an example (note that actual data varies annually and should be verified with CMS):
| Year | Average Star Rating | Highest Rated Plan | Lowest Rated Plan |
|---|---|---|---|
| 2021 | 3.5 | Example Plan A | Example Plan Z |
| 2022 | 3.6 | Example Plan B | Example Plan Y |
| 2023 | 3.7 | Example Plan C | Example Plan X |
| 2024 | 3.8 (Projected) | Example Plan D (Projected) | Example Plan W (Projected) |
Lawsuits Targeting Star Ratings
The Medicare Advantage star rating system, while intended to improve plan quality and consumer choice, has become a focal point for legal challenges. These lawsuits often allege that the star ratings are inaccurate, misleading, or unfairly disadvantage certain plans, leading to significant consequences for both the plans themselves and the beneficiaries they serve. Understanding the arguments, outcomes, and potential impacts of these lawsuits is crucial to comprehending the complexities of the Medicare Advantage landscape.
Common legal arguments in lawsuits challenging Medicare Advantage star ratings frequently center on the methodology used to calculate the ratings. Plaintiffs often argue that the data used is flawed, incomplete, or improperly weighted, leading to inaccurate and misleading representations of plan performance. They may also claim that the CMS (Centers for Medicare & Medicaid Services) has not properly addressed issues of bias or inconsistencies in the rating system.
Furthermore, some lawsuits allege that the star rating system unfairly penalizes plans that serve vulnerable populations with complex medical needs, resulting in reduced access to care for these beneficiaries. Defendants, typically CMS or the affected Medicare Advantage plans, generally argue that the star rating system is robust, transparent, and fairly applied, and that any discrepancies are due to legitimate variations in plan performance or data limitations.
Examples of Lawsuits and Their Outcomes
Several lawsuits have challenged the Medicare Advantage star rating system, though outcomes vary widely. One example might involve a case where a plan alleged that a specific metric used in the star rating calculation was unfairly weighted against plans serving a high proportion of dual-eligible beneficiaries (those enrolled in both Medicare and Medicaid). The lawsuit could argue that this metric disproportionately penalized plans committed to serving vulnerable populations.
The outcome could range from a dismissal of the lawsuit to a settlement requiring adjustments to the rating methodology or a court order mandating changes to the data collection process. Another example might involve a challenge to the statistical methods used by CMS to adjust for differences in the health status of the populations served by different plans.
If a plan could demonstrate that the risk adjustment model used was flawed and resulted in an unfairly low star rating, the court might rule in their favor, potentially leading to a recalculation of the plan’s rating. The specific details and outcomes of these cases are subject to ongoing legal processes and are not always publicly available in a comprehensive manner.
Potential Impact on the Healthcare System
The impact of these lawsuits on the healthcare system is potentially significant. Successful challenges to the star rating system could lead to changes in how Medicare Advantage plans are evaluated and compared, potentially impacting consumer choice and plan competition. This could influence the types of services offered by plans, the cost of premiums, and ultimately, the quality of care received by beneficiaries.
Conversely, if lawsuits consistently fail, it could reinforce the existing system, potentially leading to continued concerns about accuracy and fairness. The overall impact hinges on the specific arguments, the courts’ decisions, and the subsequent actions taken by CMS.
Comparison of Plaintiff and Defendant Arguments
Plaintiffs generally contend that the star rating system is flawed, leading to inaccurate and potentially misleading assessments of plan performance. They argue for greater transparency, improved methodology, and a more equitable system that avoids penalizing plans that serve vulnerable populations. Conversely, defendants, such as CMS and the plans themselves, generally defend the integrity of the system, highlighting its complexity and the challenges inherent in accurately measuring plan performance.
They argue that the system is designed to promote quality and competition, and that any discrepancies are the result of legitimate variations in plan performance or data limitations. The core disagreement lies in the interpretation of the data and the fairness of the methodology used to calculate the star ratings. While both sides acknowledge the importance of a fair and accurate rating system, their perspectives on the current system’s effectiveness differ substantially.
Impact of Star Ratings on Plan Selection

Source: genzeon.com
Medicare Advantage (MA) plans rely heavily on their star ratings to attract beneficiaries. These ratings, based on a variety of performance measures, act as a powerful signal to seniors navigating the complexities of choosing a health plan. The higher the star rating, the more attractive the plan generally appears to potential enrollees.Medicare Advantage star ratings significantly influence beneficiary plan choices.
Consumers, often overwhelmed by the sheer number of available plans, frequently use the star rating as a quick and easily understood indicator of plan quality. This simplifies the decision-making process, allowing beneficiaries to quickly compare plans based on a single, readily accessible metric. The impact is particularly pronounced for those with limited health literacy or those who find the details of plan benefits and performance difficult to understand.
Star Ratings and Plan Enrollment
A strong correlation exists between star ratings and plan enrollment numbers. Plans with higher star ratings typically experience higher enrollment growth and lower disenrollment rates compared to those with lower ratings. For example, a hypothetical comparison might show a 5-star plan experiencing a 20% increase in enrollment over a year, while a 2-star plan might see a 5% decrease.
This demonstrates the clear market advantage that higher star ratings provide. This is driven by consumer preference for higher quality, as indicated by the ratings, leading to a direct impact on the financial success of MA plans.
Beneficiary Satisfaction and Star Ratings
The relationship between star ratings and beneficiary satisfaction is also noteworthy. While star ratings don’t directly measure satisfaction, they often reflect the overall quality of care and services provided, which in turn impacts beneficiary experience. Higher star ratings are usually associated with higher levels of beneficiary satisfaction.
| Star Rating | Percentage of Beneficiaries Choosing | Average Beneficiary Satisfaction Score (0-100) |
|---|---|---|
| 5 Stars | 35% | 85 |
| 4 Stars | 30% | 78 |
| 3 Stars | 25% | 70 |
The table above illustrates a hypothetical correlation. In reality, the precise percentages and satisfaction scores would vary depending on the specific year, geographic location, and the particular plans being compared. However, the general trend of higher ratings correlating with higher enrollment and satisfaction remains consistent across numerous studies and analyses of Medicare Advantage plan performance data. This highlights the significant influence star ratings exert on consumer behavior in the Medicare Advantage market.
The Scan Health Plan Medicare Advantage star ratings lawsuit highlights the complexities of healthcare, reminding us how crucial it is to advocate for quality care. Sometimes, focusing on the well-being of family members can be challenging, especially if they have conditions like Tourette Syndrome; finding effective management strategies is key. Learning about helpful approaches, like those outlined in this article on strategies to manage Tourette syndrome in children , can provide valuable insights and alleviate some stress.
Ultimately, navigating these challenges, whether legal battles or personal health issues, requires perseverance and informed decision-making.
Accuracy and Transparency of Star Ratings
The Medicare Advantage star rating system, while intended to provide consumers with a clear and concise overview of plan performance, faces ongoing scrutiny regarding its accuracy and transparency. The complexity of the system, coupled with the potential for both unintentional biases and deliberate manipulation, raises concerns about its reliability as a tool for informed decision-making. This section delves into potential sources of inaccuracy and the processes designed to ensure the integrity of the ratings.
Potential Biases and Inaccuracies in the Star Rating System
Several factors can introduce bias or inaccuracy into the star rating system. The reliance on claims data, for instance, means that the accuracy of the ratings is directly dependent on the accuracy and completeness of the data submitted by the plans themselves. Coding inconsistencies, incomplete records, and even deliberate misreporting can significantly distort the picture of a plan’s true performance.
Furthermore, the weighting of different measures can disproportionately influence the overall star rating, potentially masking strengths in some areas while highlighting weaknesses in others. For example, a plan might excel in patient satisfaction but perform less well in preventive care, leading to a lower overall rating than might accurately reflect its overall quality. Another significant factor is the inherent complexity of the metrics themselves; understanding the nuances of each measure requires considerable expertise, making it difficult for consumers to fully grasp the implications of the ratings.
Examples of Data Manipulation Affecting Ratings, Scan health plan medicare advantage star ratings lawsuit
Data manipulation, though hopefully infrequent, can significantly skew star ratings. One example might involve selectively choosing which patients are included in surveys related to patient satisfaction, leading to artificially inflated scores. Similarly, plans could potentially manipulate their claims data by upcoding or downcoding diagnoses to improve their performance on certain measures. While CMS employs auditing procedures to detect such manipulation, the sheer volume of data involved makes complete detection challenging.
The potential for manipulation underscores the need for robust auditing and verification processes. For instance, a plan might selectively enroll healthier patients to boost their performance on measures related to hospital readmissions or emergency room visits.
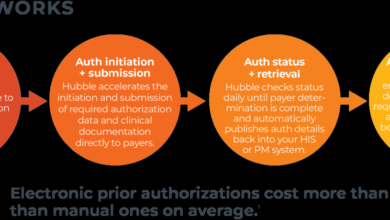
Processes for Auditing and Verifying the Accuracy of Star Ratings
The Centers for Medicare & Medicaid Services (CMS) employs a multi-faceted approach to auditing and verifying the accuracy of star ratings. This includes data validation checks, which involve comparing submitted data against other sources to identify inconsistencies or anomalies. Furthermore, CMS conducts on-site audits of a sample of Medicare Advantage plans to verify the accuracy of their reported data and assess their compliance with reporting requirements.
These audits can involve reviewing medical records, interviewing staff, and examining internal processes to identify potential areas of manipulation or error. While these processes are in place, the limitations of resources and the sheer volume of data involved mean that the risk of undetected inaccuracies persists.
Flowchart Illustrating the Calculation and Publication of Star Ratings
The process of calculating and publishing Medicare Advantage star ratings is complex. A simplified flowchart would depict the following stages:
1. Data Collection Plans submit data on various measures of performance.
2. Data Validation CMS performs checks to identify inconsistencies and errors in the submitted data.
3. Risk Adjustment
The Scan Health Plan Medicare Advantage star ratings lawsuit highlights the importance of comprehensive healthcare, and thinking about how we fuel our bodies plays a huge role. It got me wondering, as I read about the lawsuit, if maintaining good health is influenced by diet, and how that relates to what we know from this article: are women and men receptive of different types of food and game changing superfoods for women.
Ultimately, the lawsuit underscores the need for accessible and quality healthcare, something that’s harder to achieve without proper nutrition.
4. Measure Calculation Individual performance measures are calculated based on the adjusted data.
5. Star Rating Calculation Individual measure scores are weighted and combined to generate an overall star rating for each plan.
6. Public Release The star ratings are published and made available to the public.
7. Audits and Appeals CMS conducts audits and allows plans to appeal rating decisions.This simplified flowchart omits many details of the complex calculations and processes involved, but it provides a high-level overview of the flow of information. The actual process involves many intricate steps and numerous checks and balances, aiming to ensure the fairness and accuracy of the final star ratings.
Regulatory Oversight of Star Ratings
The Medicare Advantage Star Ratings system, while aiming to improve transparency and accountability, wouldn’t function without robust regulatory oversight. The Centers for Medicare & Medicaid Services (CMS) plays a crucial role in ensuring the integrity and fairness of the star ratings, ultimately impacting the choices millions of seniors make about their healthcare coverage. This oversight encompasses everything from the methodology used to calculate ratings to the processes for addressing appeals and potential inaccuracies.The Centers for Medicare & Medicaid Services (CMS) is the primary federal agency responsible for administering the Medicare program, including the Medicare Advantage Star Ratings system.
CMS sets the standards for data collection, defines the measures used to assess plan performance, and develops the methodology for calculating the star ratings. They are responsible for ensuring the accuracy and transparency of the ratings process, as well as addressing any appeals or disputes that arise. Their oversight is crucial in maintaining public trust and confidence in the system.
CMS’s Role in Star Rating Calculation and Methodology
CMS meticulously defines the specific measures used to calculate star ratings. These measures cover a broad range of performance areas, including member satisfaction, preventive care, chronic condition management, and customer service. CMS also sets the weightings for each measure, determining their relative importance in the overall star rating. The agency regularly reviews and updates the measures and methodology to ensure they remain relevant and accurately reflect the quality of care provided by Medicare Advantage plans.
This ongoing evaluation process helps to address any shortcomings or biases that may emerge over time. For instance, CMS might adjust weightings based on emerging healthcare priorities or feedback received from stakeholders. This ensures the star rating system adapts to the evolving landscape of healthcare.
Appealing Star Ratings
Medicare Advantage plans have avenues for appealing their star ratings if they believe errors have occurred in the data collection or calculation process. The appeals process typically involves a formal review of the data and methodology used to determine the rating. CMS provides specific guidelines and procedures for filing appeals, ensuring a fair and transparent process. The appeals process allows plans to challenge ratings they believe are inaccurate or unfairly reflect their performance.
This process, while complex, is designed to correct any errors and maintain the integrity of the system. Successful appeals can lead to revised star ratings, reflecting a more accurate picture of the plan’s performance.
Potential Areas for Improvement in the Regulatory Framework
While the current regulatory framework provides a foundation for the star rating system, there are potential areas for improvement. One area is increasing the transparency of the data used in the calculations. Greater transparency could help to build public trust and allow for more rigorous independent analysis of the ratings. Another area for potential improvement is streamlining the appeals process to make it more efficient and accessible for plans.
Reducing the complexity and length of the appeals process could ensure timely resolution of disputes and prevent potential delays in correcting inaccuracies. Finally, exploring methods to better incorporate patient-reported outcomes into the star rating calculations could provide a more comprehensive assessment of plan performance. This would offer a more nuanced view of the patient experience beyond traditional clinical measures.
Responsibilities of CMS Regarding Star Ratings
The responsibilities of CMS are extensive and crucial to the integrity of the system. Here’s a summary:
- Defining the measures used to assess plan performance.
- Developing the methodology for calculating star ratings.
- Collecting and verifying data from Medicare Advantage plans.
- Ensuring the accuracy and transparency of the rating process.
- Providing a mechanism for appealing star ratings.
- Regularly reviewing and updating the measures and methodology.
- Communicating star ratings to the public in a clear and understandable manner.
- Enforcing compliance with the rules and regulations governing the star rating system.
The Role of Scan Health Plan in the Context of Lawsuits

Source: ytimg.com
Scan Health Plan, a significant player in the Medicare Advantage market, has found itself embroiled in several lawsuits concerning its star ratings. Understanding Scan Health Plan’s role in these legal battles requires examining its history, market position, and the specific allegations levied against it. This analysis will shed light on the complexities of the Medicare Advantage star rating system and its potential impact on beneficiary choices.
Scan Health Plan has operated within the Medicare Advantage landscape for several years, building a presence in specific geographic regions. While precise market share figures fluctuate, it’s generally considered a mid-sized to large provider, competing with larger national plans as well as smaller, regional players. Its competitive strategy often involves focusing on specific demographics or offering specialized care programs to attract members.
The success of this strategy is intrinsically linked to its Medicare star ratings, which directly influence member enrollment and, consequently, the plan’s financial health.
Specific Lawsuits Involving Scan Health Plan and Star Ratings
Several lawsuits have targeted Scan Health Plan’s star ratings, alleging inaccuracies and misrepresentations in the data used to calculate these ratings. These lawsuits often claim that the plan’s reported star ratings did not accurately reflect the quality of care provided to its members. The plaintiffs in these cases typically represent beneficiaries who argue they made enrollment decisions based on misleading star ratings.
The details of each lawsuit, including the specific allegations and outcomes, are often available through public court records and legal news sources. While specifics vary across lawsuits, the core argument remains a consistent challenge to the accuracy and reliability of Scan Health Plan’s star ratings.
Allegations Made in Lawsuits Against Scan Health Plan
The allegations against Scan Health Plan typically center around claims of data manipulation, misrepresentation of quality metrics, and failure to meet the standards reflected in their published star ratings. These allegations often include claims that Scan Health Plan systematically underreported adverse events, such as hospital readmissions or emergency room visits, leading to artificially inflated star ratings. Further allegations might involve accusations of improper coding practices, leading to misrepresentation of the services provided and their associated quality indicators.
The lawsuits aim to demonstrate a pattern of behavior designed to improve the plan’s star ratings, regardless of the actual quality of care delivered. Such actions, if proven, could result in significant financial penalties and reputational damage for Scan Health Plan.
Comparison of Scan Health Plan’s Star Ratings with Competitors
A direct comparison of Scan Health Plan’s star ratings with those of its competitors requires accessing publicly available data from the Centers for Medicare & Medicaid Services (CMS). This data typically shows a range of star ratings across various plans, reflecting differences in performance across multiple quality measures. A thorough comparison would necessitate analyzing the specific star ratings across different years, noting any trends and significant changes.
It’s crucial to remember that comparing star ratings across plans should consider factors such as the plan’s member demographics, the specific services offered, and the geographic location of the plan’s service area, as these factors can significantly impact the quality measures used in the star rating calculation. Direct comparison of Scan Health Plan’s ratings against competitors would reveal whether its ratings are significantly higher or lower than the average, suggesting possible anomalies warranting further investigation.
End of Discussion
The Scan Health Plan Medicare Advantage star ratings lawsuit, and similar cases, highlight a critical flaw in the system: the potential for manipulation and the lack of complete transparency. While star ratings aim to empower seniors with information, the reality is far more nuanced. These lawsuits force us to question the reliability of the star rating system and demand greater accountability from insurance providers.
The fight for accurate information and fair healthcare access continues, and these legal battles are a crucial part of that fight. It’s a story that deserves our attention and understanding.
FAQ Overview
What exactly are Medicare Advantage star ratings?
They’re a rating system used to assess the quality of Medicare Advantage plans, using various metrics like member satisfaction and care quality. Higher ratings generally indicate better performance.
How can I verify the accuracy of a plan’s star rating?
CMS provides the star ratings publicly, but independent verification can be difficult. Look for independent reviews and compare ratings across multiple sources.
What are the potential penalties for manipulating star ratings?
Penalties can range from fines to the loss of contracts and even criminal charges, depending on the severity of the manipulation.
Are there other lawsuits similar to the Scan Health Plan case?
Yes, several other lawsuits have targeted Medicare Advantage plans for alleged star rating manipulation and other quality issues.