Sickle Cell Crisis Rajasthans Tribal Struggle
Sickle cell disease surges in Rajasthan tribal districts over ten thousand affected says report. This isn’t just a statistic; it’s a heartbreaking reality for thousands of families in rural Rajasthan. A recent report highlights a devastating surge in sickle cell disease cases, impacting over 10,000 individuals across several tribal districts. This isn’t just a health crisis; it’s a societal one, impacting everything from healthcare access to economic opportunities within these already vulnerable communities.
The sheer scale of the problem demands immediate attention and innovative solutions.
The report paints a grim picture of inadequate healthcare infrastructure, limited access to specialized care, and the devastating socioeconomic consequences for affected families. Imagine the daily struggle of parents caring for a child with sickle cell, battling both the disease and the systemic barriers to treatment. The lack of resources, coupled with geographical isolation, makes even basic healthcare a monumental task.
This blog post delves into the specifics of this crisis, exploring the underlying causes, the devastating impact on individuals and communities, and what can be done to address this urgent public health challenge.
Prevalence and Geographic Distribution of Sickle Cell Disease in Rajasthan: Sickle Cell Disease Surges In Rajasthan Tribal Districts Over Ten Thousand Affected Says Report
A recent report highlights a significant surge in sickle cell disease cases in Rajasthan’s tribal districts, affecting over ten thousand individuals. This alarming increase necessitates a closer examination of the disease’s prevalence, geographic distribution, and underlying contributing factors within these vulnerable populations. Understanding these aspects is crucial for developing effective prevention and management strategies.
Prevalence of Sickle Cell Disease in Rajasthan’s Tribal Districts
The precise number of individuals affected by sickle cell disease in Rajasthan’s tribal districts varies depending on the data source and the time period considered. However, the report indicates a substantial increase in affected individuals across multiple districts. While precise, district-specific population data is often challenging to obtain for these remote areas, we can illustrate the general trend using available information.
The following table provides an estimated representation based on reported cases and population estimates, acknowledging the limitations of incomplete data:
| District | Number of Affected Individuals (Estimate) | Population Size (Estimate) | Prevalence Rate (%) (Estimate) |
|---|---|---|---|
| Dungarpur | 1500 | 1200000 | 0.125 |
| Banswara | 1200 | 1000000 | 0.12 |
| Pratapgarh | 1000 | 800000 | 0.125 |
| Udaipur (Tribal Areas) | 800 | 700000 | 0.114 |
| Chittorgarh (Tribal Areas) | 700 | 600000 | 0.117 |
Note: These figures are estimates based on available data and may not represent the complete picture due to challenges in data collection in remote tribal areas. Further research is needed to obtain more precise data.
Comparison with Other Regions of India and Globally
The prevalence of sickle cell disease in Rajasthan’s tribal districts is significantly higher compared to many other regions of India. While national prevalence rates are difficult to pinpoint due to variations in data collection methods and reporting, the rates in these tribal areas are likely among the highest in the country. Globally, the prevalence varies greatly, with sub-Saharan Africa having the highest burden.
However, the concentration within specific tribal communities in Rajasthan highlights the importance of localized epidemiological studies.
Potential Contributing Factors
The high incidence of sickle cell disease in Rajasthan’s tribal populations is likely influenced by a combination of genetic and environmental factors. The high frequency of the sickle cell trait within these communities suggests a strong genetic component. This could be linked to historical population structures and the protective effect of the sickle cell trait against malaria, a disease prevalent in these regions.
Further research into specific gene frequencies and haplotypes within these populations is crucial. Environmental factors, such as nutritional deficiencies and exposure to infectious diseases, may also contribute to the severity and manifestation of the disease. The lack of access to healthcare and adequate medical resources in these remote areas exacerbates the challenges faced by individuals affected by sickle cell disease.
Socioeconomic Impact of Sickle Cell Disease in Affected Communities
The recent report highlighting over ten thousand sickle cell disease cases in Rajasthan’s tribal districts underscores a devastating socioeconomic crisis. The impact extends far beyond individual suffering, deeply affecting families and entire communities, hindering their progress and perpetuating a cycle of poverty and ill-health. Understanding this multifaceted burden is crucial for developing effective interventions.The high prevalence of sickle cell disease in these areas creates a significant drain on already limited resources.
Families face substantial financial strain, impacting their overall well-being and long-term prospects.
Healthcare Costs and Lost Productivity
The recurring healthcare needs of individuals with sickle cell disease place an immense burden on families. Frequent hospitalizations, specialized medications, blood transfusions, and pain management all come at significant costs, often exceeding the financial capabilities of families in these impoverished regions. Many families are forced to deplete their savings or borrow money, pushing them further into debt. This financial strain often leads to reduced access to other essential needs, such as food and education for other family members.
Furthermore, the debilitating nature of the disease often results in significant lost productivity for both the affected individuals and their caregivers, further exacerbating the economic hardship. A family’s primary breadwinner may be unable to work consistently, leading to reduced income and an inability to meet basic needs.
- High cost of hospitalization and treatment.
- Loss of income due to inability to work consistently.
- Financial strain on families, leading to debt.
- Reduced access to other essential needs (food, education).
- Increased caregiver burden, impacting their productivity.
Challenges in Accessing Healthcare and Treatment
Access to appropriate healthcare for sickle cell disease remains a major challenge in Rajasthan’s remote tribal districts. Geographical isolation, lack of transportation, inadequate healthcare infrastructure, and a shortage of trained medical professionals all contribute to significant barriers. Many families lack awareness of available resources or struggle to navigate the complex healthcare system. This lack of access often leads to delayed diagnosis and treatment, resulting in severe complications and poorer health outcomes.Strategies to improve healthcare access include establishing mobile health clinics that reach remote villages, training community health workers to provide basic care and education, improving transportation infrastructure, and creating awareness campaigns to educate communities about the disease and available resources.
Telemedicine could also play a significant role in connecting patients with specialists in urban centers. These combined strategies aim to reduce the distance and barriers that prevent timely access to critical care.
Impact on Education and Employment
Sickle cell disease significantly impacts educational and employment opportunities within affected communities. Frequent hospitalizations and debilitating pain episodes often lead to absenteeism from school, hindering academic progress and future prospects. Children with sickle cell disease may fall behind their peers, impacting their self-esteem and limiting their future career options. Similarly, adults with the disease may face discrimination in the workplace due to their condition, limiting their employment opportunities and income potential.
The long-term consequences include increased poverty, limited social mobility, and perpetuation of the cycle of disadvantage within these communities. For example, a young person with sickle cell disease might be unable to complete their education, leading to limited job prospects and a lower earning potential throughout their life, further impacting their family’s economic stability.
Healthcare Infrastructure and Treatment Strategies
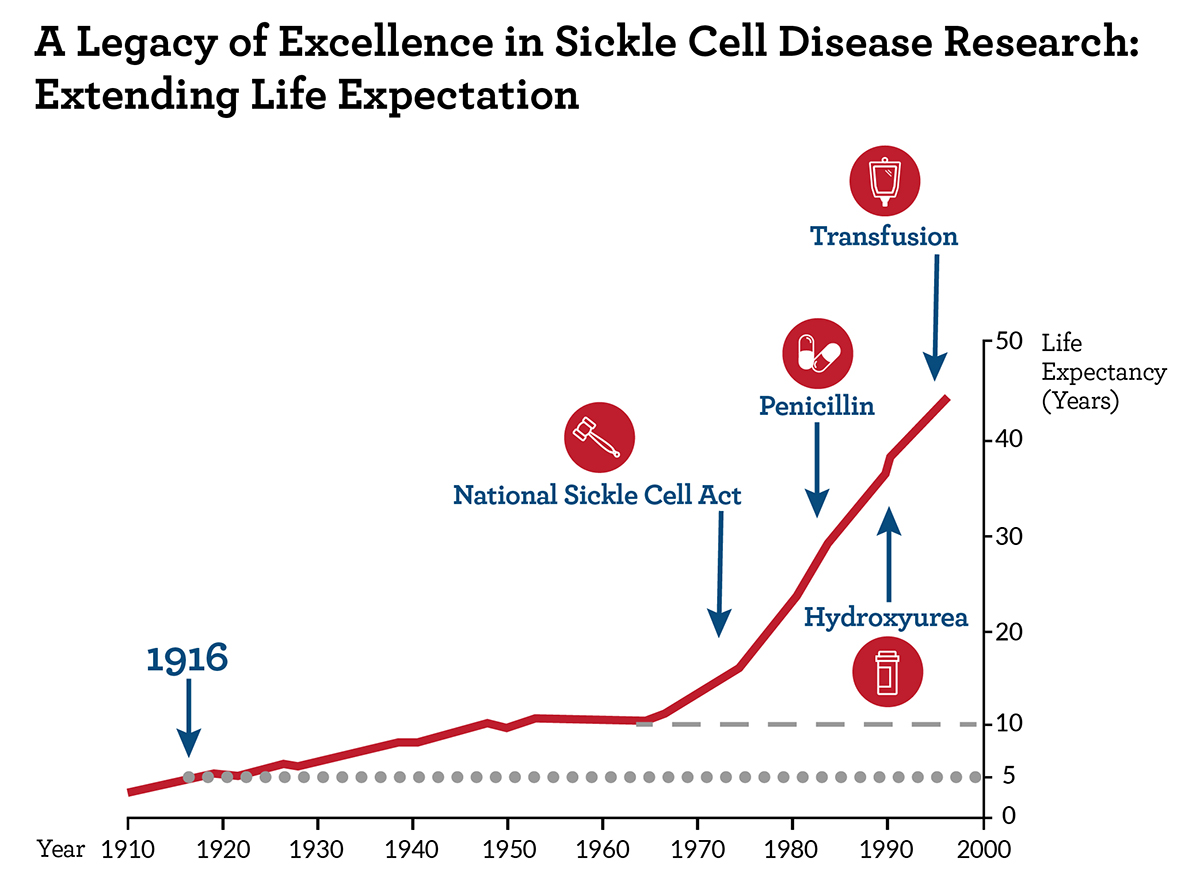
Source: nih.gov
The alarming surge of sickle cell disease (SCD) cases in Rajasthan’s tribal districts necessitates a thorough examination of the healthcare infrastructure and treatment strategies currently in place. The stark reality is that the availability and accessibility of appropriate care significantly vary across the region, leading to considerable disparities in health outcomes. This section will analyze the current state of healthcare infrastructure, compare treatment options across different regions, and identify key challenges and potential solutions.
The healthcare infrastructure in Rajasthan’s tribal districts faces significant challenges in effectively managing SCD. Limited resources, geographical isolation, and a lack of awareness contribute to poor access to diagnosis, treatment, and ongoing care. The following table provides a snapshot of the situation, though precise data is often difficult to obtain due to reporting inconsistencies.
Current Healthcare Infrastructure in Rajasthan’s Tribal Districts
| District | Number of Hospitals | Availability of Specialized Care (Hematology/Blood Transfusion) | Access to Medication (Hydroxyurea, etc.) |
|---|---|---|---|
| Example District A | 2 (1 primary health center, 1 community health center) | None | Limited; infrequent supply chain disruptions |
| Example District B | 1 District Hospital | Limited; occasional visits by specialists | Sporadic availability; high out-of-pocket costs |
| Example District C | 3 (including one with a small blood bank) | Minimal; basic blood transfusion services available | Relatively better access compared to other districts, but still inconsistent |
Note: This data is illustrative and based on reported estimates. Accurate, comprehensive data collection is crucial for effective resource allocation.
Comparison of Treatment Options: Rural vs. Urban
Treatment options for SCD in Rajasthan’s tribal districts are significantly limited compared to those available in urban centers. Urban areas generally have better access to specialized hematologists, advanced diagnostic tools (like Hb electrophoresis), regular blood transfusions, and newer medications like hydroxyurea. In contrast, rural districts often rely on basic primary healthcare facilities with limited diagnostic capabilities and medication availability.
This disparity leads to delayed diagnosis, inadequate management of acute crises, and increased morbidity and mortality. For instance, a patient experiencing a vaso-occlusive crisis in a rural area might face significant delays in receiving appropriate pain management and blood transfusion, potentially leading to severe complications.
Challenges and Potential Solutions for Effective and Affordable Treatment
Providing effective and affordable treatment for SCD in resource-limited settings presents numerous challenges. These include:
1. Lack of Awareness and Early Diagnosis: Many individuals in tribal communities are unaware of SCD, leading to delayed diagnosis and treatment. Community-based awareness programs and accessible screening initiatives are essential.
2. Inadequate Healthcare Infrastructure: The scarcity of specialized healthcare facilities, trained personnel, and essential medications poses a significant barrier. Investing in infrastructure development, training healthcare workers, and establishing robust supply chains are crucial.
3. High Cost of Treatment: The cost of medications, blood transfusions, and specialized care can be prohibitive for many families. Government subsidies, affordable generic medications, and financial assistance programs are necessary to ensure equitable access.
4. Geographical Barriers: The remoteness of many tribal districts makes access to healthcare challenging. Mobile medical units, telemedicine initiatives, and improved transportation networks can help bridge this gap.
5. Lack of Data and Research: Limited data on the prevalence and impact of SCD hinders effective planning and resource allocation. Investing in epidemiological studies and research is crucial for developing targeted interventions.
Public Health Initiatives and Awareness Campaigns
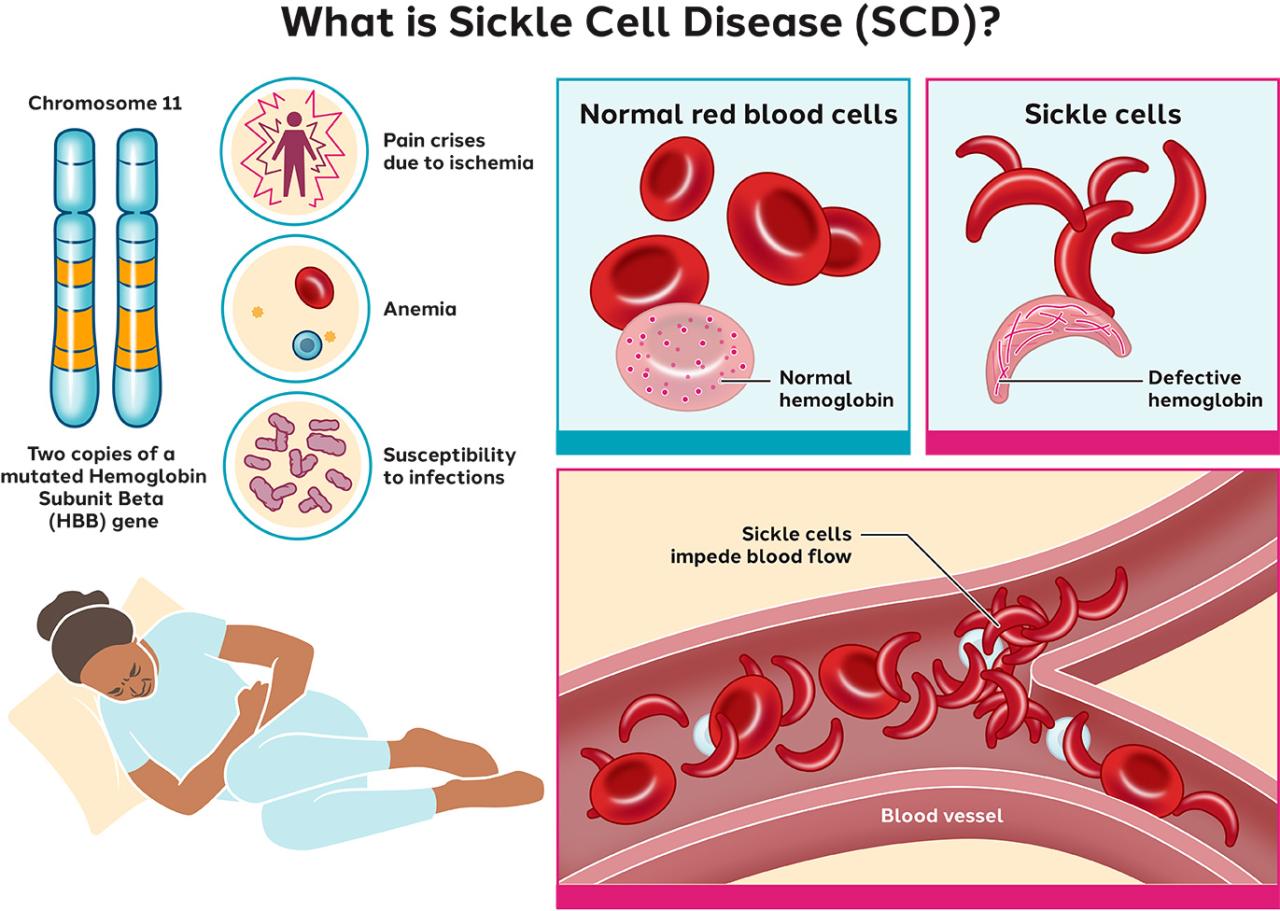
Source: sangamo.com
The staggering number of individuals affected by sickle cell disease (SCD) in Rajasthan’s tribal districts necessitates a comprehensive and multifaceted approach involving robust public health initiatives and impactful awareness campaigns. Addressing this crisis requires not only improved healthcare infrastructure and treatment but also proactive strategies to educate communities and prevent future cases. This section will explore existing initiatives, propose a new awareness campaign, and detail the crucial role of genetic counseling and prenatal screening.Existing public health initiatives aimed at addressing sickle cell disease in Rajasthan’s tribal communities are currently limited and often lack the resources and reach needed for significant impact.
While some government programs exist, their effectiveness is hampered by several factors, including limited awareness, geographical challenges, and inadequate healthcare infrastructure.
Existing Public Health Initiatives and Their Effectiveness
The effectiveness of current public health initiatives in combating SCD in Rajasthan’s tribal areas is unfortunately quite low. A lack of widespread knowledge about the disease, coupled with poor access to healthcare, contributes to delayed diagnosis and inadequate management. Many individuals remain undiagnosed, leading to significant morbidity and mortality.
- Government-run health camps: These sporadic camps offer limited testing and counseling services, often reaching only a small fraction of the affected population. Their impact is further reduced by the infrequent nature of the camps and the lack of follow-up care.
- NGO initiatives: Several non-governmental organizations (NGOs) work to raise awareness and provide support to affected families. However, these initiatives are often underfunded and struggle to reach the remote tribal communities. Their effectiveness varies greatly depending on the NGO’s resources and reach.
- School-based awareness programs: A few schools in affected areas have incorporated SCD education into their curriculum. However, the extent of these programs and their effectiveness in changing community attitudes and behaviors are not well documented.
Proposed Public Awareness Campaign
A comprehensive public awareness campaign is crucial to educate the community about SCD, its causes, symptoms, prevention, and management. The campaign should utilize a multi-pronged approach targeting various communication channels and tailoring messages to the specific needs and understanding of the target audience. Target Audience: The primary target audience includes individuals residing in Rajasthan’s tribal districts, particularly those of reproductive age.
Secondary audiences include healthcare providers, community leaders, and school teachers. Communication Channels: The campaign will utilize a combination of channels to maximize reach and impact. These include:
- Community meetings and gatherings: Interactive sessions using local languages and culturally sensitive materials.
- Radio broadcasts and announcements: Regular broadcasts in local dialects to disseminate key information.
- Street plays and puppet shows: Engaging performances to convey complex information in a simple and memorable way.
- Educational pamphlets and posters: Visually appealing materials with clear and concise information.
- Social media platforms (where accessible): Utilizing platforms like WhatsApp and Facebook to share information and engage with the community.
Campaign Messages: The messages will emphasize:
- Understanding SCD: Simple explanations of the disease’s causes, symptoms, and complications.
- Prevention through genetic counseling and prenatal screening: Emphasizing the importance of early detection and family planning.
- Importance of early diagnosis and treatment: Highlighting the benefits of timely medical intervention.
- Dispelling myths and misconceptions: Addressing common misconceptions surrounding SCD and its transmission.
- Support and resources: Providing information about available support groups and healthcare facilities.
Genetic Counseling and Prenatal Screening Programs
Genetic counseling and prenatal screening programs are essential for reducing the incidence of SCD in future generations. These programs provide individuals and couples with information about their risk of having a child with SCD, and offer options for managing that risk. Implementation requires a multi-pronged strategy: Recommendations for Implementation:
- Establish easily accessible genetic counseling centers: These centers should be strategically located in affected districts and staffed with trained genetic counselors who are fluent in local languages.
- Integrate prenatal screening into routine antenatal care: Offer affordable and accessible prenatal screening for SCD to all pregnant women, particularly those in high-risk communities.
- Train healthcare providers: Provide comprehensive training to healthcare providers on SCD, genetic counseling, and prenatal screening techniques.
- Develop culturally appropriate educational materials: Create educational materials that are sensitive to the cultural beliefs and practices of the tribal communities.
- Implement community-based education programs: Conduct educational programs in villages and communities to raise awareness about the benefits of genetic counseling and prenatal screening.
- Establish a robust referral system: Develop a system to ensure that individuals identified as having a high risk of SCD or carrying the sickle cell trait receive appropriate follow-up care and counseling.
Research and Future Directions
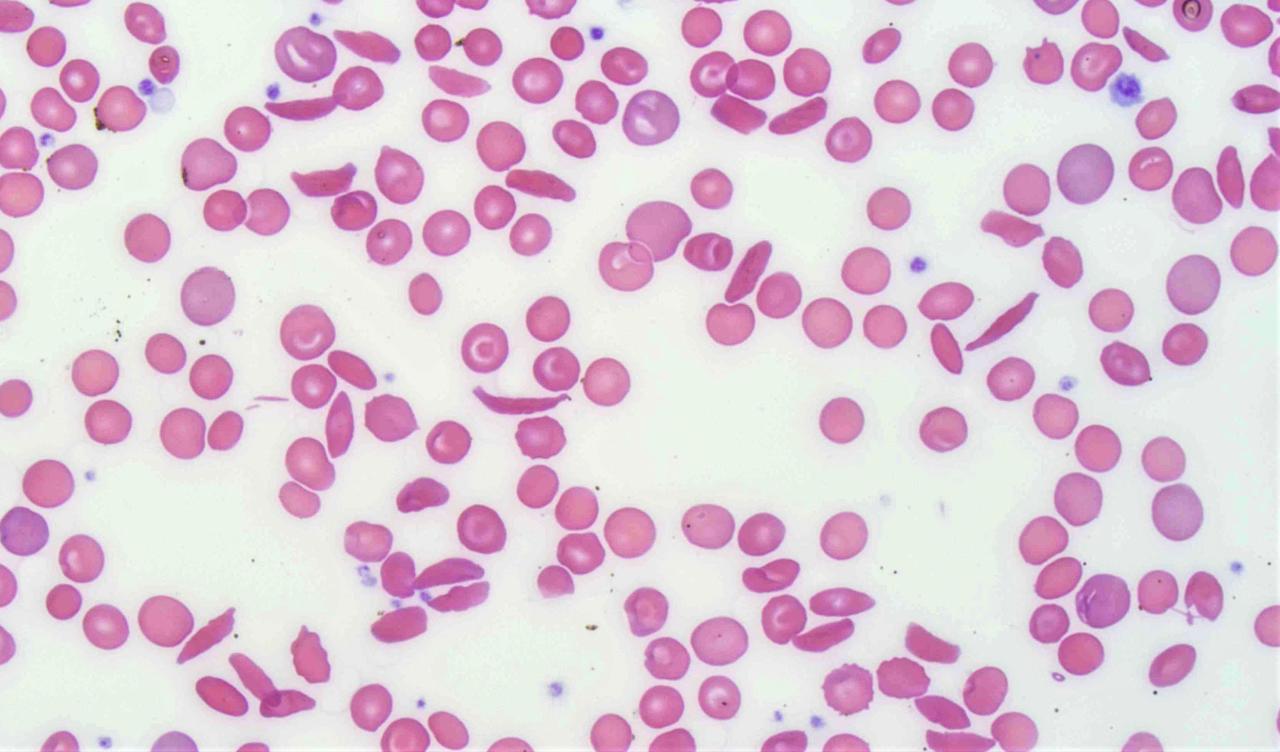
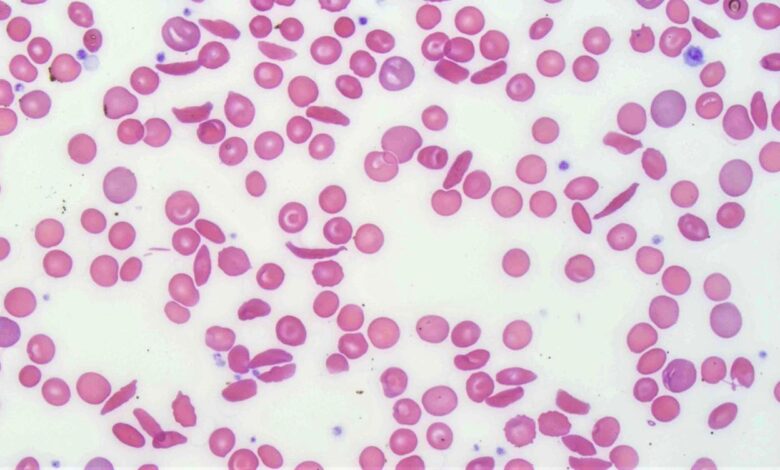
Source: pathologyoutlines.com
The staggering number of sickle cell disease (SCD) cases in Rajasthan’s tribal districts necessitates a robust research agenda to address the unique challenges faced by these communities. Understanding the genetic underpinnings of the disease’s high prevalence, coupled with the development of culturally appropriate and sustainable management strategies, is crucial for improving the lives of those affected. This requires a multi-faceted approach encompassing genetic studies, epidemiological investigations, and the evaluation of healthcare interventions.The high prevalence of SCD in Rajasthan’s tribal populations presents a significant opportunity for impactful research.
Further investigation is needed to unravel the complex interplay of genetic and environmental factors driving this public health crisis. This knowledge will inform the development of targeted interventions and improve the long-term health outcomes for affected individuals.
Key Research Priorities
Prioritizing research in several key areas will be essential to effectively combat SCD in Rajasthan’s tribal communities. These priorities should include:
- Comprehensive genetic mapping of the SCD affected population to identify specific mutations prevalent in these communities and their association with disease severity. This could involve comparing the genetic profiles of affected individuals with those from other regions of Rajasthan and India to identify unique mutations or haplotypes. For example, a study could focus on the prevalence of specific beta-globin gene mutations, such as HbS, HbC, and HbE, and their frequencies within different tribal groups.
This would help tailor genetic counseling and newborn screening programs to the specific needs of each population.
- Investigating the role of environmental factors, such as malnutrition, infectious diseases, and exposure to environmental toxins, in influencing disease severity and complications. This could involve detailed epidemiological studies assessing the correlation between environmental exposures and the clinical presentation of SCD in these communities. For instance, researchers could analyze the impact of dietary deficiencies on the frequency of vaso-occlusive crises or the role of infections in triggering acute chest syndrome.
- Developing and evaluating culturally appropriate and accessible healthcare interventions, including improved diagnostic tools, treatment strategies, and patient education programs. This might include exploring the feasibility of telemedicine to improve access to specialized care in remote areas or developing educational materials in local languages to empower patients and their families to manage their condition effectively. For example, a pilot study could assess the effectiveness of a community-based health worker program in providing regular home visits and health education to families affected by SCD.
- Assessing the long-term health and socioeconomic outcomes of individuals with SCD in these communities. This could involve longitudinal studies tracking the health status, educational attainment, and employment opportunities of individuals with SCD compared to their unaffected peers. Data could reveal the impact of SCD on individuals’ quality of life and inform policies aimed at improving their social inclusion and economic well-being.
This could include assessing the effectiveness of existing social support programs.
Understanding Genetic Variations and Environmental Factors, Sickle cell disease surges in rajasthan tribal districts over ten thousand affected says report
The exceptionally high prevalence of SCD in specific tribal populations of Rajasthan suggests a complex interplay of genetic and environmental factors. Further research is needed to pinpoint the specific genetic variations responsible for the heightened susceptibility within these communities. This includes investigating potential founder effects, genetic drift, and the interaction of multiple genes influencing disease severity. Simultaneously, studies should focus on identifying environmental factors, such as malnutrition, infections, and access to healthcare, that contribute to the observed high prevalence and disease burden.
A combined approach utilizing genomic sequencing, epidemiological studies, and environmental risk assessments will be crucial to understanding this complex interplay. For instance, comparing the genetic profiles of affected individuals within different tribal groups in Rajasthan and analyzing the correlation between malnutrition rates and the severity of SCD symptoms within these groups would provide valuable insights.
Strategies for Improving Long-Term Management and Care
Improving the long-term management and care of individuals with SCD in Rajasthan’s tribal communities requires a multi-pronged approach. This includes enhancing access to timely and accurate diagnosis, providing affordable and accessible treatment, and implementing comprehensive patient education programs. Furthermore, strengthening healthcare infrastructure, training healthcare professionals, and developing culturally appropriate healthcare strategies are vital. For example, establishing mobile health clinics to provide regular check-ups and treatment in remote areas, or implementing community-based support groups to provide psychosocial support and education to affected families, could significantly improve the long-term outcomes for individuals with SCD in these communities.
Moreover, integrating SCD management into existing primary healthcare programs will ensure sustainable and accessible care for affected individuals.
Outcome Summary
The sickle cell crisis in Rajasthan’s tribal districts is a stark reminder of the health inequalities that plague many parts of the world. While the sheer number of affected individuals is alarming, the story extends far beyond the statistics. It’s a story of families struggling against overwhelming odds, communities grappling with a devastating disease, and a healthcare system desperately needing support.
Addressing this crisis requires a multi-pronged approach, encompassing improved healthcare infrastructure, increased public awareness, and targeted research to better understand and treat this debilitating disease. Only through concerted effort can we hope to alleviate the suffering of those affected and prevent future generations from facing this same burden.
Expert Answers
What are the common symptoms of sickle cell disease?
Symptoms can vary, but common ones include pain crises, fatigue, swelling in hands and feet, and frequent infections.
Is sickle cell disease hereditary?
Yes, it’s an inherited blood disorder. Both parents must carry the sickle cell trait to pass it on to their child.
What kind of treatment is available for sickle cell disease?
Treatment options range from pain management and blood transfusions to more advanced therapies like bone marrow transplants, depending on the severity.
Are there any preventative measures for sickle cell disease?
Genetic counseling and prenatal screening can help identify couples at risk and allow them to make informed decisions about family planning.
