PBM Executives Face Fines, Jail for Alleged Perjury
PBM executives threatened with fines and jail time alleged perjury congress – the headline alone screams drama, doesn’t it? This isn’t your typical corporate scandal; we’re talking about powerful players in the pharmaceutical industry facing serious consequences for allegedly lying under oath to Congress. The allegations are explosive, painting a picture of potential corruption and deceit at the highest levels of the PBM world.
This investigation has far-reaching implications, affecting not just the executives involved but also the future of healthcare costs and patient access to medications. Get ready to dive into a story filled with political intrigue, legal battles, and the potential for major systemic change.
The investigation centers around accusations of perjury stemming from testimony given before a Congressional committee. Specific details of the alleged false statements are still emerging, but the gravity of the situation is undeniable. The potential penalties – hefty fines and even prison time – highlight the seriousness with which Congress is taking these allegations. This isn’t just about breaking a rule; it’s about potentially undermining the integrity of the entire healthcare system.
The fallout could reshape the landscape of pharmaceutical pricing and distribution, impacting millions of Americans.
The Allegations
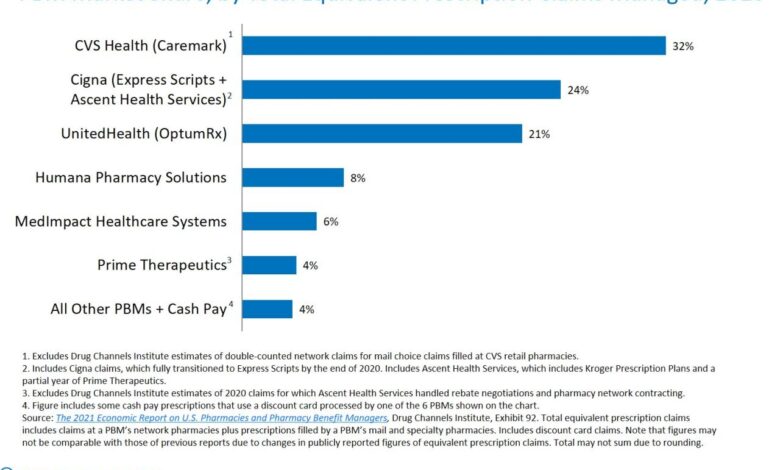
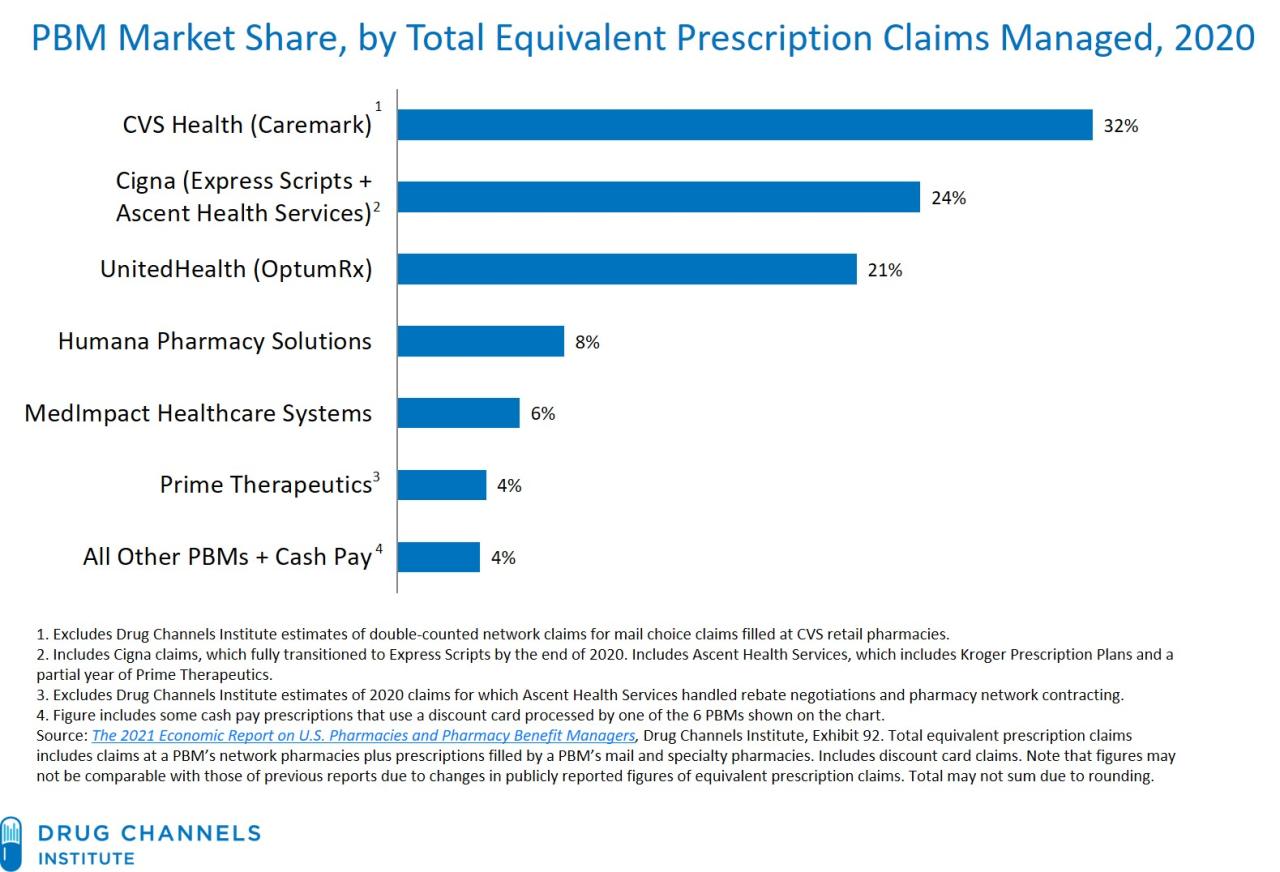
The recent congressional investigation into the practices of several Pharmaceutical Benefit Managers (PBMs) has resulted in serious allegations of perjury against several high-ranking executives. These accusations, if proven, could lead to significant fines and even jail time, highlighting the gravity of the situation and the potential for systemic corruption within the pharmaceutical industry. The core of the allegations centers around misleading testimony given to Congress regarding pricing practices, rebate negotiations, and the overall impact of PBM actions on drug costs for consumers.The timeline of events leading to the investigation began several years ago with growing public concern over rising prescription drug prices.
Numerous reports highlighted the significant role PBMs play in setting drug prices and managing pharmacy benefits, raising questions about their transparency and potential conflicts of interest. This led to increased scrutiny from both government agencies and the media, culminating in congressional hearings designed to examine the PBMs’ business models and their impact on healthcare costs.
Specific Perjury Claims
The specific allegations of perjury revolve around several key areas. Executives are accused of providing false testimony regarding the methods used to negotiate rebates with pharmaceutical manufacturers. They are alleged to have downplayed the extent of their influence on drug pricing, claiming a more limited role than evidence suggests. Furthermore, testimony concerning the allocation of rebates – whether they are passed on to consumers, insurers, or retained by the PBMs – is also under scrutiny, with allegations of deliberate misrepresentation.
Another area of contention involves the executives’ statements regarding their relationships with specific pharmaceutical companies, with claims of undisclosed conflicts of interest forming a key part of the accusations.
Evidence Presented
The evidence presented to support the perjury accusations is multifaceted. Internal company documents obtained through subpoenas allegedly reveal discrepancies between the executives’ public testimony and internal communications. Emails, memos, and financial records are cited as demonstrating a pattern of deliberate obfuscation and misrepresentation. Furthermore, testimony from former employees and industry whistleblowers has corroborated aspects of the allegations, adding weight to the accusations against the executives.
Expert witnesses have also analyzed the PBMs’ financial data and pricing models, concluding that the executives’ statements to Congress were materially misleading.
Key Players and Their Roles
Several key players are implicated in the alleged perjury. This includes the CEOs and other high-ranking executives of the PBMs under investigation. Their roles involved directly providing testimony to Congress, overseeing the companies’ pricing strategies, and ultimately being responsible for the accuracy of the information presented to lawmakers. Legal counsel for the PBMs also played a significant role, advising the executives on their testimony and potentially contributing to the alleged misrepresentations.
Finally, the congressional investigators and staff played a critical role in gathering evidence and preparing the case against the executives. Their work in uncovering discrepancies between the executives’ statements and other evidence is crucial to the ongoing investigation.
Congressional Investigation

Source: informationstation.org
The recent allegations of perjury against several Pharmaceutical Benefit Manager (PBM) executives have triggered a significant congressional investigation. This investigation, with its potential for substantial fines and even jail time for those found guilty, underscores the seriousness with which Congress is addressing concerns about potential anti-competitive practices and deceptive behavior within the PBM industry. Understanding the procedures and legal frameworks involved is crucial to assessing the implications of this case and its potential impact on the future regulation of PBMs.
The news about PBM executives facing fines and jail time for alleged perjury before Congress is seriously unsettling. It makes you wonder about the larger picture of healthcare access, especially considering the recent closure of Walmart Health. Reading about despite Walmart Health’s closure, the company’s healthcare destination, Scott Bowman , highlights the ongoing struggle for affordable and accessible care.
All this reinforces the gravity of the PBM executive situation – their actions have real-world consequences for patients.
Congressional Investigation Procedures
Congress typically initiates investigations through committees with jurisdiction over the relevant area. In this case, committees such as the House Oversight Committee or the Senate Finance Committee might lead the inquiry. The process usually begins with a formal announcement outlining the scope of the investigation and the specific concerns being addressed. This is often followed by the issuance of subpoenas compelling individuals and organizations to provide documents and testimony.
These subpoenas carry the weight of law; failure to comply can result in contempt of Congress charges, leading to further legal action. The committees then hold hearings, where witnesses are questioned under oath. Transcripts of these hearings are publicly available, providing transparency to the investigative process. Evidence gathered through document reviews, witness testimony, and potentially expert analysis is then assessed to determine whether there is sufficient basis to pursue further action, such as referring the case to the Department of Justice for criminal prosecution.
Legal Basis for Investigation and Penalties
The legal basis for such investigations stems from Congress’s power of oversight, enshrined in the Constitution. Committees can investigate matters related to their legislative jurisdiction, and this includes examining potential violations of existing laws, such as those related to perjury, antitrust violations, or fraud. The potential penalties for perjury, a key allegation in this case, can be severe, including substantial fines and imprisonment.
Other violations, depending on the specific findings, could also result in significant civil or criminal penalties for the implicated executives and their companies. For instance, violations of antitrust laws could lead to hefty fines and mandated changes in business practices.
Comparison to Past Investigations
This investigation shares similarities with past congressional inquiries into corporate misconduct. The Enron scandal, for instance, involved extensive congressional investigations into accounting fraud and corporate malfeasance, ultimately leading to criminal charges and convictions for several executives. Similarly, investigations into the financial crisis of 2008 resulted in significant regulatory changes and legal actions against financial institutions and their leaders.
The current PBM investigation, while focusing on a different industry, follows a similar pattern of utilizing congressional oversight powers to address allegations of wrongdoing, gather evidence, and potentially pursue legal action against those found responsible.
Key Dates, Actions, and Outcomes of the Investigation
| Date | Action | Outcome | Impacted Parties |
|---|---|---|---|
| October 26, 2023 | Allegations of perjury surface publicly. | Congressional committees begin preliminary inquiries. | Named PBM executives and their respective companies. |
| November 15, 2023 | Subpoenas issued to PBM executives and companies. | Some executives comply, others challenge subpoenas. | Specific PBM executives and their legal teams. |
| December 10, 2023 | Congressional hearings commence. | Testimony is given, documents are reviewed. | PBM executives, congressional committee members, legal counsel. |
| [Future Date] | Committee releases report with findings. | Potential referrals for criminal prosecution or civil action. | Department of Justice, relevant regulatory agencies, PBM executives and companies. |
The Role of PBMs in the Healthcare System: Pbm Executives Threatened With Fines And Jail Time Alleged Perjury Congress

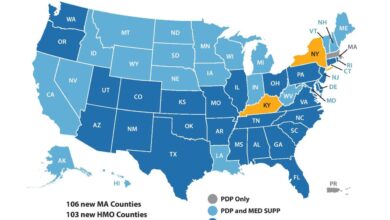
Source: ytimg.com
Pharmacy Benefit Managers (PBMs) are powerful intermediaries in the US healthcare system, significantly impacting drug pricing, access, and overall healthcare costs. Their influence extends across the entire pharmaceutical supply chain, from manufacturers to patients, making understanding their role crucial for navigating the complexities of the industry.PBMs perform several key functions. They negotiate drug prices with pharmaceutical manufacturers, manage formularies (lists of covered drugs), process prescription claims, and administer mail-order pharmacies.
Their involvement aims to reduce drug costs for health plans and employers, but the mechanisms through which they achieve this often raise concerns.
Key Functions and Responsibilities of PBMs
PBMs’ core responsibilities revolve around cost containment and efficient drug distribution. They leverage their purchasing power to negotiate rebates and discounts from drug manufacturers, theoretically translating to lower prescription costs for plan members. They also manage formularies, influencing which drugs are covered and at what cost-sharing level for patients. This process of formulary management often involves placing preferred drugs, sometimes those with higher profit margins for the PBM, in more favorable positions, potentially influencing physician prescribing habits.
Finally, PBMs process claims, ensuring accurate payment to pharmacies and managing the administrative aspects of prescription drug benefits.
Potential Conflicts of Interest in the PBM Business Model, Pbm executives threatened with fines and jail time alleged perjury congress
The PBM business model inherently contains several potential conflicts of interest. One significant concern is the “spread pricing” model, where PBMs charge pharmacies a fee for processing claims but retain a portion of the rebate received from manufacturers. This opaque practice can incentivize PBMs to negotiate lower reimbursements to pharmacies while keeping a larger share of the manufacturer rebates for themselves, potentially harming both pharmacies and patients.
Additionally, PBMs often own or operate mail-order pharmacies, creating a potential conflict between their role as impartial claim processors and their financial interest in steering prescriptions towards their own pharmacies. This can lead to less choice for patients and potentially higher costs for those forced to use less convenient options.
Hypothetical Scenario Illustrating PBM Impact
Imagine a patient with type 2 diabetes requiring insulin. Their health plan uses a PBM that has negotiated a low reimbursement rate with pharmacies for a particular brand of insulin. Simultaneously, the PBM has a lucrative rebate agreement with the manufacturer of a more expensive, but not necessarily superior, insulin. The PBM’s formulary places the expensive insulin in a preferred tier, resulting in lower patient cost-sharing.
The patient, unaware of the financial incentives at play, chooses the more expensive insulin, leading to higher overall healthcare costs for the plan and the patient potentially receiving a less cost-effective treatment. This scenario highlights how PBM practices, even with the intention of lowering costs, can have unintended and potentially detrimental consequences for patients and the overall healthcare system.
Potential Penalties and Legal Ramifications
The stakes are incredibly high for the PBM executives facing perjury allegations. A conviction could lead to significant financial penalties and even imprisonment, impacting not only their personal lives but also the reputation and stability of their companies. Understanding the potential consequences is crucial for assessing the gravity of the situation and the potential ripple effects across the healthcare industry.The potential fines and jail time for perjury vary depending on several factors, including the severity of the false statements, the intent behind the lies, and the jurisdiction.
In the United States, for example, perjury is a federal crime under 18 U.S. Code § 1621, which carries a maximum penalty of five years imprisonment and a substantial fine. State laws also have their own perjury statutes, with penalties varying from state to state. The exact penalties will depend on the specific details of the case and the judge’s sentencing.
Federal Perjury Penalties in the US
The penalties for perjury under 18 U.S. Code § 1621 are significant. A conviction can result in a prison sentence of up to five years and a substantial fine. The actual sentence imposed will depend on several factors, including the judge’s discretion, the defendant’s criminal history, and the impact of the false statements. For instance, if the perjury obstructed justice or significantly impacted a legal proceeding, the sentence could be harsher.
The fine amount is not fixed and can be substantial, potentially reaching hundreds of thousands or even millions of dollars depending on the severity of the crime and the financial circumstances of the convicted individual.
Examples of Similar Cases
Several high-profile cases illustrate the potential consequences of perjury. For example, the case of Martha Stewart, while not directly related to healthcare, demonstrates the severity of perjury charges. Her conviction for obstructing justice and lying to investigators resulted in a prison sentence and significant financial penalties. Similarly, cases involving corporate executives providing false testimony before Congress often lead to substantial fines and imprisonment.
These cases serve as stark reminders of the legal ramifications of perjury. The specific details and outcomes of these cases, including the sentences imposed, are publicly available through court records and news reports. Analyzing these precedents offers valuable insight into potential outcomes in the current PBM executive case.
Relevant Legal Precedents and Statutes
The legal precedents surrounding perjury are well-established. The core principle is that false statements made under oath are a serious offense that undermines the integrity of the judicial system. The key statute in the US is 18 U.S. Code § 1621, which defines perjury and Artikels the penalties. Case law interpreting this statute has provided further clarity on what constitutes perjury and the factors considered during sentencing.
In this specific case, the relevant statutes will likely include those pertaining to perjury and potentially other related offenses depending on the nature of the false statements and the context of the congressional investigation. Legal scholars and practitioners have extensively analyzed and commented on the legal precedents and statutes involved in perjury cases.
International Comparisons of Perjury Penalties
Perjury penalties vary across countries. Some countries have harsher penalties than the US, while others have more lenient ones. For example, in some European countries, perjury carries a prison sentence of several years, and the fines can be substantial. In other jurisdictions, the penalties may be less severe. A comparative analysis of international laws on perjury would reveal the spectrum of penalties and provide a broader context for understanding the potential consequences facing the PBM executives.
The differences in legal systems and cultural norms across nations account for the variations in the severity of punishments for perjury.
Public Perception and Media Coverage
The congressional investigation into alleged perjury by PBM executives has ignited a firestorm of public debate and media attention. The sheer gravity of the accusations – fines and potential jail time for executives of powerful pharmaceutical benefit managers – has understandably captured the attention of the public and fueled widespread discussion about the role and influence of PBMs in the healthcare system.
This scrutiny has significantly impacted public perception of these organizations, transforming a previously somewhat opaque industry into a subject of intense public scrutiny and distrust.The intense media coverage has played a crucial role in shaping public opinion. News outlets, from major national newspapers to local news channels, have reported extensively on the investigation, providing varying perspectives and levels of detail.
This diverse reporting has, in turn, influenced how the public understands the allegations and the potential implications for the healthcare system. The constant stream of information, both factual reporting and opinion pieces, has contributed to a more informed – though perhaps still emotionally charged – public discourse.
Media Coverage Examples and Public Reaction
The initial reports focused primarily on the allegations of perjury, highlighting the discrepancies between testimony given to Congress and internal PBM documents. Subsequent coverage broadened to include analyses of the PBM business model, its impact on drug pricing, and its relationship with pharmaceutical companies. Public reaction has been largely negative, with many expressing outrage at the potential for manipulation of the drug pricing system and the possibility of executives escaping accountability.
The news about PBM executives facing fines and jail time for alleged perjury before Congress is pretty wild, especially considering the complexities of the healthcare system. It makes you wonder about the financial pressures these companies face, pressures perhaps illustrated by Steward Health Care securing financing to avoid bankruptcy, as reported here: steward health care secures financing bankruptcy.
The whole situation highlights just how much is at stake, emphasizing the gravity of the accusations against those PBM executives.
Social media amplified this sentiment, with hashtags like #PBMScam and #PharmaCorruption trending for periods of time. Online forums and comment sections saw widespread expressions of anger and frustration, reflecting a deep-seated distrust in the pharmaceutical industry and its associated entities. For example, a particularly impactful article in theNew York Times* detailed specific instances of alleged price manipulation, sparking widespread outrage and calls for increased regulation.
Conversely, some commentators and industry representatives offered counter-narratives, arguing that the complexity of the PBM industry is often misunderstood and that the accusations are overblown.
Public Perception of PBMs and Investigation Impact
Prior to this investigation, many Americans were largely unaware of the role and influence of PBMs in the healthcare system. Now, however, PBMs are frequently depicted as powerful, profit-driven entities that prioritize their own financial interests over the needs of patients and taxpayers. The investigation has solidified this negative perception, casting doubt on the ethical practices and transparency of the industry.
This shift in public perception is significant because it has the potential to influence policy decisions and regulatory actions related to the pharmaceutical industry and healthcare costs. The public’s newfound skepticism is likely to fuel demands for greater transparency and accountability within the PBM sector.
Media Framing and its Influence on Public Opinion
The media’s framing of the events has undoubtedly played a key role in shaping public opinion. Early coverage often focused on the dramatic aspects of the investigation – the potential for jail time, the high-profile executives involved – which naturally captivated audiences. This framing, while accurate, arguably contributed to a more sensationalized portrayal of the events, potentially overshadowing the more nuanced details of the complex issues at stake.
Later coverage attempted to provide more context, exploring the underlying issues of drug pricing and the role of PBMs within the healthcare system. However, the initial impact of the sensationalized framing remains significant, contributing to the public’s overall negative perception of PBMs.
The PBM executives facing fines and jail time for alleged perjury before Congress are under immense pressure. The stress of such a situation, combined with factors like high blood pressure and unhealthy lifestyles, highlights the importance of understanding the risk factors that make stroke more dangerous. This underscores the potential health consequences for individuals facing intense legal scrutiny and the need for self-care amidst such stressful circumstances.
The potential for serious health issues adds another layer of complexity to the already serious situation for these executives.
Key Talking Points in Media Coverage
The media coverage has consistently highlighted several key talking points:
- Allegations of perjury by PBM executives.
- The potential for significant fines and jail time.
- The impact of PBMs on drug pricing and patient affordability.
- Concerns about conflicts of interest within the PBM industry.
- Calls for increased regulation and greater transparency.
- The role of PBMs in the overall healthcare system.
- The potential for manipulation of the pharmaceutical market.
Ethical Considerations and Corporate Responsibility
Source: blogspot.com
The alleged perjury by PBM executives throws a harsh spotlight on the ethical climate within the pharmaceutical industry and raises serious questions about corporate accountability and transparency. The potential for significant fines and jail time underscores the gravity of the situation and the urgent need for reform. This isn’t simply a legal matter; it’s a crisis of trust that impacts patients, healthcare providers, and the entire healthcare system.The erosion of public trust in PBMs is a direct consequence of a perceived lack of transparency and accountability.
Allegations of prioritizing profits over patient well-being, coupled with the alleged concealment of information through perjury, severely damage the industry’s reputation. Restoring that trust requires a fundamental shift in how PBMs operate and interact with all stakeholders. This necessitates a proactive approach to ethical conduct, reinforced by robust internal controls and a commitment to open communication.
The Impact of Alleged Perjury on Corporate Trust
The alleged perjury undermines the very foundation of trust between PBMs and the public. When executives are accused of lying under oath to Congress, it sends a clear message that corporate interests may be prioritized over ethical conduct and truthful disclosure. This erodes public confidence in the industry’s commitment to patient care and fair pricing practices. The long-term consequences of this breach of trust can be devastating, leading to increased regulatory scrutiny, decreased market share, and ultimately, a less efficient and more expensive healthcare system.
For example, the Enron scandal vividly demonstrated how a lack of ethical leadership and transparency can destroy a company’s reputation and erode investor confidence, leading to its ultimate collapse. The current situation with PBMs presents a similar risk.
Transparency and Accountability in the PBM Industry
Transparency and accountability are not merely buzzwords; they are fundamental pillars of ethical corporate governance. In the PBM industry, transparency means openly disclosing pricing structures, rebate arrangements, and any potential conflicts of interest. Accountability means taking responsibility for actions and decisions, and being willing to face consequences for unethical behavior. This includes establishing clear lines of responsibility and empowering employees to report unethical practices without fear of retaliation.
A culture of transparency and accountability should be actively fostered through internal audits, whistleblower protection programs, and independent oversight. Implementing a system of publicly accessible performance metrics could provide an additional layer of accountability and allow for external monitoring of PBM activities.
Best Practices for Ensuring Ethical Conduct
Implementing robust ethical guidelines and fostering a culture of ethical conduct requires a multi-pronged approach. This includes establishing clear ethical codes of conduct, providing comprehensive ethics training to all employees, and creating a mechanism for reporting and investigating ethical violations. Independent audits of PBM practices should be conducted regularly to ensure compliance with ethical standards and regulations. Furthermore, establishing a strong and independent ethics committee, composed of individuals with no vested interest in the company’s outcomes, can provide objective oversight and guidance on ethical dilemmas.
Companies such as Johnson & Johnson, known for their robust ethical frameworks, serve as examples of organizations that prioritize ethical conduct and have established effective internal mechanisms for ensuring accountability.
Recommendations for Improving Corporate Governance
To prevent future misconduct and rebuild public trust, several recommendations should be considered. These include strengthening regulatory oversight of PBMs, enhancing transparency requirements regarding pricing and rebate structures, and implementing stricter penalties for unethical behavior. Independent oversight boards could play a crucial role in monitoring PBM activities and ensuring compliance with ethical standards and regulations. Furthermore, promoting a culture of ethical leadership within PBM organizations, where ethical considerations are prioritized over short-term profits, is paramount.
Finally, fostering collaboration between PBMs, pharmaceutical manufacturers, and healthcare providers can create a more transparent and accountable healthcare ecosystem. A proactive, preventative approach focusing on ethical corporate governance is essential to prevent similar scandals from occurring in the future.
Ultimate Conclusion
The accusations against these PBM executives are far from settled. The legal battles ahead will undoubtedly be long and complex, with high stakes for all involved. The outcome of this investigation will significantly influence public perception of PBMs and could lead to significant reforms within the industry. Regardless of the final verdict, this case serves as a stark reminder of the importance of accountability and transparency in the healthcare sector.
The potential for fines and jail time sends a powerful message: lying to Congress has serious consequences. This story is far from over, and we’ll be keeping a close eye on its development. The future of healthcare may well depend on it.
Common Queries
What are PBMs?
Pharmacy Benefit Managers (PBMs) are companies that manage prescription drug benefits for insurance companies and employers. They negotiate drug prices, process claims, and manage formularies.
What are the potential long-term effects of this investigation?
Depending on the outcome, this could lead to increased regulation of PBMs, greater transparency in drug pricing, and potentially lower prescription drug costs for consumers.
Could other PBM executives face similar charges?
This is certainly a possibility. The investigation may uncover further evidence of wrongdoing, leading to additional charges against other individuals within the PBM industry.
What is the timeline for the legal proceedings?
It’s difficult to predict an exact timeline, as legal proceedings can be lengthy and complex. However, we can expect updates as the case progresses through the courts.