Healthcare Cybersecurity Reporting CISA Changes
Healthcare cybersecurity reporting regulation cisa change heatlhcare – Healthcare cybersecurity reporting regulation CISA change healthcare – it’s a mouthful, isn’t it? But behind the jargon lies a crucial story impacting every hospital, clinic, and doctor’s office in the US. This post dives into the evolving landscape of healthcare cybersecurity reporting, focusing on the significant changes brought about by the Cybersecurity and Infrastructure Security Agency (CISA).
We’ll explore the complexities of HIPAA compliance, the vital role of CISA in bolstering healthcare security, and what these changes mean for the future of patient data protection.
We’ll unpack the recent CISA updates, analyze their impact on healthcare organizations, and offer practical steps to navigate this complex regulatory environment. From understanding reporting timelines to implementing effective incident response plans, we’ll cover the essential elements healthcare providers need to know to stay ahead of the curve. Get ready to navigate the intricacies of protecting sensitive patient data in the digital age!
Healthcare Cybersecurity Reporting Landscape
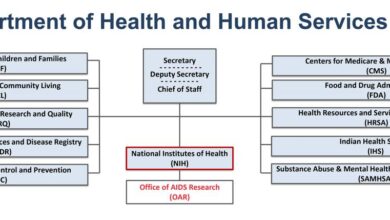
Navigating the complex web of healthcare cybersecurity regulations in the US can be challenging. Multiple laws and regulations overlap, each with its own reporting requirements and penalties for non-compliance. Understanding these nuances is crucial for healthcare providers to protect patient data and avoid significant legal and financial repercussions.The current state of healthcare cybersecurity reporting in the US is characterized by a multi-layered approach involving federal and, in some cases, state regulations.
HIPAA, while not solely focused on cybersecurity, forms the foundation, supplemented by other laws like the Health Information Technology for Economic and Clinical Health (HITECH) Act and state-specific breach notification laws. These regulations work together to establish a framework for data breach reporting, incident response, and overall security posture.
HIPAA vs. Other Regulations
HIPAA’s Privacy and Security Rules establish baseline requirements for protecting protected health information (PHI). While HIPAA doesn’t explicitly define specific cybersecurity breach reporting timelines, it mandates the implementation of reasonable and appropriate safeguards to protect PHI. The HITECH Act significantly strengthened HIPAA enforcement and broadened the scope of breach notification requirements. Other regulations, such as those enforced by the Cybersecurity and Infrastructure Security Agency (CISA), might focus on specific critical infrastructure sectors or vulnerabilities, often requiring more immediate reporting than HIPAA mandates for certain types of breaches.
State-level laws often impose additional requirements, creating a complex patchwork of regulations. For example, some states may require notification of breaches involving a smaller number of individuals than the federal threshold.
Reporting Requirements for Various Breach Types
The reporting requirements for healthcare data breaches vary depending on the type of data compromised and the number of individuals affected. Breaches involving PHI, such as medical records, billing information, or genetic data, typically require notification to affected individuals, the Department of Health and Human Services (HHS), and, in some cases, the media. Breaches involving less sensitive data might have different notification requirements.
The threshold for notification often varies depending on the specific regulation. For instance, HIPAA generally requires notification if the breach affects 500 or more individuals. However, some states have lower thresholds. The severity of the breach also influences reporting timelines and the level of detail required in the notification. A large-scale, sophisticated attack will require a more comprehensive and immediate response than a smaller, less impactful incident.
Key Regulations and Reporting Timelines
The following table summarizes key regulations and their reporting timelines. Note that these are general guidelines, and specific requirements can vary depending on the circumstances of the breach and applicable state laws.
| Regulation Name | Breach Type | Reporting Timeframe | Penalties |
|---|---|---|---|
| HIPAA (with HITECH Act) | Breach of PHI (500+ individuals) | 60 days from discovery | Significant fines, legal action |
| State Breach Notification Laws (vary by state) | Breach of PHI (thresholds vary) | Varies by state (often within 30-60 days) | Varies by state (fines, legal action) |
| CISA (for critical infrastructure) | Cybersecurity incidents impacting critical infrastructure | Immediately or within 24-72 hours (depending on severity) | Varies (fines, legal action, reputational damage) |
CISA’s Role in Healthcare Cybersecurity
The Cybersecurity and Infrastructure Security Agency (CISA) plays a crucial role in safeguarding the nation’s critical infrastructure, and healthcare is a significant component of that infrastructure. Given the increasing sophistication and frequency of cyberattacks targeting healthcare organizations, CISA’s involvement is paramount in bolstering the sector’s cybersecurity defenses. Their mandate extends beyond simply reacting to incidents; it encompasses proactive measures to prevent attacks and build a more resilient healthcare ecosystem.CISA’s responsibilities concerning healthcare cybersecurity are multifaceted.
They work to identify and mitigate cybersecurity risks, provide guidance and resources to healthcare providers, and collaborate with public and private sector partners to improve overall cybersecurity posture. This involves coordinating national-level responses to significant cyber incidents impacting healthcare, sharing threat intelligence, and promoting best practices for security awareness and incident response. They also play a vital role in coordinating information sharing and facilitating collaboration across the healthcare sector.
CISA Resources and Tools for Healthcare Organizations
CISA offers a wide array of resources and tools designed to help healthcare organizations improve their cybersecurity. These include publications offering best practices and guidance on various cybersecurity topics, such as vulnerability management, incident response planning, and security awareness training. They also provide access to threat intelligence feeds and vulnerability databases, allowing healthcare organizations to stay informed about emerging threats and proactively address potential vulnerabilities.
Furthermore, CISA offers numerous training programs and workshops tailored to the specific needs of the healthcare sector, equipping personnel with the necessary skills to effectively manage cybersecurity risks. These resources are readily available on the CISA website and are regularly updated to reflect the ever-evolving threat landscape.
CISA Initiatives for Enhancing Healthcare Cybersecurity Reporting and Incident Response
CISA actively participates in initiatives designed to streamline healthcare cybersecurity reporting and enhance incident response capabilities. For example, they work closely with the healthcare industry to improve the speed and effectiveness of reporting cybersecurity incidents, fostering a culture of proactive information sharing. This includes developing standardized reporting mechanisms and providing guidance on incident response best practices. CISA also works to facilitate collaboration between healthcare providers and other stakeholders, including law enforcement and other government agencies, to ensure coordinated and effective responses to significant cyber incidents.
These initiatives are crucial for minimizing the impact of cyberattacks on patient care and protecting sensitive patient data.
Examples of Successful CISA-Healthcare Provider Collaborations
CISA has a history of successful collaborations with healthcare providers in addressing cybersecurity threats. For example, following significant ransomware attacks targeting healthcare organizations, CISA has provided technical assistance and expertise to help affected organizations recover their systems and implement improved security measures. In several instances, CISA has facilitated information sharing among healthcare providers to help prevent similar attacks in the future.
These collaborations often involve joint exercises and training programs, which help to build stronger relationships and improve coordination in responding to cyber incidents. Through these partnerships, CISA plays a critical role in strengthening the collective cybersecurity posture of the healthcare sector, fostering a more resilient and secure healthcare ecosystem.
Impact of CISA Changes on Healthcare Cybersecurity Reporting
The Cybersecurity and Infrastructure Security Agency (CISA) plays a crucial role in safeguarding America’s critical infrastructure, and healthcare is a key component. Recent changes to CISA’s reporting requirements for healthcare cybersecurity incidents significantly alter the landscape for hospitals, clinics, and other healthcare providers. These changes aim to improve incident response and enhance the overall security posture of the healthcare sector, but they also present new challenges for compliance.CISA’s updated guidelines emphasize proactive threat detection and faster reporting of significant cybersecurity incidents.
This shift reflects a growing awareness of the devastating consequences of ransomware attacks and other cyber threats on patient care and healthcare operations. The agency’s focus has moved from simply reacting to breaches to actively preventing them and mitigating their impact. This proactive approach necessitates a more robust cybersecurity infrastructure and more stringent reporting protocols within healthcare organizations.
Failure to comply can result in significant penalties and reputational damage.
The recent changes to healthcare cybersecurity reporting regulations under CISA are forcing providers to seriously bolster their defenses. This comes at a time when healthcare spending is exploding, as highlighted by this insightful KFF report on Medicare GLP-1 spending and weight loss , a factor that could further strain already stretched budgets and potentially impact a provider’s ability to comply with the new security mandates.
Ultimately, improved cybersecurity and responsible spending are both crucial for the future of healthcare.
New Requirements and Implications for Data Breach Notification
The revised CISA regulations introduce more stringent criteria for mandatory reporting, expanding the types of incidents requiring immediate notification. This includes incidents that may not necessarily involve data breaches but pose a significant risk to patient safety or the continuity of healthcare services. The definition of a “significant” incident has broadened, requiring a more nuanced risk assessment by healthcare organizations.
For example, successful attacks on medical devices that could compromise patient care, even without data exfiltration, now fall under mandatory reporting. This change demands a more comprehensive understanding of the organization’s IT infrastructure and its vulnerabilities. The timeline for reporting has also been shortened, demanding quicker incident response and a more efficient reporting process. Delays in reporting can lead to severe penalties.
Steps for Healthcare Organizations to Adapt to New CISA Regulations, Healthcare cybersecurity reporting regulation cisa change heatlhcare
Adapting to the new CISA regulations requires a multi-faceted approach. Healthcare organizations must proactively strengthen their cybersecurity posture and establish robust incident response plans. This requires a commitment to ongoing training and investment in cybersecurity infrastructure and technology.
- Conduct a comprehensive vulnerability assessment: Identify and address weaknesses in your IT infrastructure and systems.
- Implement robust security controls: This includes multi-factor authentication, intrusion detection systems, and regular security audits.
- Develop and regularly test an incident response plan: This plan should Artikel clear procedures for detecting, containing, and responding to cybersecurity incidents. It should also include detailed protocols for communication and reporting to CISA.
- Invest in cybersecurity awareness training for staff: Educating employees about phishing scams, malware, and other cyber threats is crucial for preventing incidents.
- Establish a dedicated cybersecurity team: A dedicated team can effectively manage cybersecurity risks and respond to incidents.
- Regularly review and update your policies and procedures: Stay informed about the latest CISA guidelines and adapt your policies accordingly.
- Implement a system for tracking and reporting incidents: This will ensure timely and accurate reporting to CISA.
Challenges and Best Practices in Healthcare Cybersecurity Reporting
Navigating the complex landscape of healthcare cybersecurity reporting regulations presents significant hurdles for organizations of all sizes. The sheer volume of data, the sensitivity of patient information, and the evolving threat landscape all contribute to the difficulty of maintaining compliance and responding effectively to incidents. This section will explore some of the key challenges and Artikel best practices for effective reporting and incident response.
Major Challenges in Healthcare Cybersecurity Reporting Compliance
Healthcare organizations face numerous challenges in complying with cybersecurity reporting regulations. These challenges often stem from a combination of resource constraints, technological limitations, and the inherent complexity of healthcare data. For example, maintaining accurate and up-to-date inventory of all systems and devices across a sprawling network is a monumental task, crucial for effective vulnerability management and incident response.
Similarly, the lack of skilled cybersecurity personnel, especially in smaller healthcare facilities, exacerbates the problem. The constant evolution of cyber threats and attack vectors necessitates continuous adaptation and training, placing further strain on already stretched resources. Furthermore, the stringent regulatory requirements, such as HIPAA and the evolving CISA mandates, demand meticulous record-keeping and documentation, adding to the administrative burden.
Finally, integrating cybersecurity into existing workflows and culture can be challenging, requiring a significant shift in organizational mindset and prioritization.
Best Practices for Developing and Implementing Effective Cybersecurity Incident Response Plans
A well-defined and regularly tested incident response plan is paramount for mitigating the impact of a cybersecurity breach. This plan should Artikel clear roles and responsibilities, communication protocols, and escalation procedures. It’s crucial to establish a dedicated incident response team with members from various departments, including IT, legal, public relations, and clinical staff. Regular training and tabletop exercises are essential to ensure the team’s preparedness and familiarity with the plan.
The plan should also include a detailed process for identifying, containing, eradicating, recovering from, and learning from a security incident. The use of established frameworks like NIST Cybersecurity Framework can significantly enhance the structure and effectiveness of the plan, providing a standardized approach to incident management. Furthermore, the plan should be regularly reviewed and updated to reflect changes in technology, threats, and regulatory requirements.
A successful incident response plan will minimize the disruption caused by an attack and protect sensitive patient data.
Effective Communication of Cybersecurity Incidents to Stakeholders
Effective communication is critical during and after a cybersecurity incident. This includes promptly notifying affected patients, regulatory bodies (like HHS’ Office for Civil Rights and CISA), and other relevant stakeholders. Transparency and honesty are key to building trust and maintaining credibility. Communication should be clear, concise, and tailored to the specific audience. For patients, the communication should focus on the impact on their data, the steps taken to mitigate the risk, and the resources available to them.
For regulators, the communication should adhere to all reporting requirements and provide a detailed account of the incident, including root cause analysis and remedial actions. A well-crafted communication strategy can significantly reduce the negative impact of a breach and help maintain the organization’s reputation. This strategy should be pre-planned and tested as part of the overall incident response plan.
The changes to healthcare cybersecurity reporting under CISA are a huge deal, impacting everything from data breaches to operational resilience. The recent news about Steward Health Care, with its steward ohio hospitals closures pennsylvania facility at risk , highlights just how vulnerable even large systems can be. This underscores the urgency of these new regulations and the need for robust cybersecurity practices across the healthcare industry to prevent further disruptions.
Utilizing Incident Response Frameworks to Enhance Reporting Efficiency
Leveraging incident response frameworks, such as the NIST Cybersecurity Framework, can significantly improve the efficiency and effectiveness of cybersecurity reporting. These frameworks provide a structured approach to incident management, guiding organizations through the various stages of response, from identification and containment to recovery and post-incident activity. The NIST framework, for instance, provides a comprehensive set of guidelines and best practices that can be adapted to fit the specific needs of healthcare organizations.
By adopting a standardized framework, organizations can streamline their incident response processes, improve communication and collaboration, and ensure consistent reporting across different incidents. This standardized approach not only enhances efficiency but also facilitates better analysis of incidents and identification of recurring vulnerabilities, ultimately leading to improved overall cybersecurity posture. Furthermore, using a recognized framework can demonstrate due diligence to regulators, potentially mitigating penalties in the event of a breach.
Future Trends in Healthcare Cybersecurity Reporting
Source: ytimg.com
The healthcare cybersecurity landscape is in constant flux, driven by evolving threats and technological advancements. Predicting the future of reporting requires considering these dynamic forces and their interplay with regulatory mandates. The coming years will see a significant shift in how healthcare organizations approach and manage cybersecurity reporting, impacting everything from data breach notification to proactive risk management.
The Rise of Automated Reporting and Threat Intelligence Integration
Automated reporting systems will become increasingly prevalent, leveraging AI and machine learning to analyze vast amounts of security data, identify anomalies, and generate concise, actionable reports. This automation will reduce the manual burden on security teams, enabling quicker response times to incidents. Simultaneously, the integration of threat intelligence feeds will allow for a more proactive approach, enabling organizations to anticipate and mitigate emerging threats before they can cause significant damage.
For example, an AI-powered system could automatically detect a suspicious login attempt from an unusual geographic location and generate a report highlighting the potential breach, triggering automated mitigation steps like account lockout. This represents a significant improvement over current methods that rely heavily on manual detection and analysis.
Blockchain’s Role in Enhancing Data Integrity and Transparency
Blockchain technology offers the potential to enhance the security and transparency of cybersecurity reporting. By creating an immutable record of security events, blockchain can provide verifiable evidence of compliance with regulations and improve trust among stakeholders. Imagine a system where every security incident, from a phishing attempt to a data breach, is recorded on a shared, tamper-proof blockchain.
This would significantly improve the accuracy and reliability of reporting, reducing the potential for manipulation or misrepresentation. This is particularly relevant in situations requiring collaboration between multiple healthcare providers or sharing sensitive patient data.
The Impact of Increasingly Sophisticated Cyberattacks
The increasing sophistication of cyberattacks, including ransomware and advanced persistent threats (APTs), will necessitate more robust and detailed reporting processes. Healthcare organizations will need to invest in advanced security information and event management (SIEM) systems and threat intelligence platforms to capture and analyze the complex data generated by these attacks. The shift towards cloud-based services will also require adaptations in reporting methodologies to account for the distributed nature of data and systems.
The changing landscape of healthcare cybersecurity reporting, particularly with CISA’s updated regulations, has me thinking about resource allocation. News that Kaiser Permanente is nixing a $500 million Seattle bed tower, as reported by this article , highlights how financial pressures can impact even major healthcare systems. This makes the need for effective, cost-conscious cybersecurity strategies even more critical, ensuring compliance without sacrificing patient care.
For example, a sophisticated ransomware attack might involve multiple vectors and encrypted data across various systems. Comprehensive reporting in this scenario would necessitate a detailed timeline of events, impact assessment, and a thorough analysis of the attacker’s tactics, techniques, and procedures (TTPs).
Projected Evolution of Healthcare Cybersecurity Reporting (Visual Representation)
Imagine a graph charting the evolution of healthcare cybersecurity reporting over the next five years. The X-axis represents time (years), and the Y-axis represents the complexity and sophistication of reporting. The graph starts with a relatively flat line representing the current state, where reporting is largely manual and reactive. Over the next two years, the line begins to ascend more steeply, reflecting the increasing adoption of automated reporting and threat intelligence integration.
After year three, the line’s ascent accelerates further, driven by the integration of blockchain technology and the need to respond to increasingly complex attacks. By year five, the line plateaus at a significantly higher level, signifying a mature, proactive, and highly automated reporting ecosystem, capable of handling sophisticated threats and providing comprehensive insights into cybersecurity posture. This visualization depicts a transition from reactive, manual reporting to a proactive, automated, and highly secure system.
Final Conclusion: Healthcare Cybersecurity Reporting Regulation Cisa Change Heatlhcare

Source: industrialcyber.co
Navigating the world of healthcare cybersecurity reporting can feel like a daunting task, but understanding the role of CISA and the implications of recent regulatory changes is critical. By proactively adapting to these evolving requirements and embracing best practices, healthcare organizations can significantly enhance their cybersecurity posture and protect the sensitive data entrusted to their care. The future of healthcare cybersecurity relies on collaboration, continuous improvement, and a commitment to safeguarding patient information.
Let’s work together to build a more secure and resilient healthcare system.
FAQ Insights
What are the penalties for non-compliance with healthcare cybersecurity reporting regulations?
Penalties vary depending on the regulation and the severity of the breach. They can range from significant financial fines to legal action and reputational damage.
How often should healthcare organizations review and update their cybersecurity incident response plans?
Regular reviews, at least annually, and updates should be conducted whenever there are significant changes in technology, regulations, or the threat landscape.
What resources does CISA offer to help healthcare organizations improve their cybersecurity?
CISA provides numerous resources, including threat intelligence, vulnerability assessments, and training materials, to assist healthcare organizations in strengthening their cybersecurity defenses.
Can small healthcare providers afford to comply with all these regulations?
While compliance can be challenging, many resources and collaborative efforts exist to help smaller providers meet these requirements. CISA offers support, and industry groups often provide guidance and assistance.