How Does Maida Harm Your Gut and Health?
How does maida a glue for gut harms your gut and health – How does maida, a glue for gut, harm your gut and health? It’s a question that deserves a closer look, especially given how prevalent this refined flour is in our diets. We often hear about the benefits of whole grains, but what about the flip side? This post dives into the science behind maida’s impact on digestion, inflammation, and overall well-being, exploring why choosing alternatives might be a game-changer for your gut health.
Maida, or refined wheat flour, undergoes a process that strips away the bran and germ, leaving only the endosperm. This process, while making the flour easier to work with, significantly reduces its nutritional value. The lack of fiber, crucial for gut health, is a primary concern. We’ll explore how this deficiency disrupts the delicate balance of your gut microbiome, potentially leading to digestive issues, inflammation, and even long-term health problems like type 2 diabetes and cardiovascular disease.
We’ll also uncover healthier alternatives and how incorporating them into your diet can make a positive difference.
Maida’s Composition and Gut Microbiome Interaction

Source: ytimg.com
Maida, or refined wheat flour, undergoes extensive processing that removes the bran and germ, leaving primarily the endosperm. This process significantly alters its nutritional profile and impacts its interaction with the gut microbiome, the complex community of microorganisms residing in our intestines. Understanding this interaction is crucial for assessing the potential health consequences of a diet high in maida-based foods.Maida’s chemical composition lacks the fiber, vitamins, and minerals present in whole wheat flour.
This refined nature contributes to its digestibility but also to its potential negative effects on gut health. The absence of fiber, in particular, is a key factor impacting the gut microbiome.
Maida’s Impact on Gut Microbiome Diversity
The lack of fiber in maida limits the growth of beneficial gut bacteria that thrive on fiber fermentation. These beneficial bacteria, such as
- Bifidobacteria* and
- Lactobacilli*, play vital roles in maintaining gut health, including boosting immunity and producing short-chain fatty acids (SCFAs) that nourish the gut lining. Conversely, a diet rich in maida may promote the growth of certain harmful bacteria, potentially leading to an imbalance in the gut microbiome, known as dysbiosis. This dysbiosis is linked to various health problems, including inflammation, irritable bowel syndrome (IBS), and even increased risk of chronic diseases.
For instance, studies have shown a correlation between high maida consumption and increased prevalence of gut dysbiosis in individuals with metabolic syndrome.
Digestive Process Comparison: Maida vs. Whole Grains
Digesting maida-based foods is a relatively quick process due to the absence of fiber. This rapid digestion leads to a rapid spike in blood sugar levels, potentially contributing to insulin resistance and weight gain. In contrast, whole grains, rich in fiber, are digested more slowly. This slower digestion results in a more gradual release of glucose into the bloodstream, preventing blood sugar spikes and promoting satiety.
The fiber in whole grains also acts as prebiotics, feeding the beneficial bacteria in the gut and promoting a healthy microbiome. A typical example is comparing the digestive response to a white bread roll (maida-based) versus a whole-wheat roll. The latter provides sustained energy and promotes gut health due to its fiber content.
Maida’s Potential Disruption of the Gut Barrier
The gut barrier, a single layer of cells lining the intestines, is crucial for maintaining the separation between the gut contents and the bloodstream. A compromised gut barrier, also known as increased intestinal permeability or “leaky gut,” can allow harmful substances, such as toxins and undigested food particles, to enter the bloodstream, triggering inflammation and contributing to various health issues.
While direct evidence linking maida consumption to a significant disruption of the gut barrier is limited, the lack of fiber in maida and the potential for dysbiosis it promotes may indirectly contribute to gut barrier dysfunction. This is because a healthy gut microbiome plays a critical role in maintaining the integrity of the gut barrier. A disrupted microbiome, as may occur with high maida consumption, could weaken the gut barrier, potentially leading to increased intestinal permeability.
Further research is needed to fully elucidate the precise mechanisms involved.
Maida’s Impact on Digestion and Nutrient Absorption
Maida, the refined flour stripped of its bran and germ, significantly alters the digestive process and impacts nutrient absorption. Unlike whole grains, its processed nature leads to several negative consequences for our gut health and overall well-being. Understanding these effects is crucial for making informed dietary choices.Maida’s impact on digestion primarily stems from its lack of fiber and high glycemic index.
The absence of fiber means less bulk in the digestive tract, resulting in slower transit time. This slower movement allows for increased fermentation of the remaining carbohydrates by gut bacteria, potentially leading to discomfort, bloating, and gas. The high glycemic index, on the other hand, causes a rapid spike in blood sugar, followed by a subsequent crash, further disrupting digestive balance and contributing to energy fluctuations.
Digestive Issues Associated with High Maida Consumption
The reduced fiber content and rapid digestion of maida are directly linked to several common digestive problems. Individuals who consume a diet high in maida often experience symptoms like constipation due to the lack of bulk promoting regular bowel movements. Bloating and gas are also prevalent due to the increased fermentation of the refined carbohydrates in the gut.
Furthermore, some individuals may experience diarrhea or abdominal discomfort due to the rapid digestion and potential irritation of the gut lining. These symptoms collectively highlight the negative impact of maida on the digestive system.
Impact of Maida on Nutrient Absorption
Maida’s low fiber content significantly impairs the absorption of essential nutrients. Fiber acts as a prebiotic, feeding beneficial gut bacteria that aid in nutrient extraction. Without sufficient fiber, the gut microbiome is negatively affected, hindering the efficient breakdown and uptake of several vital nutrients. This is particularly true for vitamins and minerals which are often found in higher concentrations in the bran and germ of the grain, components removed during maida processing.
Specific Nutrients Affected by Maida Consumption
The absorption of several key nutrients can be compromised by a diet high in maida. For example, B vitamins, crucial for energy production and nerve function, are less readily absorbed when fiber intake is low. Similarly, the absorption of minerals like iron and magnesium, essential for red blood cell production and bone health, can be negatively impacted. The lack of fiber also affects the absorption of certain antioxidants and phytochemicals, which contribute to overall health and disease prevention.
A diet rich in whole grains, in contrast to one heavily reliant on maida, promotes a healthier gut environment and better nutrient assimilation.
Maida and Inflammatory Responses in the Gut
Maida, a refined flour stripped of its bran and germ, has been increasingly linked to chronic inflammation in the gut. This inflammatory response isn’t a direct, immediate effect but rather a consequence of several factors related to its composition and impact on the digestive system. Understanding this connection is crucial for appreciating the potential long-term health implications of a diet high in maida-based products.The refined nature of maida is a key player in its inflammatory potential.
The removal of fiber during processing significantly alters its impact on the gut microbiome. Fiber acts as prebiotic, feeding beneficial bacteria and promoting a balanced gut environment. Maida’s lack of fiber disrupts this balance, potentially leading to an overgrowth of harmful bacteria and a subsequent inflammatory response. Furthermore, maida’s high glycemic index (GI) causes rapid spikes in blood sugar levels.
These fluctuations trigger inflammation throughout the body, including the gut. This process is further exacerbated by the presence of antinutrients in some maida products, which can interfere with nutrient absorption and contribute to gut irritation.
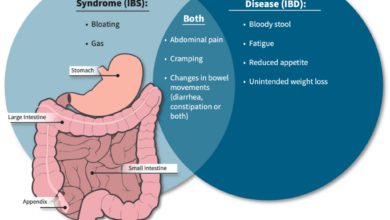
Maida’s Contribution to Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a chronic gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. While the exact cause of IBS remains unclear, there’s growing evidence suggesting a link between a diet high in refined carbohydrates, such as maida, and the development or exacerbation of IBS symptoms. The lack of fiber in maida contributes to irregular bowel movements and constipation, a common symptom of IBS.
The resulting gut dysbiosis (imbalance in gut microbiota) and increased intestinal permeability further fuel inflammation, potentially triggering or worsening IBS symptoms. Studies have shown that individuals with IBS often experience improvements in their symptoms when they adopt a diet rich in fiber and low in refined carbohydrates.
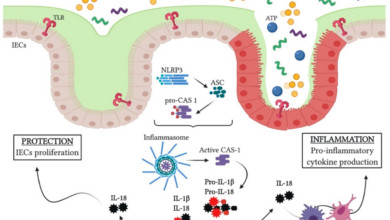
Inflammatory Pathways Triggered by Maida Consumption
Maida consumption can trigger several inflammatory pathways in the gut. The rapid rise in blood sugar levels following maida consumption stimulates the production of pro-inflammatory cytokines, such as TNF-α and IL-6. These cytokines promote inflammation and can damage the intestinal lining, increasing gut permeability. Increased gut permeability, or “leaky gut,” allows undigested food particles and toxins to enter the bloodstream, triggering a systemic inflammatory response.
Additionally, the lack of fiber in maida can lead to alterations in the gut microbiota composition, favoring the growth of harmful bacteria that produce pro-inflammatory substances. This dysbiosis further exacerbates the inflammatory response in the gut. The combination of these factors contributes to a chronic inflammatory state, increasing the risk of various health problems.
Comparison of Inflammatory Responses
| Food Type | Inflammatory Markers | Gut Permeability | Associated Symptoms |
|---|---|---|---|
| Maida | Increased TNF-α, IL-6, other pro-inflammatory cytokines | Increased; “Leaky gut” | Bloating, abdominal pain, diarrhea or constipation, fatigue, IBS symptoms |
| Whole Grains | Reduced levels of pro-inflammatory cytokines | Improved; reduced permeability | Improved digestion, regular bowel movements, reduced inflammation |
Maida and Overall Health Implications

Source: imimg.com
Maida, due to its refined nature and lack of fiber, poses significant challenges to overall health beyond just gut issues. Its impact extends to weight management, blood sugar control, and cardiovascular health, highlighting the importance of mindful consumption. Let’s delve into the specific ways maida consumption can negatively affect your well-being.
Maida and Weight Management Challenges, How does maida a glue for gut harms your gut and health
The high glycemic index (GI) of maida contributes significantly to weight gain. Maida is rapidly digested and absorbed, leading to a quick spike in blood sugar levels. This surge triggers an insulin response, promoting fat storage. The lack of fiber in maida also means it doesn’t provide the satiety that fiber-rich foods offer, leading to increased calorie intake.
For example, a diet rich in maida-based products like bread and pastries often leaves individuals feeling hungry sooner, prompting them to consume more throughout the day, ultimately contributing to a calorie surplus and weight gain. This is particularly problematic for individuals already struggling with weight management.
Maida and the Risk of Type 2 Diabetes
The rapid rise in blood sugar levels after consuming maida-rich foods contributes directly to insulin resistance, a hallmark of type 2 diabetes. Consistent consumption of maida can lead to the pancreas working harder to produce insulin, eventually becoming less efficient. This chronic state of elevated blood sugar increases the risk of developing type 2 diabetes. Studies have consistently shown a correlation between high maida consumption and an increased incidence of this metabolic disorder.
For instance, populations with diets heavily reliant on maida-based staples have shown higher rates of type 2 diabetes compared to populations with diets richer in whole grains.
Maida and Cardiovascular Health Issues
High maida intake is associated with increased levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. This increase in LDL cholesterol, coupled with the potential for elevated blood sugar and insulin resistance, significantly raises the risk of developing cardiovascular diseases like heart disease and stroke. The lack of fiber in maida also means it doesn’t contribute to lowering cholesterol levels, unlike fiber-rich whole grains.
Furthermore, maida’s impact on inflammation, as discussed earlier, also plays a role in the development of atherosclerosis, a key factor in cardiovascular disease.
Potential Long-Term Health Problems Associated with High Maida Intake
High and consistent consumption of maida can contribute to a range of long-term health problems. It’s crucial to remember that these risks are amplified when combined with other unhealthy lifestyle choices.
A list of potential long-term health consequences includes:
- Obesity
- Type 2 diabetes
- Cardiovascular diseases (heart disease, stroke)
- Increased risk of certain cancers
- Digestive problems (constipation, bloating)
- Nutrient deficiencies
Alternatives to Maida and their Gut Health Benefits: How Does Maida A Glue For Gut Harms Your Gut And Health
Maida, while convenient, significantly lacks the nutritional value and fiber content crucial for a healthy gut. Fortunately, numerous flour alternatives offer substantial benefits for digestion and overall well-being. Switching to these options can positively impact your gut microbiome and contribute to a healthier lifestyle.
Let’s explore some healthier alternatives to maida and delve into their nutritional profiles and gut-health benefits.
Nutritional Comparison of Maida and Alternative Flours
Maida, being refined flour, is stripped of its bran and germ, resulting in a low fiber and high glycemic index product. In contrast, whole wheat flour, oat flour, and barley flour retain the bran and germ, providing a richer source of fiber, vitamins, minerals, and antioxidants. This table visually represents the differences:
Imagine a bar chart with four bars representing Maida, Whole Wheat, Oats, and Barley. The chart has two axes: the vertical axis represents the quantity (e.g., grams per 100g of flour), and the horizontal axis represents the four types of flour. The first set of bars shows fiber content. Maida’s bar is very short, indicating low fiber. Whole wheat’s bar is significantly taller, showing much higher fiber content.
Oat flour and barley flour bars are also tall, with oat flour possibly slightly taller than barley. The second set of bars, positioned alongside the first, shows the glycemic index. Maida’s bar is very tall, reflecting its high glycemic index. The bars for whole wheat, oats, and barley are much shorter, demonstrating their lower glycemic index. The visual difference clearly highlights the nutritional disparities.
Positive Effects of Alternative Flours on Gut Health
The increased fiber content in whole wheat, oat, and barley flour significantly benefits gut health. Fiber acts as prebiotic, feeding beneficial gut bacteria. This promotes a balanced gut microbiome, crucial for optimal digestion, nutrient absorption, and immune function. The higher fiber content also contributes to improved bowel regularity and reduced risk of constipation. Furthermore, the lower glycemic index of these flours leads to more stable blood sugar levels, preventing the spikes and crashes associated with maida consumption, which can negatively impact gut inflammation.
Recipes Utilizing Healthier Flour Alternatives
Whole wheat flour can easily replace maida in many recipes, such as roti, chapatis, and even cakes (though adjustments to liquid might be necessary). Oat flour is excellent for baking muffins, cookies, and pancakes, offering a naturally moist and slightly sweet texture. Barley flour can be used to make hearty breads and crackers. For example, a simple recipe swap could involve using whole wheat flour instead of maida in making pancakes, significantly increasing the fiber content and nutritional value.
Similarly, substituting oat flour for maida in muffins adds a subtle sweetness and increases fiber.
Wrap-Up

Source: possible.in
So, is maida the enemy of your gut? The evidence suggests it might be. While a small amount occasionally might not cause significant harm, consistently consuming maida-rich foods can negatively impact your digestive system and overall health. By understanding the science behind its negative effects, we can make informed choices about our diets. Switching to whole grains and exploring alternative flours offers a simple yet powerful way to nourish your gut and improve your well-being.
Remember, a healthy gut is a happy gut, and that starts with the food we choose!
Questions and Answers
What are the best alternatives to maida?
Whole wheat flour, oat flour, barley flour, and even almond flour are excellent alternatives, offering more fiber and nutrients.
Can I still eat foods with maida occasionally?
Occasional consumption is likely fine for most people, but prioritizing whole-grain options is key for long-term gut health.
How quickly will I see improvements after switching to healthier flours?
Results vary, but many people experience improvements in digestion and energy levels within a few weeks.
Are there any specific symptoms that indicate maida sensitivity?
Bloating, gas, constipation, diarrhea, and abdominal pain are common symptoms of maida sensitivity. If you experience these regularly, consider eliminating maida from your diet for a trial period.