Samsung Bwell Health Record Appointment Scheduling
Samsung Bwell health record appointment scheduling is revolutionizing how we manage our healthcare! This app aims to streamline the often-frustrating process of booking doctor’s appointments and accessing medical records. But does it live up to the hype? We’ll dive into the features, user experience, security, and future potential of this increasingly popular health management tool, exploring its strengths and weaknesses, and comparing it to other leading health apps.
From its intuitive interface to its integration with various healthcare providers, we’ll uncover the details behind Samsung Bwell’s appointment scheduling system. We’ll also examine user feedback, addressing common concerns and exploring potential improvements. Ultimately, we’ll assess whether Samsung Bwell truly simplifies healthcare access or if there’s room for significant enhancement.
Samsung Bwell App Functionality
Samsung Bwell is Samsung’s health and wellness app, aiming to provide a centralized platform for managing various aspects of your health. While it integrates with Samsung devices seamlessly, its functionality extends beyond simple fitness tracking. A key feature is its ability to access and manage health records, and, importantly, schedule appointments with healthcare providers. This blog post will delve into the specifics of these features.
Scheduling appointments via Samsung Bwell’s health record system is usually pretty straightforward, but recent news makes me think about the healthcare system’s complexities. I read that a deal was finally reached to end the New York nurse strike at Mount Sinai and Montefiore, as reported here. This highlights how crucial access to timely appointments is, and how smoothly functioning systems like Samsung Bwell can help navigate those potentially stressful situations.
Health Record Access and Management
The app allows users to securely store and access their health records, including lab results, medical history, and medication lists. This centralized location simplifies the process of sharing information with doctors or specialists, eliminating the need to carry physical copies or remember numerous details. The user interface presents this information in a clear, easily navigable format, using color-coding and intuitive icons to improve usability.
For example, recent lab results are prominently displayed, while older records are easily accessible through a chronological view or by search functionality. Users can also add manual entries, such as notes from doctor visits or personal health goals. Data security is a paramount concern, and the app employs robust encryption methods to protect sensitive user information.
Appointment Scheduling Functionality
Scheduling appointments within the Samsung Bwell app is generally straightforward. Users can search for providers based on specialty, location, and availability. Once a provider is selected, the app presents a calendar view of their available appointment slots, allowing for easy selection. The process is largely automated, with reminders sent via push notifications to ensure users don’t miss their appointments.
The UI is designed to minimize the number of steps required to book an appointment, focusing on clarity and efficiency. The appointment details, including date, time, and provider information, are clearly displayed and easily accessible for review or modification.
Comparison to Other Health Apps
The appointment scheduling feature in Samsung Bwell compares favorably to other popular health apps, but with some nuances. While apps like Apple Health and Google Fit excel in fitness tracking and data aggregation, their appointment scheduling capabilities are often limited or integrated through third-party apps. Samsung Bwell’s integration of health records and appointment scheduling within a single platform offers a more streamlined experience for users.
However, the availability of providers and appointment scheduling options within Bwell may depend on geographical location and the level of integration with local healthcare providers. The depth of health record integration also varies, with Bwell potentially offering a more comprehensive view for users within the Samsung ecosystem.
Feature Comparison Table
| App Name | Appointment Scheduling | Health Record Access | User Reviews (General Sentiment) |
|---|---|---|---|
| Samsung Bwell | Integrated, provider dependent | Good integration with Samsung devices; varies by region | Mixed; praised for integration, criticized for limited provider availability in some areas |
| Apple Health | Limited; often relies on third-party apps | Strong integration with Apple devices; focuses on fitness data | Generally positive; praised for ease of use and data privacy |
| Google Fit | Limited; relies on third-party apps or manual entry | Focuses on fitness and activity data; limited health record access | Generally positive; praised for comprehensive fitness tracking |
Integration with Healthcare Providers

Source: samsung.com
Samsung Bwell’s success hinges on its ability to seamlessly integrate with existing healthcare systems. Effective integration ensures a smooth patient experience and allows for the efficient exchange of crucial health information. This involves both technical considerations and strategic partnerships with various healthcare providers.The integration process is complex, requiring careful consideration of data security, interoperability standards, and the specific functionalities offered by different healthcare providers and their Electronic Health Record (EHR) systems.
A robust integration strategy is crucial for a user-friendly and reliable appointment scheduling experience.
Currently Integrated Healthcare Providers and Systems
Currently, Samsung Bwell’s specific list of integrated healthcare providers and systems is not publicly available. This information is often considered proprietary and subject to non-disclosure agreements. However, we can speculate on the types of providers likely to be integrated. These would include large hospital networks, individual clinics specializing in various medical fields (cardiology, dermatology, etc.), and potentially telehealth platforms.
The integration likely focuses on systems adhering to common interoperability standards like HL7 FHIR to facilitate data exchange.
Technical Aspects of the Integration Process
The technical integration of Samsung Bwell with healthcare providers’ systems typically involves Application Programming Interfaces (APIs). These APIs act as intermediaries, allowing Samsung Bwell to securely request and receive information from the provider’s EHR system. The process often involves authentication and authorization protocols to ensure data security and privacy compliance (e.g., HIPAA in the US). Data exchanged through these APIs could include patient demographics, appointment availability, appointment scheduling details, and potentially even limited medical history relevant to the appointment type.
The integration might leverage cloud-based services for secure data transmission and storage. Specific technical details, such as the types of APIs used (REST, SOAP, etc.) and the chosen data exchange formats (XML, JSON), are generally not publicly disclosed due to security and competitive reasons.
Challenges in Integrating with Different EHR Systems
Integrating with diverse EHR systems presents significant challenges. Different systems employ varying data formats, APIs, and security protocols. This lack of standardization necessitates custom integrations for each system, increasing development time and costs. Furthermore, ensuring data integrity and security across different systems requires rigorous testing and ongoing maintenance. Legacy systems, often lacking modern APIs, pose an additional hurdle, potentially requiring extensive workarounds or data transformations.
Differences in data models and terminologies also complicate the process, requiring careful mapping between the data structures used by Samsung Bwell and those employed by each healthcare provider. Finally, compliance with various healthcare regulations and data privacy laws (such as HIPAA) adds another layer of complexity to the integration process.
Data Flow During Appointment Scheduling
The following illustrates the data flow between Samsung Bwell and a healthcare provider’s system during appointment scheduling:[Diagram description: A flowchart depicting the data flow. The flowchart starts with the user on the Samsung Bwell app initiating an appointment request, specifying the provider and desired time slot. This request is then sent via an API to the healthcare provider’s EHR system.
The EHR system checks availability, and if available, sends a confirmation back to Samsung Bwell. Samsung Bwell then updates the user’s calendar with the confirmed appointment. If the time slot is unavailable, a rejection message is sent back to Samsung Bwell, which informs the user. The entire process highlights the secure transfer of data using encrypted channels and adherence to relevant privacy standards.]
User Experience and Feedback
Source: samsung.com
The Samsung Bwell app’s appointment scheduling feature, while aiming for seamless integration into users’ healthcare routines, has received a mixed bag of reviews. Understanding user experiences, both positive and negative, is crucial for optimizing the app and improving user satisfaction. This analysis delves into user feedback to identify areas for improvement and suggest concrete solutions.
Analyzing user reviews reveals a spectrum of experiences. While many praise the convenience and ease of scheduling appointments directly through the app, eliminating the need for phone calls or website navigation, others express frustration with various aspects of the system.
Positive User Reviews and Experiences
Positive feedback frequently highlights the app’s intuitive interface and the time-saving benefits. Users appreciate the ability to view available appointment slots, select their preferred time, and receive confirmation all within the app. Comments such as “So much easier than calling the doctor’s office!” and “Love the clear calendar view” are common. The integration with existing Samsung devices and health data also receives positive mention, creating a holistic health management experience for many users.
Negative User Reviews and Common Issues, Samsung bwell health record appointment scheduling
Conversely, negative reviews often center around specific issues. A significant number of complaints relate to limited provider availability within the app. Users in rural areas or those with less common specialists report difficulty finding appointments. Another recurring theme is technical glitches, including instances of scheduling failures, incorrect date/time displays, and notification issues. Some users also express concern about data privacy and security, despite Samsung’s stated commitment to these areas.
Finally, the lack of robust support features, such as a readily available help center or in-app chat support, frustrates many users who encounter problems.
Scheduling appointments through Samsung Bwell’s health record system is usually pretty straightforward, but I wonder how staffing shortages are impacting wait times. I read this article about healthcare executives highlighting talent acquisition and labor shortages as a major business risk, healthcare executives say talent acquisition labor shortages business risk , and it made me think about how that could translate to longer wait times for appointments, even with a convenient system like Samsung Bwell.
Hopefully, they’re finding ways to manage the workload effectively.
Suggestions for Improving User Experience
Based on the collected feedback, several improvements could significantly enhance the user experience. Addressing the limitations in provider availability requires strategic partnerships with a wider range of healthcare providers, especially in underserved areas. Investing in rigorous testing and quality assurance to minimize technical glitches is paramount. Clear, concise error messages should replace generic error prompts to assist users in troubleshooting.
Implementing a comprehensive FAQ section and providing multiple support channels, such as email and phone support, alongside in-app assistance, can effectively address user concerns and improve problem resolution. Furthermore, proactively addressing data privacy and security concerns through transparent communication and robust security measures can build user trust.
Five Key Improvements Based on User Feedback
To directly address user concerns and improve the appointment scheduling feature, the following improvements are suggested:
- Expand the network of participating healthcare providers to include a wider range of specialties and geographic locations.
- Implement a more robust system for appointment reminders and notifications, including customizable options and multiple notification methods (e.g., push notifications, SMS).
- Enhance error handling and provide clear, user-friendly error messages that guide users towards resolving issues.
- Develop a comprehensive FAQ section within the app and provide multiple support channels (e.g., email, phone, in-app chat) for user assistance.
- Strengthen data privacy and security measures, and clearly communicate these measures to users to build trust and transparency.
Security and Privacy
Protecting your health information is paramount, and Samsung Bwell takes this responsibility very seriously. We understand the sensitive nature of health data and have implemented robust security measures to safeguard your privacy throughout the appointment scheduling process. This commitment extends to our comprehensive privacy policies, which clearly Artikel how your data is collected, used, and protected.Samsung Bwell employs a multi-layered approach to security, ensuring your data remains confidential and secure.
This involves a combination of technical safeguards, stringent data governance policies, and adherence to industry best practices. We are continuously evaluating and improving our security protocols to stay ahead of evolving threats.
Data Encryption and Secure Transmission
All data transmitted between the Samsung Bwell app and our servers is encrypted using industry-standard encryption protocols, such as TLS (Transport Layer Security). This ensures that your personal and health information remains confidential during transmission and cannot be intercepted by unauthorized individuals. Data at rest, meaning data stored on our servers, is also encrypted using advanced encryption algorithms to protect against unauthorized access even if a breach were to occur.
For example, patient Personally Identifiable Information (PII) like names, addresses, and medical history are encrypted both in transit and at rest.
Privacy Policy Compliance
Samsung Bwell’s privacy policy adheres to all relevant data protection regulations, including HIPAA (Health Insurance Portability and Accountability Act) in the US and GDPR (General Data Protection Regulation) in Europe. Our policy clearly Artikels what data we collect, why we collect it, how we use it, and with whom we may share it (if applicable, such as with your healthcare provider).
We only collect the minimum necessary data required for appointment scheduling and related functionalities. Users have the right to access, correct, or delete their data at any time. Transparency and user control are central to our privacy practices.
Comparison with Industry Best Practices
Samsung Bwell’s security protocols are aligned with, and in many cases exceed, industry best practices for healthcare applications. We regularly benchmark our security measures against leading healthcare apps and undergo independent security audits to identify and address any vulnerabilities. We employ robust access control mechanisms, regular security updates, and intrusion detection systems to protect against unauthorized access, malware, and other threats.
Our commitment to security is ongoing and proactive, reflecting the dynamic nature of cybersecurity threats.
User Data Security Throughout Appointment Scheduling
The entire appointment scheduling process within Samsung Bwell is designed with security in mind. From the initial login, which may utilize multi-factor authentication, to the final confirmation of the appointment, data is encrypted and protected. We use secure APIs (Application Programming Interfaces) to communicate with healthcare provider systems, ensuring that data remains protected even during inter-system transfers. Regular security assessments and penetration testing are conducted to identify and mitigate potential weaknesses in the system.
Our commitment to user privacy and data security is a cornerstone of the Samsung Bwell platform.
Future Development and Improvements
The Samsung Bwell appointment scheduling function, while already a valuable tool, possesses significant potential for enhancement. Future development should focus on leveraging emerging technologies to create a more intuitive, efficient, and personalized user experience, ultimately improving patient engagement and healthcare outcomes. This involves exploring opportunities in machine learning, wearable device integration, and UI/UX refinements.
Machine Learning for Optimized Scheduling
Incorporating machine learning algorithms can dramatically improve appointment scheduling efficiency. For instance, a predictive model could analyze historical appointment data, including patient preferences, doctor availability, and appointment durations, to proactively suggest optimal scheduling times, minimizing wait times and maximizing clinic utilization. This could also include predicting potential scheduling conflicts and automatically suggesting alternative times. Real-world examples of this are already seen in other industries, such as ride-sharing services, which use machine learning to predict demand and optimize driver allocation.
In healthcare, this could translate to reduced patient frustration and improved resource management.
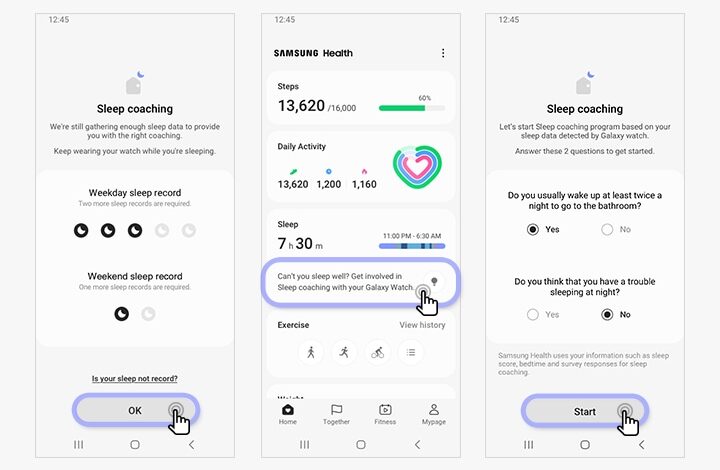
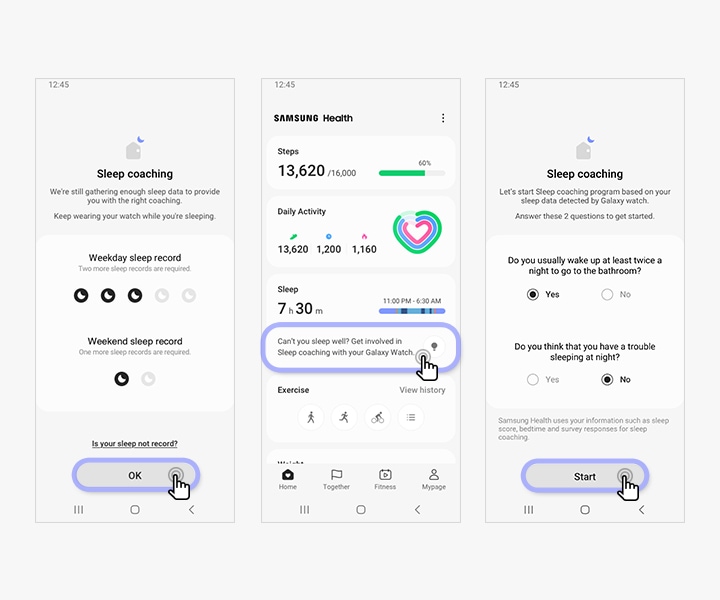
Wearable Device Integration for Enhanced Reminders and Health Data Tracking
Seamless integration with Samsung’s wearable devices, such as Galaxy Watches and smart fitness trackers, could revolutionize appointment reminders and health data tracking. Users could receive timely reminders directly on their wrist, reducing the risk of missed appointments. Furthermore, relevant health data, such as heart rate or sleep patterns, could be automatically pre-populated in the appointment scheduling process, providing valuable context for healthcare providers.
Imagine a scenario where a patient’s consistently elevated heart rate, as tracked by their wearable, is automatically flagged, prompting the system to schedule a follow-up appointment or alert the physician. This proactive approach could lead to earlier diagnosis and intervention.
Improved Appointment Scheduling User Interface
The ideal user interface for improved appointment scheduling in Samsung Bwell would prioritize simplicity and clarity. Imagine a clean, uncluttered screen with a prominent calendar view displaying available appointment slots for chosen providers. A color-coded system could clearly differentiate between different appointment types (e.g., routine check-up, specialist consultation) and highlight any scheduling conflicts. Users should have intuitive options to filter appointments by date, time, provider, and appointment type.
A simple, one-tap option to reschedule or cancel appointments should be readily available. The overall aesthetic should align with the modern and minimalist design language of other Samsung apps, maintaining consistency across the user’s ecosystem. A clear visual representation of the provider’s profile, including their photo, specialty, and contact information, should also be prominently displayed.
Scheduling appointments with Samsung Bwell’s health record system can be a breeze, but imagine a future where AI streamlines the process even further. This is where innovations like those discussed in this article on google cloud healthcare amy waldron generative AI become relevant. Such advancements could easily integrate with Samsung Bwell, potentially automating appointment reminders and even predicting optimal scheduling times based on individual patient needs.
It’s exciting to think about how this could improve healthcare access.
Final Wrap-Up
Managing your health shouldn’t be a headache, and Samsung Bwell aims to make it easier. While the app offers convenient appointment scheduling and health record access, its success hinges on continued improvements based on user feedback and advancements in integration with healthcare providers. Addressing security concerns and enhancing the user experience will be crucial for Samsung Bwell to solidify its position as a leading player in the health app market.
The future looks bright for apps like this, offering the potential to significantly simplify healthcare navigation, but only time will tell if it truly delivers on its promise.
FAQ: Samsung Bwell Health Record Appointment Scheduling
Can I use Samsung Bwell if I don’t have a Samsung phone?
No, Samsung Bwell is currently exclusive to Samsung devices.
What happens if my doctor’s office isn’t integrated with Samsung Bwell?
You won’t be able to schedule appointments directly through the app with that provider. You’ll have to use their traditional scheduling methods.
Is my data safe on Samsung Bwell?
Samsung employs various security measures to protect user data, but it’s crucial to review their privacy policy for specifics and understand the risks involved with storing sensitive health information digitally.
How do I cancel an appointment scheduled through Samsung Bwell?
The cancellation process varies depending on your provider. Check the app for specific instructions or contact your provider directly.





