Prior Authorization Blocks Necessary Care AMAs Stand
Prior authorization stands in way medically necessary care american medical association – Prior Authorization Blocks Necessary Care: AMA’s Stand. That’s the blunt truth facing countless Americans. This seemingly bureaucratic process – requiring pre-approval for medical treatments – is increasingly delaying, and even denying, essential care. We’re talking about life-altering treatments, procedures that are medically necessary, caught in a frustrating web of paperwork and insurance company red tape. The American Medical Association (AMA) has been vocal in its opposition, highlighting the significant negative impacts on both patients and healthcare providers.
This post delves into the frustrating reality of prior authorization, exploring its consequences and the ongoing fight for reform.
The current system places an immense burden on doctors and their staff, diverting precious time and resources away from patient care. Imagine a doctor spending hours battling insurance companies instead of focusing on their patients’ needs. The financial consequences for patients are equally staggering, leading to delayed treatments, mounting medical bills, and, in some cases, irreversible health damage. We’ll examine real-world examples, explore the AMA’s proposed solutions, and discuss potential technological advancements that could streamline this broken process.
The Impact of Prior Authorization on Access to Care

Source: smartbusinessgreatmedicine.com
Prior authorization, a process requiring pre-approval from insurance companies before receiving certain medical services, has become a significant barrier to timely and necessary healthcare. This seemingly simple administrative step introduces delays, increases administrative burdens on providers, and ultimately impacts patients’ access to crucial care. The consequences ripple through the entire healthcare system, affecting patient outcomes and the overall efficiency of medical practices.
The Prior Authorization Process and Delays
The prior authorization process typically involves healthcare providers submitting detailed requests to insurance companies, including medical records, treatment plans, and justifications for the necessity of the requested service. Insurance companies then review these submissions, which can take anywhere from a few days to several weeks, or even longer in complex cases. These delays can be critical, particularly for time-sensitive treatments such as cancer care or urgent surgeries.
The uncertainty created by the waiting period adds stress to patients already grappling with illness, and often leads to compromised treatment plans. For example, a patient needing a specific medication for a chronic condition might experience a worsening of their symptoms while waiting for approval, leading to potentially avoidable hospitalizations or complications.
Administrative Burden on Healthcare Providers
Prior authorization places a significant administrative burden on healthcare providers. Doctors and their staff spend considerable time and resources completing and submitting authorization requests, often using complex and often varying online portals for each insurer. This administrative work diverts valuable time and resources away from direct patient care, leading to increased operational costs for medical practices. The process often requires multiple follow-up calls and faxes to insurance companies to clarify requests or expedite approvals, further impacting efficiency and productivity.
Estimates suggest that physicians spend an average of 15 minutes per authorization request, which translates to significant lost time that could be used for patient interaction and care.
Examples of Delayed or Denied Medically Necessary Care
Numerous documented cases highlight the negative impact of prior authorization on patient care. For instance, a patient requiring a specific type of physical therapy for rehabilitation after a stroke might face delays in starting treatment, impacting their recovery. Similarly, a patient diagnosed with a specific type of cancer may experience a delay in initiating chemotherapy, which could negatively affect their prognosis.
Denials of prior authorization are also common, leading to patients being forced to appeal the decision, a process that further delays care and adds to their stress. These delays and denials are not only frustrating but can also have serious consequences for patient health and well-being.
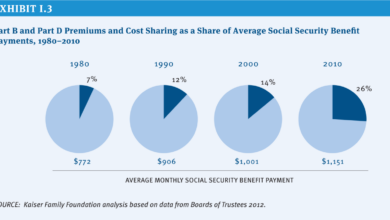
Comparison of Prior Authorization Processes Across Insurance Providers
The prior authorization process varies significantly across different insurance providers. The complexity of the process, the required documentation, and the turnaround time can differ considerably. This table provides a simplified comparison, noting that individual experiences may vary.
The American Medical Association’s fight against prior authorization delays highlights a critical issue: timely access to necessary care. Stories like Monali Thakur’s hospitalization, detailed in this article monali thakur hospitalised after struggling to breathe how to prevent respiratory diseases , underscore the urgency. Her breathing difficulties could have been better managed with quicker access to treatment, a stark reminder of how prior authorization needlessly obstructs vital medical interventions.
| Insurance Provider | Online Portal Availability | Average Turnaround Time (Days) | Required Documentation |
|---|---|---|---|
| Provider A | Yes, user-friendly | 3-5 | Referral, treatment plan, medical records |
| Provider B | Yes, but complex | 7-10 | Referral, treatment plan, medical records, specialist notes |
| Provider C | No, fax only | 10-14 | Referral, treatment plan, medical records, pre-authorization form |
| Provider D | Yes, but requires multiple logins | 5-7 | Referral, treatment plan, medical records, patient history |
Financial Implications of Prior Authorization Delays
Prior authorization, while intended to control healthcare costs, often creates significant financial burdens for patients. Delays in obtaining necessary care due to these processes can lead to a cascade of negative financial consequences, impacting individuals and families in profound ways. These delays not only increase direct medical expenses but also indirectly affect patients through lost wages, increased debt, and diminished quality of life.The increased healthcare costs associated with prolonged treatment due to prior authorization delays are substantial.
When treatment is delayed, conditions can worsen, requiring more extensive and expensive interventions later. A simple, treatable infection, for example, might progress to a severe, hospital-requiring illness if timely access to medication or procedures is blocked by prior authorization delays. This escalation of care dramatically increases the overall cost of treatment, ultimately placing a greater financial strain on the patient.
Financial Hardship Due to Prior Authorization Issues
Data on the precise number of patients experiencing financial hardship due to prior authorization issues is difficult to obtain comprehensively. However, numerous studies and anecdotal evidence consistently point to a significant problem. The American Medical Association, for example, has highlighted the considerable financial strain placed on patients and their families as a result of unnecessary delays in accessing care.
Many patients report accumulating significant medical debt, facing difficulty paying for essential necessities, and experiencing emotional distress related to their financial predicament. This often results in patients forgoing necessary care altogether, leading to further health complications and increased long-term costs.
Case Study: The Impact of Prior Authorization Delay on Healthcare Expenses, Prior authorization stands in way medically necessary care american medical association
Consider the case of Sarah, a 45-year-old single mother with type 1 diabetes. Sarah requires a specific insulin pump to manage her condition effectively. Her insurance company requires prior authorization for this pump, initiating a process that takes six weeks. During this delay, Sarah experiences several hyperglycemic episodes requiring emergency room visits, incurring significant costs for ambulance transportation, emergency room fees, and subsequent hospitalizations.
These unforeseen expenses, coupled with lost wages from missed work due to her illness, total approximately $15,000, far exceeding the cost of the insulin pump itself. Had the prior authorization process been expedited, Sarah would have avoided these substantial additional expenses, preventing a significant financial setback. This scenario illustrates how prior authorization delays can exponentially increase healthcare costs for patients, pushing them into financial hardship.
The AMA’s Position on Prior Authorization Reform
The American Medical Association (AMA) has been a vocal advocate for significant reform of the prior authorization process, arguing that it creates substantial burdens for physicians and ultimately hinders patient access to timely and necessary care. Their position rests on the belief that the current system is inefficient, overly bureaucratic, and contributes to significant administrative costs within the healthcare system.The AMA’s stance isn’t simply about reducing paperwork; it’s about ensuring patients receive the care they need when they need it.
They contend that prior authorization delays can lead to worsening health conditions, increased hospitalizations, and even preventable deaths. The organization’s efforts focus on practical solutions to streamline the process and reduce the administrative burden on physicians.
AMA’s Key Policy Recommendations for Prior Authorization Reform
The AMA has proposed several key policy recommendations aimed at reforming the prior authorization process. These recommendations are designed to improve efficiency, reduce administrative burden, and enhance patient access to care. Their approach focuses on both technological solutions and regulatory changes.The AMA advocates for the implementation of advanced technology, such as electronic prior authorization systems that allow for real-time decision-making.
This would eliminate the need for fax machines and manual processes, which are notorious for delays and errors. They also strongly support the development of standardized criteria for prior authorization requests, making the process more transparent and predictable for physicians. Furthermore, the AMA urges the establishment of clear timeframes for processing prior authorization requests, with penalties for payers who fail to meet those deadlines.
Finally, they propose the implementation of robust appeals processes to ensure that legitimate requests for care aren’t arbitrarily denied.
Comparison of AMA Recommendations with Current Legislative Efforts
While the AMA’s recommendations align with many current legislative efforts at both the state and federal levels, there are still significant gaps. Many states have enacted laws aimed at streamlining prior authorization, often focusing on specific specialties or types of services. However, these laws are often fragmented and lack the comprehensive approach advocated by the AMA. At the federal level, while there’s growing bipartisan support for prior authorization reform, legislative progress has been slower than many would like.
The AMA actively lobbies for federal legislation that would establish national standards for prior authorization, ensuring consistency across states and payers. The challenge lies in balancing the need for patient protection with the concerns of payers regarding cost containment.
The American Medical Association’s concerns about prior authorization delaying necessary care are completely valid. The sheer volume of paperwork involved is overwhelming, and this is exacerbated by the current medical coding worker shortage. A potential solution lies in leveraging technology, like what’s discussed in this insightful article on the ai powered solution to the medical coding worker shortage , which could streamline the process and ultimately get patients the treatment they need faster.
Hopefully, AI can help alleviate the bottleneck created by prior authorization and its impact on timely care.
Key Arguments Used by the AMA to Support Prior Authorization Reform
The AMA’s arguments for prior authorization reform center around several core tenets. First, they highlight the significant administrative burden placed on physicians and their staff, diverting valuable time and resources away from direct patient care. Second, they emphasize the negative impact on patient access to timely and appropriate care, leading to potentially worse health outcomes. Third, the AMA points to the substantial financial implications of prior authorization delays, including increased healthcare costs due to avoidable hospitalizations and emergency room visits.
Finally, they stress the importance of improving the efficiency and transparency of the prior authorization process to ensure that patients receive the care they need without unnecessary delays or bureaucratic hurdles. They consistently argue that a reformed system would not only benefit patients and physicians but also contribute to a more efficient and cost-effective healthcare system overall.
Patient Experiences with Prior Authorization: Prior Authorization Stands In Way Medically Necessary Care American Medical Association
Source: ama-assn.org
Prior authorization, a seemingly simple administrative hurdle, frequently transforms into a significant obstacle for patients seeking timely and necessary medical care. The process, often involving extensive paperwork, phone calls, and delays, places an undue burden on individuals already grappling with health concerns. This section explores the real-life impacts of prior authorization on patients and their families, highlighting the emotional toll and negative health consequences.The emotional toll of navigating the prior authorization process is substantial.
Patients often feel frustrated, anxious, and even hopeless as they grapple with bureaucratic red tape while their health deteriorates. The added stress can exacerbate existing health problems and negatively impact their overall well-being. Imagine a cancer patient whose crucial chemotherapy is delayed due to a prior authorization snafu; the anxiety and fear are immense, potentially impacting treatment efficacy and prognosis.
Similarly, a patient with a chronic condition needing a prescription refill might face weeks of pain and discomfort while waiting for approval, leading to potential complications and hospitalizations.
Negative Health Outcomes Associated with Prior Authorization Delays
Delays caused by prior authorization procedures have been directly linked to a range of negative health outcomes. Studies have shown a correlation between these delays and increased hospital readmissions, worsening of chronic conditions, and even increased mortality rates in certain cases. For instance, a delay in obtaining authorization for a necessary medication for a heart condition could lead to a cardiac event, resulting in hospitalization or even death.
The American Medical Association rightly highlights how prior authorization delays crucial medical care. This bureaucratic hurdle is especially frustrating when considering conditions like carpal tunnel syndrome; thankfully, there are often non-surgical options. For example, check out this helpful resource on ways to treat carpal tunnel syndrome without surgery to see if less invasive treatments might be available.
Ultimately, the prior authorization process needs reform to ensure patients receive timely, necessary treatment.
The longer the delay, the greater the risk of negative consequences. This isn’t just about inconvenience; it’s about jeopardizing health and potentially lives.
Examples of Patient Testimonials
The stories of patients impacted by prior authorization are heartbreaking and alarming. One patient, a diabetic needing a specialized insulin pump, reported spending weeks on the phone with insurance companies and doctors’ offices, only to have their request repeatedly denied due to technicalities. During this period, her blood sugar levels fluctuated dangerously, leading to several hospital visits and significant health complications.
Another patient, a mother of a child with asthma, described the agonizing wait for authorization for a nebulizer, resulting in several severe asthma attacks before approval was finally granted. These are not isolated incidents; they represent a systemic problem causing unnecessary suffering.
Common Patient Complaints Regarding Prior Authorization
The frustration and anger experienced by patients are often palpable. Here are some of the most common complaints:
- Excessive paperwork and complex forms requiring significant time and effort.
- Lengthy wait times for authorization decisions, often exceeding weeks or even months.
- Confusing and inconsistent requirements from different insurance providers.
- Lack of transparency and communication throughout the process.
- Difficulty reaching a knowledgeable representative to address concerns.
- Denial of authorization for medically necessary treatments or medications.
- The feeling of being treated as a number rather than a patient with individual needs.
Potential Solutions and Reforms
Source: chiromi.com
The current prior authorization system places an unacceptable burden on healthcare providers and patients. The good news is that numerous solutions exist to streamline this process and improve access to necessary care. These solutions involve a combination of technological advancements, policy changes, and alternative authorization models. By implementing these reforms, we can create a more efficient and patient-centered healthcare system.
Technological Solutions for Streamlining Prior Authorization
The sheer volume of prior authorization requests can be significantly reduced through technological innovation. Real-time electronic prior authorization systems, integrated directly into electronic health record (EHR) systems, can drastically cut down on administrative overhead. These systems allow for immediate decisions on authorization, eliminating the delays inherent in paper-based processes. Furthermore, the use of artificial intelligence (AI) and machine learning can help predict which requests are likely to be approved, reducing the need for manual review in many cases.
For example, an AI system could analyze patient data and treatment plans to identify cases that consistently meet pre-defined criteria for approval, automatically authorizing these treatments while flagging only those requiring additional review. This automation would free up staff time for more complex cases, ultimately improving efficiency and reducing the overall burden.
Policy Changes to Improve Prior Authorization Efficiency
Policy changes at both the state and federal levels are crucial for improving the prior authorization process. One important step is to establish clear, standardized criteria for prior authorization requests. Ambiguous or inconsistently applied criteria contribute significantly to delays. Implementing consistent guidelines across payers would significantly improve predictability and reduce the need for repeated requests or appeals.
Furthermore, legislation could mandate shorter turnaround times for prior authorization decisions, with penalties for payers who consistently fail to meet these deadlines. This would incentivize payers to improve their processes and reduce delays in accessing care. For instance, a state could mandate a 24-hour turnaround time for urgent requests and a 72-hour turnaround for non-urgent requests, with penalties for non-compliance.
Benefits of Alternative Prior Authorization Models
Moving away from the current retrospective authorization model towards pre-authorization or other alternative models offers significant advantages. Pre-authorization, where authorization is obtainedbefore* treatment begins, eliminates the delays and uncertainty associated with the current system. Retrospective review, where authorization is reviewed after treatment, reduces the administrative burden on providers but requires trust and transparency between payers and providers. Both models reduce the potential for delays in critical care, allowing providers to focus on patient care rather than administrative tasks.
For example, a pre-authorization system for cancer treatment could allow oncologists to begin treatment immediately upon diagnosis, rather than waiting weeks for approval. This can be crucial in cases where prompt treatment significantly improves patient outcomes.
Successful Prior Authorization Reform Initiatives
Several states and countries have successfully implemented prior authorization reforms. For example, some states have adopted legislation requiring payers to use real-time electronic prior authorization systems, resulting in significant reductions in processing times. Other states have established independent review boards to adjudicate disputes between providers and payers, ensuring a fair and transparent process. These initiatives demonstrate that meaningful progress can be made in improving prior authorization through focused legislative action and collaborative efforts between stakeholders.
The success of these initiatives highlights the potential for wider adoption of these reforms to improve access to timely and appropriate care across the nation.
The Role of Technology in Improving Prior Authorization
The current prior authorization process is notoriously cumbersome, creating significant delays in patient care and adding substantial administrative burden to both healthcare providers and payers. The good news is that technology offers a powerful solution to streamline this process, reducing delays and improving efficiency for all stakeholders. Electronic prior authorization systems are rapidly becoming the standard, offering a significant upgrade over the antiquated manual systems still prevalent in many healthcare settings.Electronic prior authorization systems significantly reduce delays and administrative burdens by automating many of the steps involved in the traditional paper-based process.
Instead of faxing forms, making phone calls, and manually tracking requests, electronic systems allow for real-time submission and tracking of authorization requests. This automation minimizes the risk of lost paperwork, reduces manual data entry errors, and enables faster decision-making. The result is a quicker turnaround time for approvals, leading to less disruption in patient care and reduced frustration for providers and staff.
Features of an Ideal Electronic Prior Authorization System
An ideal electronic prior authorization system would incorporate several key features to benefit both providers and payers. It would need a user-friendly interface, easily accessible to all stakeholders, with robust data security measures in place to protect sensitive patient information. The system should integrate seamlessly with existing electronic health record (EHR) systems, allowing for automatic population of relevant patient data and minimizing the need for manual data entry.
Furthermore, it should offer real-time tracking of requests, clear communication between providers and payers, and automated alerts to notify providers of approvals or denials. Finally, it should be able to generate comprehensive reports and analytics to track performance and identify areas for improvement.
Comparison of Manual and Electronic Prior Authorization Processes
The difference in efficiency between manual and electronic prior authorization processes is stark. Manual processes, relying on paper forms and fax machines, are slow, prone to errors, and require significant administrative overhead. Studies have shown that manual processes can take weeks, sometimes even months, to complete, leading to significant delays in patient care. In contrast, electronic systems can process requests in a matter of days, or even hours, in some cases.
This significant reduction in processing time translates directly into improved patient outcomes and reduced costs associated with delayed treatment. For example, a study published in the
American Journal of Managed Care* found that electronic prior authorization reduced the average processing time from 7 days to less than 24 hours.
Improving the Prior Authorization Process with a Specific Technology: AI-Powered Decision Support
One specific technology with the potential to significantly improve the prior authorization process is an AI-powered decision support system. This type of system uses machine learning algorithms to analyze patient data, treatment plans, and prior authorization criteria to predict the likelihood of approval. The system can then automatically pre-fill authorization requests with the most relevant information, identify potential issues that might lead to denials, and even suggest alternative treatments that are more likely to be approved.
This proactive approach reduces the time and effort required to complete the authorization process, minimizes denials, and ensures that patients receive the care they need in a timely manner. For instance, an AI system could analyze a patient’s medical history and proposed treatment to identify potential red flags based on payer guidelines, flagging potential issues before the request is even submitted, allowing the provider to address these proactively and increasing the likelihood of a first-pass approval.
The resulting efficiency gains would be substantial, leading to reduced administrative costs and improved patient care.
Conclusive Thoughts
The fight to reform prior authorization is far from over, but the AMA’s stance, along with the countless stories of patients struggling to access necessary care, is shining a much-needed light on this critical issue. The sheer human cost of this system is undeniable, and the need for swift and effective change is urgent. We need innovative solutions, coupled with strong policy reform, to ensure that prior authorization doesn’t stand in the way of timely, life-saving medical care.
The future of healthcare depends on it.
Essential Questionnaire
What exactly is prior authorization?
Prior authorization is the process where a patient’s doctor must obtain approval from their insurance company before certain medical treatments or procedures can be provided.
How long does prior authorization typically take?
It varies widely, but delays of days, weeks, or even months are not uncommon, causing significant disruptions to care.
Can I appeal a denied prior authorization?
Yes, but the appeals process can be complex and time-consuming. You should contact your insurance provider to understand their specific appeals process.
What are some examples of treatments requiring prior authorization?
Many expensive medications, specialized tests, and certain surgeries often require prior authorization.