The Next Era of Hospital Healthtech and Outsourced Provider Partnerships
The next era of hospital healthtech and outsourced provider partnerships is dawning, ushering in a transformative period for healthcare delivery. Imagine a future where AI-powered diagnostics seamlessly integrate with remote patient monitoring, all managed by expertly coordinated outsourced teams. This isn’t science fiction; it’s the rapidly evolving reality fueled by technological advancements and the increasing demand for efficient, high-quality care.
This post dives into the exciting potential – and the inevitable challenges – of this rapidly evolving landscape.
We’ll explore how artificial intelligence, cloud computing, and data analytics are revolutionizing hospital operations, improving patient care, and driving down costs. We’ll also delve into the different models of outsourced provider partnerships, examining their benefits, challenges, and the legal considerations involved. Get ready for a deep dive into the synergies between healthtech and outsourcing, and how this powerful combination is reshaping the future of healthcare.
The Evolving Landscape of Hospital Healthtech
The healthcare industry is undergoing a digital transformation, driven by advancements in technology and a growing need for improved efficiency and patient care. Hospitals are at the forefront of this change, rapidly adopting new health technologies to enhance their operations and deliver better outcomes. This evolution is marked by the integration of artificial intelligence, cloud computing, and sophisticated data analytics, leading to a fundamentally different approach to healthcare delivery.
Artificial Intelligence and Machine Learning in Hospital Operations
Artificial intelligence (AI) and machine learning (ML) are revolutionizing various aspects of hospital operations. AI-powered diagnostic tools can analyze medical images with greater speed and accuracy than human radiologists, leading to faster diagnoses and treatment plans. Predictive analytics, using ML algorithms, can identify patients at high risk of developing complications, allowing for proactive interventions and improved patient outcomes.
For instance, AI can predict sepsis onset hours in advance, giving medical teams crucial time to administer life-saving treatment. Furthermore, AI-powered chatbots are being deployed to handle routine patient inquiries, freeing up staff for more complex tasks. These technologies are not just improving efficiency; they are directly contributing to better patient care and potentially saving lives.
The Role of Cloud Computing and Data Analytics in Improving Patient Care and Operational Efficiency
Cloud computing provides hospitals with scalable and cost-effective solutions for storing and managing vast amounts of patient data. This allows for seamless data sharing between different departments and healthcare providers, improving coordination of care. Data analytics, applied to this cloud-based data, allows hospitals to identify trends, improve resource allocation, and optimize workflows. For example, analyzing patient flow data can reveal bottlenecks in the emergency room, enabling hospitals to implement strategies to reduce wait times.
Similarly, analyzing medication usage data can help identify potential adverse drug reactions and prevent medication errors. The combined power of cloud computing and data analytics is essential for creating a more efficient and patient-centered healthcare system.
Comparison of Traditional Hospital Systems with Emerging Healthtech Solutions
The following table highlights the key differences between traditional hospital systems and the emerging healthtech solutions:
| Feature | Traditional Hospital Systems | Emerging Healthtech Solutions |
|---|---|---|
| Data Storage | On-premise servers, often siloed data | Cloud-based storage, centralized data repositories |
| Diagnostics | Primarily reliant on human interpretation of images and tests | AI-powered diagnostic tools for faster and more accurate results |
| Patient Monitoring | Manual monitoring, potential for delays in identifying critical changes | Real-time remote patient monitoring with wearable sensors and AI-driven alerts |
| Administrative Tasks | Manual processes, prone to errors and inefficiencies | Automation of administrative tasks through robotic process automation (RPA) and AI |
The Rise of Outsourced Provider Partnerships

Source: ttgtmedia.com
The healthcare industry is undergoing a dramatic transformation, driven by escalating costs, evolving patient expectations, and a growing shortage of specialized healthcare professionals. One significant response to these challenges is the burgeoning trend of outsourced provider partnerships. Hospitals and health systems are increasingly leveraging external expertise and resources to enhance efficiency, improve quality of care, and ultimately, improve their bottom line.
This shift represents a fundamental change in the traditional model of healthcare delivery.The growth of outsourced provider partnerships is fueled by several key factors. Firstly, the increasing complexity of healthcare necessitates specialized skills and technology that individual hospitals may not possess or be able to afford. Secondly, the persistent physician shortage, particularly in specialized areas, compels hospitals to seek external partnerships to fill critical gaps in service.
Thirdly, the pressure to control costs and improve operational efficiency is pushing hospitals to outsource non-core functions, allowing them to focus on their core competencies. Finally, the desire to improve patient outcomes and satisfaction through access to cutting-edge technologies and expertise is driving this trend.
Models of Outsourced Provider Partnerships
Outsourced provider partnerships come in various forms, each with its own advantages and disadvantages. Two prominent models are revenue-based and performance-based partnerships. Revenue-based partnerships typically involve a fixed fee or percentage of revenue generated from the outsourced services. This model offers predictability for the hospital but may not incentivize the provider to optimize performance. Performance-based partnerships, conversely, tie the provider’s compensation to the achievement of pre-defined metrics, such as patient satisfaction scores, readmission rates, or cost reduction targets.
This model aligns the incentives of both parties, encouraging a focus on quality and efficiency. For example, a hospital might partner with a specialized radiology group on a performance-based model, where the radiology group’s compensation is tied to the timely delivery of accurate reports and efficient scheduling. A revenue-based model, in contrast, might see a flat fee paid regardless of efficiency.
Benefits and Challenges of Outsourcing Healthcare Services
Outsourcing healthcare services offers several potential benefits. It can improve access to specialized care, enhance operational efficiency, reduce administrative burdens, and free up internal resources for core functions. It can also lead to improved quality of care through access to advanced technologies and best practices. However, outsourcing also presents challenges. These include potential risks to data security and patient privacy, the need for robust contract management and oversight, and the potential for communication and coordination challenges between the hospital and the outsourced provider.
Maintaining consistent quality of care and ensuring seamless patient transitions are also crucial considerations. For instance, a poorly managed outsourcing arrangement could lead to delays in patient care, impacting patient satisfaction and potentially legal ramifications.
Regulatory and Legal Considerations
Establishing outsourced provider partnerships involves careful consideration of various regulatory and legal aspects. Compliance with HIPAA regulations regarding patient privacy and data security is paramount. Contracts must clearly define responsibilities, liabilities, and performance expectations. State licensing requirements for healthcare providers must be adhered to, and appropriate credentialing and privileging processes must be followed. Antitrust laws must also be considered to ensure that partnerships do not create monopolies or restrict competition.
Failure to address these legal and regulatory considerations can result in significant financial penalties and reputational damage. For example, a hospital failing to ensure HIPAA compliance through its outsourced provider could face substantial fines and legal action. Thorough due diligence and legal counsel are essential throughout the process.
Synergies Between Healthtech and Outsourced Partnerships: The Next Era Of Hospital Healthtech And Outsourced Provider Partnerships

Source: forbesindia.com
The convergence of advanced health technologies and the increasing reliance on outsourced provider partnerships is reshaping the healthcare landscape. This synergy is not merely coincidental; it’s a powerful driver of efficiency, cost-effectiveness, and improved patient care. Advancements in healthtech are directly enabling and expanding the capabilities of outsourced providers, leading to more comprehensive and integrated healthcare delivery models.The expansion of outsourced provider partnerships is significantly facilitated by advancements in healthtech.
The next era of hospital healthtech hinges on strong partnerships, especially with outsourced providers. Understanding the financial landscape is crucial, and the recent elevance health earnings Q1 change, including the impact of their cyberattack and shifts in Medicaid and Medicare Advantage , highlights the complexities involved. This financial volatility underscores the need for robust, adaptable healthtech solutions within these evolving provider relationships.
Telehealth platforms, for instance, allow specialists located remotely to provide consultations and monitor patients, effectively extending the reach of hospital systems beyond their geographical limitations. Similarly, robust electronic health record (EHR) systems and interoperable data exchange platforms make it easier for outsourced providers to seamlessly access and share patient information with hospital staff, ensuring continuity of care and reducing administrative burdens.
The next era of hospital healthtech hinges on smart partnerships, leveraging outsourced providers for specialized services. However, recent news about Steward Health Care, like this article on Steward Ohio hospitals closures and a Pennsylvania facility at risk , highlights the precariousness of even large systems. This underscores the need for robust risk management strategies within these new healthtech partnerships to ensure both financial stability and patient care.
The use of AI-powered diagnostic tools also allows outsourced providers to analyze medical images and data more efficiently, leading to faster and more accurate diagnoses.
Examples of Successful Collaborations
Successful collaborations between hospitals and outsourced providers often leverage healthtech to achieve shared goals. For example, a large hospital system might outsource its radiology services to a specialized imaging center equipped with cutting-edge AI-powered diagnostic tools. This allows the hospital to focus on its core competencies while benefiting from the expertise and advanced technology of the outsourced provider. Another example involves a hospital partnering with a telehealth provider to offer remote patient monitoring for patients with chronic conditions.
This partnership uses wearable sensors and connected devices to collect real-time health data, which is then analyzed by the outsourced provider to identify potential problems and alert hospital staff. The resulting proactive care approach improves patient outcomes and reduces hospital readmissions. These examples demonstrate the value of integrating technology into outsourced partnerships.
Best Practices for Integrating Healthtech Solutions
Effective integration of healthtech solutions within outsourced provider partnerships requires careful planning and execution. Key best practices include establishing clear communication channels and data sharing protocols between the hospital and outsourced provider. This ensures seamless information flow and avoids potential data silos. Robust cybersecurity measures are also crucial to protect sensitive patient data. Finally, ongoing monitoring and evaluation of the integrated healthtech solutions are necessary to ensure they are meeting their intended goals and to identify areas for improvement.
A well-defined service level agreement (SLA) outlining responsibilities, performance metrics, and escalation procedures is essential for a successful partnership.
Framework for Evaluating Healthtech Implementations, The next era of hospital healthtech and outsourced provider partnerships
A comprehensive framework for evaluating the effectiveness of healthtech implementations within outsourced partnerships should incorporate both quantitative and qualitative metrics. Quantitative metrics might include reductions in wait times, improvements in diagnostic accuracy, decreases in hospital readmissions, and cost savings. Qualitative metrics could involve patient satisfaction surveys, staff feedback on the usability of the technology, and assessments of the overall efficiency of the integrated system.
This framework allows for a holistic evaluation of the partnership’s success and facilitates data-driven decision-making for future improvements. Regular review of these metrics, perhaps quarterly or annually, is key to adapting the partnership and technology use to ensure ongoing effectiveness.
Impact on Patient Care and Outcomes
The burgeoning partnerships between hospitals and outsourced healthcare providers, facilitated by advancements in healthtech, hold significant potential to reshape patient care. This transformation hinges on improved access, enhanced quality, and a more streamlined patient experience. However, realizing this potential requires careful consideration of data security and the effective integration of technology to foster seamless communication and collaboration.The impact of these partnerships on patient care is multifaceted.
Increased access to specialized services, particularly in underserved areas, is a key benefit. Outsourcing allows hospitals to leverage the expertise of specialists without the need for significant capital investment in infrastructure or staffing. This is especially crucial for procedures requiring advanced technology or highly specialized personnel, which might otherwise be unavailable to patients in smaller hospitals or rural communities.
For example, a rural hospital partnering with a large urban cardiology practice via telehealth could provide timely access to specialist consultations and potentially life-saving interventions for heart patients.
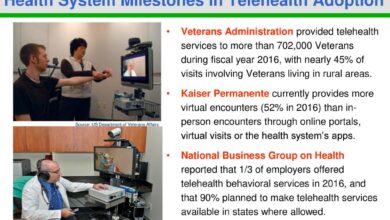
Improved Access to Care
Improved access to care is a direct result of these partnerships. The geographical limitations often faced by patients seeking specialized care can be significantly reduced through telehealth platforms and remote monitoring technologies. This allows for timely consultations and treatment, minimizing delays and improving overall health outcomes. For instance, a partnership between a hospital and a telemedicine provider could offer remote monitoring of chronic conditions like diabetes, reducing hospital readmissions and improving patient management.
Enhanced Quality of Care
Partnerships can improve the quality of care through access to specialized expertise and advanced technologies. Outsourced providers often bring cutting-edge medical knowledge and technological capabilities that may not be readily available within a single hospital system. This translates to better diagnostic accuracy, more effective treatment strategies, and improved patient outcomes. A partnership with a specialized radiology group, for example, could provide access to advanced imaging techniques and interpretation, leading to earlier detection of diseases and more precise treatment plans.
Patient Experience Enhancement
Streamlined processes and improved communication facilitated by healthtech are key to enhancing the patient experience. Integrated systems allow for seamless information sharing between hospitals and outsourced providers, minimizing administrative burdens and reducing the potential for medical errors. Patient portals and mobile apps can empower patients to actively participate in their care, increasing satisfaction and adherence to treatment plans.
For instance, a patient using a portal to access their test results and communicate with their physician directly experiences a more efficient and convenient healthcare journey.
Data Security and Privacy in Outsourced Provider Partnerships
Data security and patient privacy are paramount concerns in outsourced provider partnerships. Robust data security protocols, including encryption, access controls, and regular security audits, are essential to protect sensitive patient information. Compliance with regulations like HIPAA (in the US) is crucial, and ongoing monitoring and training are necessary to mitigate risks. Hospitals must carefully vet potential partners, ensuring they have adequate security measures in place and a proven track record of data protection.
The consequences of a data breach can be severe, damaging patient trust and incurring significant financial penalties.
Healthtech’s Role in Communication and Coordination
Healthtech plays a vital role in improving communication and coordination between hospitals and outsourced providers. Secure messaging platforms, electronic health records (EHR) integration, and telehealth platforms facilitate real-time communication and information sharing. This improves care coordination, reduces medical errors, and enhances the overall efficiency of the healthcare system. For example, the use of a shared EHR system allows hospital staff and outsourced specialists to access the same patient information, reducing the need for repeated data entry and ensuring everyone is working with the most up-to-date information.
Key Performance Indicators (KPIs) for Measuring Success
Measuring the success of these partnerships in improving patient outcomes requires a comprehensive set of KPIs. These should track improvements across various aspects of care.
The following KPIs can be used to assess the effectiveness of the partnerships:
- Reduced hospital readmission rates: Indicates improved post-discharge care and management of chronic conditions.
- Improved patient satisfaction scores: Reflects the overall patient experience, including access, communication, and quality of care.
- Increased patient adherence to treatment plans: Shows the effectiveness of communication and patient engagement strategies.
- Reduced length of hospital stay: Demonstrates efficiency in diagnosis and treatment.
- Lower healthcare costs per patient: Indicates efficient resource utilization and cost-effectiveness of the partnership.
- Improved diagnostic accuracy: Reflects the quality of care provided by outsourced specialists.
- Enhanced patient access to specialized care: Measures the success of expanding access to specialized services.
- Reduced wait times for appointments and procedures: Indicates improved efficiency in scheduling and resource allocation.
Future Directions and Challenges
The integration of outsourced provider partnerships with hospital healthtech, while promising, faces significant hurdles on the path to widespread adoption. Successfully navigating these challenges will require careful planning, proactive risk mitigation, and a commitment to ethical practices. The future success of this model hinges on addressing these complexities and capitalizing on emerging trends.
The next era of hospital healthtech hinges on strong outsourced provider partnerships, streamlining care and reducing costs. This collaborative approach extends beyond hospital walls; consider how effective partnerships are vital, as highlighted in this excellent article on reimagining collaboration in senior care a technology-driven approach , which shows how technology fosters better outcomes in senior care.
Ultimately, successful hospital healthtech strategies will rely on these expanded partnerships for efficient and comprehensive patient care.
Challenges and Obstacles to Widespread Adoption
Several key obstacles hinder the widespread adoption of integrated outsourced provider partnerships and healthtech. Data security and privacy remain paramount concerns, particularly when sensitive patient information is shared across multiple systems and organizations. Interoperability issues between different healthtech platforms and the systems used by outsourced providers can create significant integration challenges, leading to data silos and inefficient workflows.
Furthermore, the regulatory landscape is constantly evolving, requiring ongoing adaptation and compliance. Finally, establishing clear lines of accountability and responsibility when issues arise within the partnership can be complex and needs careful contractual consideration. For example, a failure in a telehealth platform provided by an outsourced vendor could lead to significant legal and reputational damage for the hospital, even if the hospital itself wasn’t directly responsible for the technical malfunction.
Ethical Considerations in Outsourced Provider Partnerships and Healthtech
Ethical considerations are central to the responsible use of healthtech within outsourced provider partnerships. Maintaining patient privacy and data security is paramount. Robust data encryption, access control mechanisms, and compliance with regulations like HIPAA are essential. Transparency is also critical; patients need to be fully informed about the involvement of outsourced providers and how their data is being used.
The potential for bias in algorithms used in healthtech needs careful consideration, ensuring fairness and equitable access to care for all patient populations. Finally, the allocation of responsibility for clinical decisions made using healthtech by outsourced providers needs clear definition to avoid conflicts of interest and ensure patient safety. A real-world example could involve an AI-powered diagnostic tool suggesting a course of treatment that conflicts with a physician’s assessment; this necessitates clear protocols for resolving such discrepancies.
Future Trends in Hospital Healthtech and Outsourced Provider Partnerships
Several key trends are shaping the future of this evolving landscape. Artificial intelligence (AI) and machine learning (ML) will continue to play an increasingly significant role in improving diagnostic accuracy, personalizing treatment plans, and streamlining administrative tasks. The expansion of telehealth services will likely accelerate, driven by both patient demand and cost-effectiveness. Blockchain technology offers the potential to enhance data security and interoperability, fostering greater trust and transparency.
Finally, a greater focus on data analytics will enable hospitals and outsourced providers to gain valuable insights into patient populations, leading to improved resource allocation and more effective care delivery. For instance, predictive analytics could help hospitals anticipate surges in patient volume during flu season, allowing them to proactively adjust staffing and resource allocation.
Visual Representation of Future Evolution
The illustration depicts a central hub representing the hospital, connected to various specialized outsourced providers (e.g., radiology, pathology, telehealth) via secure, high-bandwidth digital connections. These connections are represented by brightly colored, interconnected lines, symbolizing seamless data flow and communication. Each outsourced provider is depicted as a smaller, specialized node, indicating their individual expertise. Surrounding the entire network is a protective shield, representing robust cybersecurity measures and data privacy protocols.
The hospital hub incorporates AI-powered systems and data analytics dashboards, highlighting the use of advanced technology for improved decision-making. The overall image conveys a dynamic, interconnected ecosystem where technology facilitates efficient and secure collaboration between the hospital and its outsourced partners, ultimately benefiting patient care.
Last Word
The convergence of hospital healthtech and outsourced provider partnerships represents a pivotal moment in healthcare. While challenges remain – particularly regarding data security and ethical considerations – the potential benefits for patients and providers are undeniable. By embracing innovative technologies and strategically leveraging outsourced expertise, hospitals can enhance efficiency, improve patient outcomes, and ultimately, create a more sustainable and accessible healthcare system.
The future of healthcare is collaborative, technologically advanced, and undeniably exciting. Let’s embrace the opportunities and navigate the challenges together.
General Inquiries
What are the biggest risks associated with outsourcing healthcare services?
The biggest risks include data breaches, compromised patient privacy, potential quality inconsistencies, and difficulties in maintaining consistent communication and coordination.
How can hospitals ensure data security and privacy in outsourced partnerships?
Robust contracts with stringent data security clauses, regular audits, employee training on data protection, and the implementation of advanced encryption technologies are crucial.
What are some examples of successful healthtech integrations in outsourced partnerships?
Examples include using telehealth platforms for remote patient monitoring, employing AI-powered diagnostic tools managed by outsourced radiologists, and leveraging data analytics to optimize resource allocation within outsourced care teams.
How will this partnership model affect healthcare costs?
The potential exists for both cost savings (through increased efficiency and reduced overhead) and increased costs (due to initial investment in technology and management of outsourced partnerships). The net effect will depend on effective implementation and management.