Smart Devices Reliable for Health? Doctors Weigh In
Are smart devices reliable for health monitoring doctors opinion on smart healthtech – Smart Devices Reliable for Health? Doctors Weigh In: We’re living in an age of wearable tech, where fitness trackers and smartwatches promise to revolutionize personal health management. But are these devices truly reliable for accurate health monitoring? This post dives into the opinions of medical professionals on the accuracy, limitations, and ethical considerations surrounding the integration of smart health technology into healthcare.
We’ll explore what doctors think about the data these devices provide and how it impacts clinical decision-making.
From the accuracy of heart rate monitors to the potential pitfalls of relying solely on smart device data for diagnoses, we’ll unpack the complexities of this rapidly evolving field. We’ll examine the perspectives of various medical specialties, the potential for misinterpretations, and the crucial role of patient education in responsible smart health technology use. Get ready to explore the fascinating intersection of technology and medicine!
Accuracy and Reliability of Smart Health Devices: Are Smart Devices Reliable For Health Monitoring Doctors Opinion On Smart Healthtech

Source: sensights.ai
Smart health devices, from fitness trackers to smartwatches and blood pressure monitors, are increasingly popular. However, their accuracy and reliability in providing truly reliable health data remain a significant concern, particularly when compared to traditional medical equipment used in clinical settings. While these devices offer convenience and can provide valuable insights into certain aspects of health, it’s crucial to understand their limitations.Smart health devices often rely on sensors and algorithms that, while sophisticated, are not perfect.
This can lead to inaccuracies in the data they collect, potentially misrepresenting an individual’s health status. This inaccuracy is further exacerbated by factors outside the device’s control.
Limitations of Smart Health Device Technology
Current smart health device technology faces several limitations in accurately reflecting physiological parameters when compared to professional medical equipment. Traditional medical equipment, such as electrocardiograms (ECGs) and laboratory tests, are designed and calibrated to meet stringent accuracy standards and undergo regular maintenance and calibration. Smart devices, on the other hand, often lack this level of precision and rigorous quality control.
The miniaturization required for wearable devices necessitates compromises in sensor sensitivity and signal processing capabilities. For instance, a smartwatch’s heart rate sensor might struggle to accurately measure heart rate during intense physical activity due to movement artifacts, while a hospital-grade ECG machine can provide a far more detailed and precise reading.
Examples of Misleading or Inaccurate Data
Several scenarios illustrate how smart device health data can be misleading. A fitness tracker might overestimate the number of calories burned during a workout due to inaccuracies in motion detection and individual metabolic rate variations. A smart blood pressure monitor might provide readings that are consistently higher or lower than those obtained with a clinically validated device due to improper cuff placement or inconsistent inflation pressure.
Similarly, sleep tracking apps, while useful for identifying general sleep patterns, may not accurately diagnose sleep disorders that require professional assessment. In these instances, relying solely on smart device data could lead to misinterpretations of one’s health and potentially inappropriate self-treatment.
Sources of Error in Data Collection
Several factors contribute to errors in data collected from smart health devices. Sensor inconsistencies, inherent to the manufacturing process, can cause variations in readings across devices and over time. User error, such as incorrect placement of a sensor or improper calibration, significantly impacts data accuracy. Environmental factors, such as temperature and humidity, can also influence sensor performance. For example, a fitness tracker’s GPS signal might be weak indoors or in areas with poor satellite coverage, leading to inaccurate distance tracking.
Furthermore, individual variations in physiology and skin characteristics can influence the quality of data obtained.
Accuracy Comparison of Smart Health Devices
The following table compares the accuracy of several common smart health devices across different health metrics. Note that the accuracy levels are general estimates and can vary significantly based on the specific device model, user factors, and environmental conditions.
| Device Type | Metric Measured | Accuracy Level | Limitations |
|---|---|---|---|
| Smartwatch | Heart Rate | Generally good at rest, less accurate during intense activity | Affected by movement artifacts, skin tone variations, sensor placement |
| Fitness Tracker | Steps Taken | Fairly accurate for general activity level | Can be affected by arm movement not related to walking/running, user calibration |
| Smart Blood Pressure Monitor | Blood Pressure | Variable, depends heavily on correct usage | Inaccurate readings if cuff is improperly placed or inflated, affected by movement |
| Smart Scale | Body Composition (Fat Mass, Muscle Mass) | Moderately accurate, less reliable for precise measurements | Affected by hydration levels, body temperature, and user consistency |
Doctors’ Perspectives on Smart Health Technology Integration
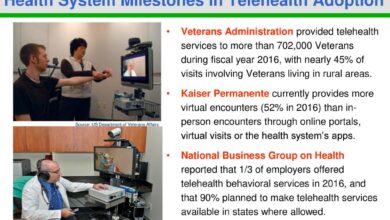
The rise of smart health devices presents a fascinating dichotomy in the medical field. While offering the potential for revolutionary improvements in patient care and preventative medicine, they also introduce significant challenges for doctors in terms of data interpretation, integration into existing workflows, and ethical considerations. This section explores the perspectives of medical professionals on this rapidly evolving landscape.The integration of data from smart health devices holds immense promise for improving routine medical care.
Imagine a scenario where a patient’s continuous glucose monitor seamlessly transmits data directly to their physician, allowing for proactive adjustments to diabetes management before complications arise. Or consider the potential for early detection of atrial fibrillation through a smart watch, leading to timely intervention and preventing strokes. These are just a few examples of how real-time data can enhance diagnosis, treatment, and overall patient outcomes.
So, are smart health devices truly reliable for monitoring health? Doctors have mixed opinions, often highlighting the need for careful data interpretation. For instance, managing conditions like Tourette Syndrome in children requires a multi-faceted approach, as detailed in this helpful article on strategies to manage Tourette syndrome in children , and this complexity underscores the limitations of relying solely on smart device data.
Ultimately, smart devices can be useful tools, but they shouldn’t replace professional medical advice.
Challenges in Interpreting and Utilizing Smart Health Device Data
Doctors face numerous hurdles in effectively utilizing the flood of data generated by smart health devices. The sheer volume and variety of data from different manufacturers, often using incompatible formats, pose a significant challenge. Furthermore, the accuracy and reliability of these devices vary considerably, requiring careful validation and interpretation. Integrating this data into existing electronic health record (EHR) systems also presents technical and logistical difficulties.
Standardization of data formats and the development of user-friendly interfaces are crucial for seamless integration. Doctors need tools that can efficiently filter, analyze, and contextualize this data within the broader clinical picture, avoiding information overload.
Ethical Concerns Related to Data Privacy and Security, Are smart devices reliable for health monitoring doctors opinion on smart healthtech
The collection and storage of sensitive health data by smart health devices raise significant ethical concerns. Data breaches, unauthorized access, and the potential for misuse of personal information are real risks. Clear regulations and robust security protocols are necessary to protect patient privacy and maintain trust in this technology. Informed consent regarding data collection, usage, and sharing is paramount.
Furthermore, the potential for algorithmic bias in data analysis and the implications for healthcare equity require careful consideration and mitigation strategies. Transparency and accountability are crucial in addressing these ethical challenges.
Varied Perspectives Across Medical Specialties
Different medical specialties hold varying perspectives on the value of smart health devices. Cardiologists, for example, may find continuous heart rate monitoring invaluable for detecting arrhythmias, while dermatologists might utilize image analysis tools for early skin cancer detection. However, specialties dealing with more complex conditions might find the data less immediately useful or require more sophisticated analytical tools.
For instance, psychiatrists might find challenges in interpreting data from wearable devices in relation to mental health conditions, requiring further research and development of specific algorithms and analytic approaches. Ultimately, the successful integration of smart health technology depends on the development of tailored solutions for individual specialties and conditions.
Data Interpretation and Clinical Decision-Making
Integrating data from smart health devices into clinical practice requires a careful and considered approach. Doctors must understand the limitations of these devices and interpret the data within the broader context of the patient’s overall health and medical history. Simply relying on the numbers generated by a wearable can be misleading, and a thorough understanding of the device’s capabilities and limitations is paramount.The process of evaluating health data from smart devices involves a multi-step approach that combines technological understanding with clinical expertise.
It is not a simple substitution for traditional methods but rather a valuable augmentation of existing diagnostic and monitoring tools.
Factors Influencing Clinical Significance of Smart Device Data
The clinical significance of data derived from smart health devices hinges on several critical factors. Ignoring these factors can lead to misinterpretations and potentially harmful clinical decisions. Careful consideration of these points is crucial for responsible integration of this technology.
- Device Accuracy and Validation: The reliability and accuracy of the specific device used must be established. Different devices have varying degrees of precision and may be validated for specific populations or health conditions only. A doctor should be aware of the device’s limitations and any known biases or inaccuracies.
- Data Context and Patient History: Smart device data should never be interpreted in isolation. A comprehensive understanding of the patient’s medical history, lifestyle, and current medications is essential. Data anomalies should be considered in light of this broader clinical picture.
- Data Completeness and Consistency: Incomplete or inconsistent data can lead to inaccurate conclusions. Gaps in data should be identified and addressed, and the doctor should assess the overall quality and reliability of the data stream before making any clinical decisions.
- Patient Compliance and Data Integrity: The accuracy of data is directly dependent on patient compliance in wearing and using the device correctly. Doctors should assess patient adherence and identify any potential issues that might compromise data integrity. For example, inconsistent wear patterns can lead to unreliable readings.
- Algorithm Transparency and Bias: Many smart devices use algorithms to interpret raw data. Understanding the algorithm’s limitations and potential biases is crucial for proper interpretation. Algorithms may not be equally effective across different demographics or health conditions.
Hypothetical Case Study: Smart Device Data in Diagnosis
Consider a 65-year-old male patient, Mr. Jones, presenting with complaints of increasing fatigue and shortness of breath. He is wearing a smart watch that monitors his heart rate and activity levels. His watch data shows a consistently elevated resting heart rate (averaging 100 bpm) over the past two weeks, coupled with a significant decrease in daily steps compared to his baseline.
This, combined with a physical examination revealing mild edema in his lower extremities and auscultation suggesting a possible murmur, leads the doctor to suspect heart failure. Further investigations, such as an echocardiogram, are ordered to confirm the diagnosis. The smart watch data provided an early indication, prompting earlier investigation and potentially preventing a more serious outcome.
Smart Device Data in Conjunction with Other Diagnostic Tools
Smart device data can significantly enhance the information obtained from traditional diagnostic tools. For example, a patient with suspected sleep apnea might wear a smart watch to track their sleep patterns and heart rate variability. This data, combined with a polysomnography (sleep study), provides a more comprehensive picture of the severity and characteristics of their sleep apnea, allowing for a more personalized treatment plan.
Similarly, continuous glucose monitoring data from a smart device can be integrated with HbA1c levels to provide a more nuanced understanding of a diabetic patient’s glucose control over time. This integrated approach offers a richer dataset for clinical decision-making than either method alone.
Patient Education and Engagement

Source: petra.com
Smart health devices offer incredible potential for improving health outcomes, but their effectiveness hinges on patients understanding how to use them correctly and interpreting the data responsibly. Without proper education, these devices can lead to misinterpretations, inappropriate self-treatment, and even increased anxiety. Effective patient education is therefore crucial for maximizing the benefits and minimizing the risks associated with this technology.Educating patients about the proper use and limitations of smart health devices requires a multi-faceted approach.
It’s not enough to simply hand someone a device and expect them to understand its nuances. Clear, concise communication, tailored to the individual’s health literacy level, is essential. This includes explaining the device’s functionality, its limitations, and how the data it collects should be interpreted. Equally important is highlighting potential risks and emphasizing that the data provided by these devices should complement, not replace, professional medical advice.
Strategies for Communicating Benefits and Risks of Smart Health Devices
Effective communication strategies involve a combination of methods. For example, providing short, easy-to-understand videos demonstrating how to use the device and interpret the data can be highly effective. Supplementing this with written materials, such as patient handouts (an example of which is provided below), reinforces learning and provides a reference point. Interactive workshops or online tutorials can further enhance engagement and understanding, particularly for those who learn best through hands-on experience.
Finally, incorporating real-life examples of how the device has helped others can make the information more relatable and encourage adoption.
Resources for Doctor’s Patient Education
Doctors can utilize several resources to enhance their patient education efforts. Many reputable organizations, such as the American Heart Association or the Centers for Disease Control and Prevention, offer comprehensive materials on various health conditions and the role of technology in their management. These resources often include patient-friendly brochures, videos, and online modules covering topics such as the responsible use of wearable technology for heart rate monitoring or the interpretation of sleep data from smartwatches.
Additionally, many device manufacturers provide training materials for healthcare professionals, which can be invaluable in ensuring doctors are equipped to guide their patients effectively.
Patient Handout: Accurately Using and Interpreting Data from a Smart Blood Pressure Monitor
This handout explains how to accurately use a home blood pressure monitor and understand the readings. Using Your Blood Pressure Monitor:
Doctors are divided on the reliability of smart devices for continuous health monitoring; some argue the data isn’t precise enough for diagnosis. However, early detection is key, as highlighted by the recent hospitalization of Monali Thakur, as detailed in this article monali thakur hospitalised after struggling to breathe how to prevent respiratory diseases , which underscores the importance of proactive health management.
Perhaps smart devices, combined with regular check-ups, could offer a better approach to preventative care.
1. Find a quiet place
Sit comfortably with your back supported and feet flat on the floor. Avoid talking or moving during the measurement.
2. Proper positioning
Rest your arm on a table, ensuring the cuff is at heart level.
3. Cuff placement
Place the cuff snugly around your upper arm, above the elbow, leaving about two fingers’ width of space between the cuff and your elbow.
So, are smart devices reliable for health monitoring? Doctors have mixed opinions on smart health tech, with concerns about accuracy and data privacy. The recent news that the FDA approves clinical trials for pig kidney transplants in humans highlights the need for reliable, accurate medical data – something smart devices still need to consistently deliver. Ultimately, integrating smart tech into healthcare requires careful consideration of its limitations alongside its potential benefits.
4. Inflate the cuff
Follow the device instructions to inflate the cuff.
5. Take multiple readings
Take at least three readings, spaced a minute apart, and record each reading.
6. Record your readings
Note the systolic (top) and diastolic (bottom) numbers, along with the date and time. Interpreting Your Readings:Your doctor will provide you with your target blood pressure range. Readings consistently above or below this range should be discussed with your physician. A single high or low reading doesn’t necessarily indicate a problem, but consistent readings outside your target range require medical attention.
Important Considerations:* Ensure your cuff is the correct size for your arm. An incorrectly sized cuff can lead to inaccurate readings.
- Avoid caffeine, nicotine, or strenuous exercise immediately before taking your blood pressure.
- This device is for monitoring purposes only. It does not replace regular check-ups with your doctor.
Concluding Remarks
So, are smart health devices reliable for monitoring health? The answer, as we’ve seen, is nuanced. While they offer exciting possibilities for personalized healthcare and proactive monitoring, they are not a replacement for traditional medical assessments. Doctors are cautiously optimistic, emphasizing the importance of critical data interpretation, patient education, and the ongoing need for research to improve the accuracy and reliability of these devices.
The future of smart health tech is bright, but responsible integration and a healthy dose of skepticism are crucial for maximizing its benefits and minimizing its risks.
Q&A
What are the biggest limitations of current smart health devices?
Accuracy can vary significantly depending on the device, the user, and environmental factors. Data might be affected by sensor inconsistencies, incorrect usage, and interference from external sources. They also don’t replace professional medical advice.
Can I rely solely on smart device data for diagnosis?
Absolutely not. Smart device data should be considered supplemental information, not a primary diagnostic tool. Always consult a doctor for diagnosis and treatment.
How can I ensure accurate data from my smart device?
Follow the manufacturer’s instructions carefully, ensure proper fit and placement of the device, and be mindful of potential sources of interference (e.g., strong electromagnetic fields).
Are my health data from smart devices private and secure?
Data privacy and security are crucial concerns. Read the privacy policies of your devices and apps carefully. Choose reputable brands with strong security measures.