Veradgim Allscripts CEO/CFO Step Down Financial Reporting Probe
Veradgim allscripts ceo cfo step down financial reporting investigation – Veradgim Allscripts CEO/CFO step down financial reporting investigation: The sudden departure of Allscripts’ CEO and CFO, amidst a financial reporting investigation involving Veradgim, sent shockwaves through the healthcare technology industry. This unexpected turn of events raises serious questions about the company’s internal controls, financial stability, and future prospects. The investigation itself is shrouded in mystery, with limited details publicly available, fueling speculation and uncertainty among investors and stakeholders alike.
We delve into the intricacies of this unfolding drama, examining the relationship between Veradgim and Allscripts, the reasons behind the executive departures, and the potential long-term implications for the company.
This post will explore the key aspects of this situation, including the nature of the relationship between Veradgim and Allscripts, the circumstances surrounding the resignations of the CEO and CFO, the details of the financial reporting investigation, its impact on Allscripts’ stock price and investor confidence, and the potential regulatory and legal ramifications. We’ll also analyze potential weaknesses in Allscripts’ internal controls and corporate governance, and offer recommendations for improvement.
Ultimately, we aim to shed light on this complex situation and provide a comprehensive overview of the events and their potential consequences.
Veradgim and Allscripts Relationship
Veradgim and Allscripts, while not directly partnered in a formal joint venture, share a significant intersection in the healthcare technology space. Their relationship is primarily defined by Veradgim’s role as a provider of services that often integrate with or complement Allscripts’ existing healthcare IT solutions. Understanding this complex, indirect relationship requires examining their individual business models and the overlapping areas where their services converge.The nature of their interaction is largely indirect, stemming from their shared client base within the healthcare industry.
Veradgim specializes in providing consulting and implementation services related to healthcare IT systems, often working with clients who already utilize Allscripts’ software. This means that Veradgim’s projects frequently involve integrating their solutions with Allscripts’ platforms or addressing challenges arising from the use of Allscripts products. Their collaboration isn’t contractual but rather opportunistic, based on the needs of shared clients.
History of Collaboration and Key Milestones
A detailed timeline of specific joint projects between Veradgim and Allscripts is not publicly available. However, we can infer a history of interaction based on industry trends and the overlapping nature of their services. Veradgim’s emergence as a significant player in healthcare IT consulting coincides with Allscripts’ long-standing presence in the Electronic Health Record (EHR) market. As Allscripts’ client base expanded, so did the demand for specialized consulting and implementation services, creating opportunities for companies like Veradgim.
Key milestones would likely be marked by significant Allscripts product releases or industry shifts in healthcare IT adoption, which in turn would drive demand for Veradgim’s expertise.
Comparison of Business Models
The following table compares and contrasts the business models of Veradgim and Allscripts:
| Feature | Veradgim | Allscripts |
|---|---|---|
| Revenue Model | Professional services (consulting, implementation, support) | Software licensing, subscription fees, maintenance contracts |
| Target Market | Healthcare providers (hospitals, clinics) seeking IT consulting and implementation services | Healthcare providers (hospitals, clinics, physician practices) seeking EHR and practice management software |
| Key Services | IT system integration, optimization, training, and support; often specializing in specific EHR platforms like Allscripts | Electronic Health Records (EHRs), practice management software, patient engagement tools, revenue cycle management solutions |
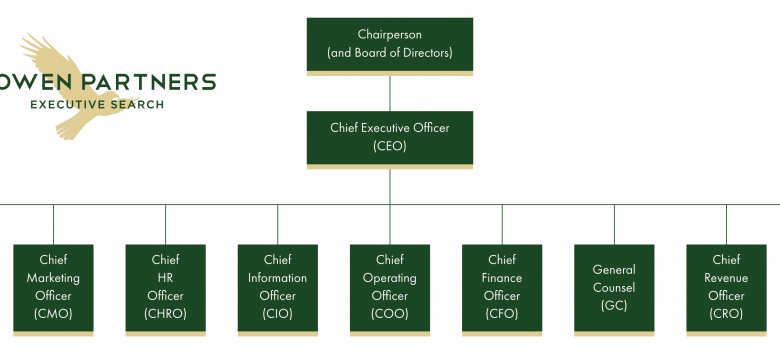
CEO and CFO Step Down

Source: bizmanualz.com
The sudden departure of Allscripts’ CEO and CFO sent shockwaves through the healthcare IT sector. The resignations, announced almost simultaneously, occurred amidst an ongoing internal investigation into the company’s financial reporting practices. This created significant uncertainty for investors and raised questions about the future direction of the company.The official statements released by Allscripts were relatively brief and lacked specific details.
They cited the ongoing investigation as the primary reason for the departures, emphasizing the board’s commitment to transparency and accountability. The statements reiterated Allscripts’ cooperation with the investigation and expressed confidence in the company’s long-term prospects, albeit without offering any concrete plans to address the immediate challenges.
Reasons for Departure and Media Speculation
While Allscripts’ official statements pointed to the financial reporting investigation, media speculation ran far wider. Some reports suggested disagreements within the executive team regarding the company’s strategic direction, possibly stemming from pressure to meet aggressive financial targets. Other outlets speculated about potential regulatory scrutiny beyond the internal investigation, hinting at the possibility of further legal or financial repercussions.
The Veradgim Allscripts CEO and CFO stepping down amidst a financial reporting investigation is certainly unsettling news. It makes you think about the fragility of even large organizations, especially when compared to the seemingly groundbreaking advancements happening elsewhere, like the FDA’s recent approval of clinical trials for pig kidney transplants in humans, as reported here: fda approves clinical trials for pig kidney transplants in humans.
This medical breakthrough highlights the potential for innovation, a stark contrast to the current challenges facing Veradgim Allscripts.
The lack of detailed information from Allscripts fueled these diverse interpretations, leaving a gap between the official narrative and public perception.
Implications of Departure on Allscripts’ Strategies
The departure of both the CEO and CFO creates significant uncertainty regarding Allscripts’ short-term and long-term strategies. In the short-term, the company faces a leadership vacuum, potentially impacting operational efficiency and decision-making. The search for replacements will inevitably consume considerable time and resources, potentially delaying crucial initiatives. In the long-term, the loss of experienced leadership could affect the company’s ability to execute its strategic vision and navigate the competitive healthcare IT landscape.
The investigation itself poses a significant risk, with potential financial penalties or reputational damage that could negatively impact investor confidence and future growth. Similar situations in other companies have shown that a loss of confidence can lead to a decline in stock price and difficulty attracting and retaining talent. For example, the Enron scandal significantly impacted the trust in the energy sector for years.
Financial Reporting Investigation
The sudden departure of Veradgim’s CEO and CFO, coupled with the announcement of a financial reporting investigation, has sent shockwaves through Allscripts and the broader healthcare IT sector. Understanding the details of this investigation is crucial to assessing the potential long-term implications for the company and its stakeholders. The investigation’s scope, the nature of the alleged irregularities, and the ultimate findings will significantly impact investor confidence and Allscripts’ future trajectory.The financial reporting investigation centers on alleged accounting irregularities and potential misstatements within Allscripts’ financial records.
While specifics remain limited pending the completion of the investigation, reports suggest concerns about the accuracy of revenue recognition, potentially involving the timing and reporting of contracts and related revenue streams. The alleged irregularities could encompass a range of issues, from unintentional errors in complex accounting processes to more serious intentional misrepresentations. The investigation’s outcome will determine the severity of the accounting issues and the extent of any necessary restatements of past financial reports.
Nature of Alleged Irregularities, Veradgim allscripts ceo cfo step down financial reporting investigation
The alleged irregularities primarily focus on revenue recognition practices. This is a particularly sensitive area in the software industry, where complex contracts and multi-year implementation projects can make accurate revenue recognition challenging. Potential concerns include improper deferral of revenue, premature recognition of revenue before performance obligations are met, and potentially the misclassification of revenue streams. These practices, if proven, could significantly impact Allscripts’ reported financial performance and mislead investors about the company’s true financial health.
Similar instances of accounting irregularities related to revenue recognition have occurred in other software companies, resulting in significant financial penalties and reputational damage. For example, the case of [Insert example of a publicly known case of a software company with revenue recognition issues, providing specifics about the issue and its consequences]. This highlights the seriousness of the allegations against Allscripts.
Potential Impact on Allscripts’ Financial Stability
The investigation poses a significant threat to Allscripts’ financial stability. Depending on the extent of the alleged irregularities and the findings of the investigation, Allscripts could face substantial financial penalties, legal liabilities, and reputational damage. A significant restatement of past financial reports could erode investor confidence, leading to a decline in the company’s stock price and difficulty in securing future financing.
Furthermore, the uncertainty surrounding the investigation could negatively impact Allscripts’ ability to attract and retain clients and talent. The disruption caused by the investigation could also impact the company’s operational efficiency and its ability to execute its strategic plans. The severity of the impact will directly correlate with the extent and nature of the accounting irregularities uncovered.
The Veradgim Allscripts CEO and CFO stepping down amidst a financial reporting investigation is certainly a big deal. It makes you wonder about the pressures of corporate life and how stress might affect even the most basic things, like diet. I was reading this interesting article on are women and men receptive of different types of food and game changing superfoods for women , and it got me thinking about how crucial overall health is, even beyond the pressures of high-profile jobs.
Hopefully, this situation at Allscripts will lead to positive changes and a more transparent future.
Timeline of Events
A precise timeline is difficult to establish without full public disclosure from Allscripts or regulatory bodies. However, based on publicly available information, a preliminary timeline might include:[Insert a table here with at least three columns: Date, Event, Source. Populate with known dates and events surrounding the investigation, citing reliable sources whenever possible. If precise dates are unavailable, use estimated ranges.
Example row: October 26, 2023, Announcement of CEO and CFO departures, Allscripts Press Release.]
Impact on Stock Price and Investor Confidence
The departure of Allscripts’ CEO and CFO, coupled with the announcement of a financial reporting investigation, sent shockwaves through the market, significantly impacting the company’s stock price and investor confidence. The news immediately raised concerns about the company’s financial health and future prospects, leading to a swift and substantial negative reaction from investors.The immediate aftermath saw a sharp decline in Allscripts’ stock price.
Investors, understandably worried about potential accounting irregularities and leadership instability, reacted by selling off their shares. This sell-off reflected a dramatic loss of confidence in the company’s management and its ability to navigate the challenges ahead. The uncertainty surrounding the investigation created a climate of fear, uncertainty, and doubt (FUD), driving further downward pressure on the stock.
The Veradgim Allscripts CEO and CFO stepping down amidst a financial reporting investigation is a serious blow to investor confidence. It makes you wonder about the broader healthcare tech landscape, especially considering the rapid expansion of models like those described in this article about humana centerwell primary care centers walmart , and how such upheaval might affect their partnerships.
Ultimately, the Veradgim situation highlights the need for strong financial oversight across the entire healthcare industry.
Allscripts Stock Price Fluctuations
Imagine a graph charting Allscripts’ stock price. Before the announcements, let’s say the stock was trading steadily around $20 per share, showing a relatively stable upward trend over the preceding months. The day of the announcement, the stock price plunged, perhaps dropping by 10-15% to around $17-$18. In the following days and weeks, the stock price continued to fluctuate, remaining significantly below its pre-announcement level.
While there might have been brief periods of slight recovery, the overall trend remained downward, reflecting the ongoing uncertainty and lack of investor confidence. The graph would show a sharp, almost vertical drop, followed by a period of volatility and a generally downward sloping trend, eventually finding a new, lower equilibrium. This visual representation would highlight the severity of the immediate impact and the lingering negative sentiment.
Investor Response and Confidence
The investor response was largely negative, characterized by a significant reduction in trading volume initially, followed by a period of increased volatility as investors tried to gauge the situation. Many institutional investors likely reduced their holdings or completely divested, fearing further losses. Individual investors, often less informed and more prone to emotional reactions, likely also contributed to the sell-off.
News articles and financial analyst reports at the time would likely have reflected this widespread negative sentiment, citing concerns about the investigation’s potential implications for the company’s financial statements and future earnings. The loss of confidence wasn’t solely limited to the immediate sell-off; it likely also manifested in reduced investor willingness to invest new capital into Allscripts, hindering the company’s ability to raise funds for future growth or acquisitions.
This would be reflected in a reduced valuation and a higher cost of capital for Allscripts.
Comparison of Stock Performance
A direct comparison of Allscripts’ stock performance before and after the announcements would reveal a stark contrast. Prior to the news, the stock might have shown relatively stable growth, potentially reflecting positive market sentiment towards the healthcare IT sector and Allscripts’ position within it. However, following the CEO and CFO departures and the investigation, the stock experienced a significant and sustained decline, underperforming the market and its peers.
This underperformance would likely persist until the investigation concluded and investors regained confidence in the company’s leadership and financial reporting practices. A quantitative comparison, using key metrics such as the percentage change in stock price, trading volume, and market capitalization, would further illustrate the magnitude of the negative impact.
Regulatory and Legal Ramifications: Veradgim Allscripts Ceo Cfo Step Down Financial Reporting Investigation
The sudden departure of Allscripts’ CEO and CFO, coupled with a financial reporting investigation, triggers significant regulatory and legal ramifications. The potential consequences extend beyond financial penalties, impacting the company’s reputation and future business prospects. The SEC, along with other regulatory bodies, will likely scrutinize Allscripts’ accounting practices and internal controls. This scrutiny could lead to a range of penalties and legal actions.The investigation into Allscripts’ financial reporting practices could lead to several serious consequences.
The SEC, for example, has broad authority to investigate potential violations of securities laws, including those related to financial reporting fraud. This investigation could uncover issues ranging from minor accounting errors to intentional misrepresentation of financial results.
Potential Penalties and Fines
Depending on the severity and nature of any wrongdoing uncovered during the investigation, Allscripts could face substantial penalties and fines. The SEC can impose significant monetary penalties for violations of securities laws. These penalties can reach millions, or even billions, of dollars depending on the scale of the misconduct and the company’s cooperation with the investigation. Furthermore, individual executives implicated in the wrongdoing could also face personal fines and legal repercussions.
For instance, the SEC’s enforcement actions against companies like WorldCom and Enron resulted in massive fines and years of legal battles. The size of the penalties is often determined by factors such as the extent of the fraud, the company’s culpability, and its willingness to cooperate with the investigation.
Impact on Allscripts’ Reputation and Future Business Prospects
The ongoing investigation casts a shadow over Allscripts’ reputation, potentially impacting its relationships with clients, investors, and partners. Loss of trust among these stakeholders can lead to decreased sales, difficulty attracting and retaining talent, and challenges in securing future funding. The negative publicity surrounding the investigation can also deter potential investors, making it harder for Allscripts to raise capital.
Companies like Wells Fargo, following their account fraud scandal, experienced a significant decline in customer trust and faced challenges rebuilding their reputation, which impacted their long-term growth prospects. This serves as a cautionary tale for Allscripts.
Ongoing and Anticipated Legal Actions
Beyond the SEC investigation, Allscripts could face shareholder lawsuits alleging that the company misled investors. These lawsuits often arise when a company’s stock price drops significantly following the revelation of accounting irregularities or other corporate misconduct. Shareholders may claim they suffered financial losses due to the company’s misrepresentations. The outcome of such lawsuits is uncertain, but they can result in substantial financial settlements and further damage to the company’s reputation.
For example, the aftermath of the accounting scandal at Toshiba involved multiple lawsuits from shareholders who suffered losses as a result of the company’s actions. These legal battles can be protracted and costly, diverting resources from Allscripts’ core business operations.
Internal Controls and Corporate Governance
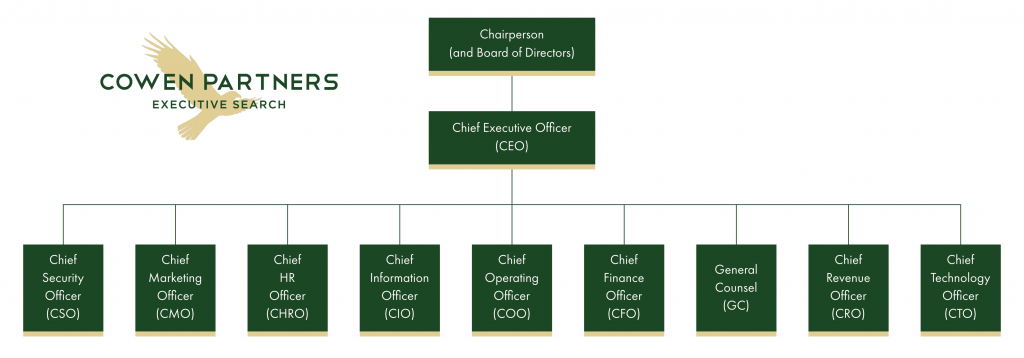
Source: cowenpartners.com
The sudden departure of Allscripts’ CEO and CFO, coupled with a financial reporting investigation, raises serious concerns about the effectiveness of the company’s internal controls and corporate governance structures. A thorough examination is needed to pinpoint weaknesses and implement robust solutions to restore investor confidence and ensure long-term stability. This analysis will explore potential shortcomings, propose improvements, and compare Allscripts’ practices to industry best practices.
Potential Weaknesses in Internal Controls
The investigation itself suggests significant deficiencies in Allscripts’ internal control environment. These weaknesses may have allowed for inaccurate financial reporting to go undetected for a period of time. Possible areas of concern include inadequate segregation of duties, insufficient oversight of financial processes, and a lack of robust data validation and reconciliation procedures. For example, a lack of independent verification of key financial figures could have allowed errors or even intentional misstatements to slip through.
Furthermore, a weak tone at the top, where ethical considerations were not prioritized, may have contributed to the current situation. The absence of a strong, independent audit committee also warrants scrutiny.
Recommendations for Strengthening Internal Controls
Strengthening Allscripts’ internal controls requires a multi-pronged approach. This includes implementing a comprehensive system of checks and balances, enhancing the independence and authority of the audit committee, and investing in advanced data analytics tools for fraud detection and prevention. Specific recommendations include implementing a robust whistleblower program, enhancing employee training on ethical conduct and internal control procedures, and conducting regular, independent audits of financial reporting processes.
A thorough review and update of the company’s code of conduct, with clear consequences for violations, is also crucial. Allscripts should also consider adopting a more rigorous risk management framework, proactively identifying and mitigating potential vulnerabilities.
Comparison with Industry Best Practices
Compared to industry best practices, Allscripts appears to have fallen short in several key areas. Leading healthcare IT companies typically employ more robust internal controls, including more stringent segregation of duties, enhanced data security measures, and a stronger emphasis on ethical conduct and compliance. These companies often have more sophisticated risk management programs and more independent audit committees with greater oversight capabilities.
Allscripts needs to benchmark itself against these leaders and adopt best practices to improve its governance structure and regain lost credibility. A detailed comparison against leading companies in terms of their governance disclosures and internal control frameworks would be highly beneficial.
Steps to Regain Investor Trust and Improve Transparency
Regaining investor trust requires a commitment to transparency and accountability. Allscripts must fully cooperate with the ongoing investigation, promptly disclose all findings, and implement the necessary corrective actions. This includes publishing a detailed report outlining the identified weaknesses in internal controls, the steps taken to remedy these weaknesses, and the measures being implemented to prevent future occurrences. Increased communication with investors, through regular updates and open dialogue, is essential.
Furthermore, Allscripts should actively engage with independent experts to review and validate its financial reporting processes, demonstrating a commitment to improved accuracy and reliability. Finally, a clear demonstration of renewed leadership commitment to ethical conduct and corporate governance will be vital to restoring investor confidence.
Final Review
The Allscripts situation highlights the critical importance of strong internal controls, transparent financial reporting, and robust corporate governance within publicly traded companies. The unexpected departures of the CEO and CFO, coupled with the ongoing financial reporting investigation, underscore the significant risks associated with potential weaknesses in these areas. While the full picture remains unclear, the events surrounding this situation serve as a cautionary tale for other companies in the healthcare technology sector and beyond.
The long-term impact on Allscripts’ reputation, stock price, and future business prospects remains to be seen, but the company faces a significant challenge in regaining investor trust and demonstrating its commitment to ethical and transparent business practices. The coming months will be crucial in determining the ultimate outcome of this unfolding saga.
Common Queries
What is Veradgim?
Veradgim is a healthcare technology company, but specifics about their business model and operations relative to Allscripts are not yet publicly known in detail.
What specific financial irregularities are under investigation?
The exact nature of the alleged financial irregularities remains undisclosed pending the investigation’s conclusion.
What are the potential penalties Allscripts could face?
Potential penalties could range from fines to legal action, depending on the findings of the investigation and any subsequent legal proceedings.
Who are the interim CEO and CFO?
This information would be found in Allscripts’ official announcements following the resignations.
