FTC OCR warns telehealth companies hospitals online trackers
FTC OCR warns telehealth companies hospitals online trackers – Whoa, that’s a mouthful, right? But it’s a seriously important topic. We’re talking about the growing concerns around patient privacy and data security in the booming telehealth industry. The Federal Trade Commission (FTC) and the Office for Civil Rights (OCR) are cracking down, sending warnings to telehealth providers and hospitals about the potentially illegal use of online trackers.
This post dives into the details, exploring the legal implications, patient rights, and steps everyone needs to take to ensure compliance.
The implications are huge. We’ll examine specific examples of how online trackers – from cookies to device IDs – are collecting sensitive patient data, often without proper consent. We’ll also look at the roles and responsibilities of both telehealth companies and hospitals in safeguarding this information, exploring the potential legal ramifications of non-compliance, including hefty fines and reputational damage.
Think HIPAA violations, data breaches, and the erosion of patient trust – it’s a complex landscape.
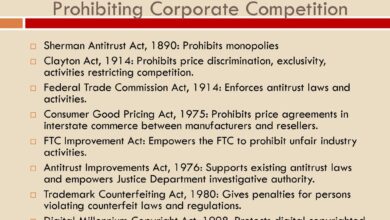
FTC OCR Warnings
Source: freebiesupply.com
The Federal Trade Commission (FTC) and the Office for Civil Rights (OCR) have issued warnings to telehealth companies regarding their data privacy and security practices, particularly concerning the use of online trackers. These warnings highlight significant concerns about the potential for violations of HIPAA and other privacy laws, emphasizing the need for robust data protection measures within the telehealth industry.
The agencies have made it clear that non-compliance will result in serious consequences.
FTC and OCR Concerns Regarding Telehealth Data Practices
The FTC and OCR’s concerns center on the collection, use, and disclosure of protected health information (PHI) by telehealth companies, especially in conjunction with the use of third-party online trackers. These trackers, often embedded in websites and apps, collect data about user activity, which can include sensitive information indirectly linked to PHI. The agencies are particularly concerned about the lack of transparency regarding data collection practices, the inadequate security measures implemented to protect collected data, and the potential for unauthorized disclosure or misuse of PHI.
The warnings underscore the importance of obtaining informed consent from patients and ensuring compliance with all relevant privacy regulations.
The FTC OCR’s warning to telehealth companies and hospitals about online trackers highlights the importance of patient data privacy, especially concerning sensitive health information. This makes me think of Monali Thakur’s recent hospitalization, as reported in this article monali thakur hospitalised after struggling to breathe how to prevent respiratory diseases , underscoring the need for proactive respiratory health management.
Ultimately, responsible data handling and preventative healthcare are crucial for both individual well-being and maintaining public trust in the healthcare system, which is what the FTC warning aims to protect.
Potential Violations of Privacy and Security Laws
Telehealth companies failing to adequately protect patient data risk violating several key privacy and security laws. These include the Health Insurance Portability and Accountability Act (HIPAA), which sets stringent standards for the privacy and security of PHI, and state laws that may offer additional protections. Violations can lead to significant penalties, including hefty fines, legal action, and reputational damage.
The FTC can also pursue enforcement actions for violations of the FTC Act, which prohibits unfair or deceptive acts or practices, including those that involve the deceptive collection or use of consumer data.
Examples of Telehealth Practices Triggering FTC/OCR Scrutiny
Several telehealth practices might attract FTC/OCR scrutiny. For instance, using online trackers without obtaining explicit consent from patients, failing to implement appropriate security measures to protect data from unauthorized access or breaches, sharing patient data with third-party vendors without proper authorization, and failing to provide clear and accessible privacy policies are all potential red flags. The use of insecure data storage methods, inadequate employee training on data security protocols, and a lack of procedures for responding to data breaches also pose significant risks.
Hypothetical Scenario: Non-Compliant Telehealth Data Practices
Imagine a telehealth company, “HealthConnect,” that uses a third-party analytics platform to track user behavior on its website and mobile app. This platform collects data on patient visits, diagnoses, and treatment plans, potentially identifying individuals through IP addresses or other indirect identifiers. HealthConnect fails to obtain explicit consent from patients for this data collection, does not inform patients about the types of data collected or how it’s used, and does not implement sufficient security measures to protect the data from unauthorized access.
This scenario clearly demonstrates a non-compliant approach to data handling, potentially violating HIPAA and other privacy regulations, and leaving HealthConnect vulnerable to substantial penalties and reputational harm. A data breach revealing this information could result in significant legal repercussions and loss of patient trust.
Online Trackers in Telehealth
The increasing reliance on telehealth platforms has raised significant concerns about patient privacy. The use of online trackers within these platforms presents a complex challenge, demanding careful consideration of the data collected, the potential risks, and the existing legal frameworks designed to protect sensitive health information. Understanding these trackers and their implications is crucial for both telehealth providers and patients.
Types of Online Trackers and Data Collection Methods
Telehealth platforms utilize various online trackers to gather data on user behavior and preferences. These trackers operate through different methods, each with varying degrees of intrusiveness. Common examples include cookies, which store small pieces of data on a user’s device; pixels, tiny images that track website visits; and device IDs, unique identifiers assigned to individual devices. These trackers collect data such as IP addresses, browsing history, and the specific pages visited within the telehealth platform.
More sophisticated trackers may even collect data on user interactions within the platform, such as the duration of video calls or the specific features used.
Privacy Risks Associated with Different Tracker Technologies
The privacy risks associated with online trackers in telehealth vary depending on the type of tracker and the data collected. Cookies, while relatively low-risk in isolation, can be combined with other data to create a detailed profile of a user’s online activity, potentially revealing sensitive health information. Pixels, often used for advertising purposes, can track a user’s movement across multiple websites, creating a comprehensive picture of their interests and behavior, including potential health concerns.
Device IDs, while seemingly anonymous, can be linked to other data points to identify individual users, potentially compromising their privacy. The aggregation of data from multiple trackers poses the greatest risk, allowing for the creation of highly detailed and potentially sensitive user profiles.
Legal Frameworks Governing Tracker Use in Telehealth
The use of online trackers in telehealth is subject to various legal frameworks, most notably the Health Insurance Portability and Accountability Act (HIPAA) in the United States. HIPAA regulations mandate the protection of Protected Health Information (PHI), which includes data collected through telehealth platforms. The use of trackers must comply with HIPAA’s requirements for data security, privacy, and patient consent.
Failure to comply with HIPAA can result in significant fines and legal repercussions. Other relevant regulations, depending on jurisdiction, may include GDPR (General Data Protection Regulation) in Europe and similar data protection laws in other countries. These regulations generally require transparency about data collection practices and obtain explicit consent from users before collecting and processing their data.
Comparison of Data Collected and Associated Privacy Risks
| Tracker Type | Data Collected | Privacy Risks | HIPAA Compliance Considerations |
|---|---|---|---|
| Cookies | Website visits, browsing history, preferences | Potential for de-anonymization when combined with other data; tracking of health-related searches | Requires clear notice and consent if collecting PHI; robust security measures needed |
| Pixels | Website visits, user interactions, ad targeting data | Tracking across multiple websites, creating comprehensive profiles; potential for revealing health information indirectly | Requires careful consideration of data collected and its potential link to PHI; consent may be required |
| Device IDs | Unique device identifier | Potential for re-identification of users if linked to other data; tracking across multiple platforms | Requires appropriate de-identification or anonymization techniques if used to identify individuals; strict security measures |
Hospitals’ Role in Telehealth Data Security
The increasing reliance on telehealth has brought significant benefits to healthcare delivery, but it has also amplified concerns about patient data security. Hospitals, as key players in this evolving landscape, bear a substantial responsibility for protecting sensitive patient information shared through telehealth platforms. Failure to do so can lead to serious legal and reputational consequences. This section will explore the specific responsibilities of hospitals in securing telehealth data, potential liabilities, and best practices for compliance.Hospitals partnering with telehealth companies share joint responsibility for protecting patient data.
This shared responsibility necessitates clear contractual agreements outlining data security protocols, breach notification procedures, and liability allocation. The hospital must ensure the telehealth vendor adheres to stringent data privacy and security standards, such as HIPAA, and conducts regular security audits of the vendor’s systems. Furthermore, hospitals must establish robust internal processes to oversee the security of data exchanged through telehealth platforms, including access control, encryption, and data loss prevention measures.
Hospital Liabilities for Inadequate Data Security
Hospitals face significant liabilities if they fail to adequately safeguard patient information shared through telehealth platforms. These liabilities can include hefty fines from regulatory bodies like the Office for Civil Rights (OCR) under HIPAA, costly lawsuits from patients whose data has been compromised, and reputational damage leading to loss of patient trust and business. For instance, a hospital failing to encrypt data transmitted through a telehealth platform and experiencing a data breach could face millions of dollars in fines and legal fees.
The severity of the penalties will depend on the nature and extent of the breach, as well as the hospital’s demonstrated efforts (or lack thereof) to protect patient data.
Best Practices for Data Privacy Compliance in Telehealth Collaborations
Implementing robust data security protocols is crucial for hospitals collaborating with telehealth companies. This involves several key steps:
A comprehensive approach is necessary to ensure compliance. This includes thorough risk assessments, employee training, and regular security audits.
- Conduct regular risk assessments: Identify vulnerabilities and potential threats to telehealth data security.
- Implement strong access controls: Restrict access to patient data based on the principle of least privilege.
- Utilize robust encryption: Encrypt data both in transit and at rest to protect against unauthorized access.
- Establish a robust breach notification plan: Define procedures for promptly notifying patients and regulatory bodies in the event of a data breach.
- Provide comprehensive employee training: Educate staff on data security policies and procedures.
- Regularly audit security controls: Conduct periodic assessments to ensure the effectiveness of security measures.
- Maintain thorough documentation: Document all security policies, procedures, and audits for compliance purposes.
Implementing a Robust Data Security Protocol for Telehealth Integration
A robust data security protocol requires a multi-faceted approach. This goes beyond simply choosing a secure telehealth platform; it demands proactive management and ongoing vigilance.
The following points Artikel a practical implementation strategy:
- Select HIPAA-compliant telehealth vendors: Ensure vendors undergo rigorous security assessments and maintain robust security practices.
- Implement multi-factor authentication (MFA): Enhance access control by requiring multiple forms of authentication for accessing patient data.
- Utilize data loss prevention (DLP) tools: Prevent sensitive data from leaving the hospital’s network without authorization.
- Regularly update software and security patches: Address vulnerabilities promptly to minimize the risk of exploitation.
- Conduct penetration testing and vulnerability assessments: Simulate attacks to identify weaknesses in the security infrastructure.
- Establish incident response plan: Develop a detailed plan to handle data breaches and other security incidents.
- Contractual agreements: Include strong data security clauses in contracts with telehealth vendors, clearly defining responsibilities and liabilities.
Patient Rights and Informed Consent
The recent FTC OCR warnings highlight the critical need for telehealth providers to prioritize patient rights and obtain valid informed consent regarding data collection practices. Failing to do so can lead to significant legal and reputational damage. Transparency and respect for patient autonomy are paramount in building trust and ensuring ethical data handling.Informed consent in the context of telehealth data collection means patients must be fully aware of how their data will be used, shared, and protected before agreeing to its collection.
This goes beyond simply checking a box; it necessitates a clear and understandable explanation of the platform’s data practices. This includes the types of data collected, the purpose of collection, who will have access to it, and the security measures in place to protect it.
Obtaining and Documenting Valid Patient Consent
Telehealth companies should obtain informed consent through a process that ensures comprehension and voluntary agreement. This involves providing patients with accessible and understandable information about data collection practices, in a language they understand, before asking them to consent. Documentation of this consent is crucial; it should include the date, method of consent (e.g., electronic signature, verbal confirmation documented in the patient record), and a clear statement that the patient understood and agreed to the data collection practices.
The FTC OCR’s warning to telehealth companies and hospitals about online trackers got me thinking about patient data security and the overall healthcare system. It’s crucial to ensure robust privacy measures, especially with initiatives like the new cms launches primary care medicare model aco , which will handle a massive amount of sensitive patient information. This new model, while aiming to improve care, also highlights the urgent need for stronger data protection protocols to prevent misuse of the data collected by telehealth and hospital systems.
The documentation should be readily available and easily accessible to the patient upon request. Maintaining a secure and auditable record of consent is paramount.
Examples of Clear and Concise Language for Informing Patients
Instead of complex legal jargon, use plain language that patients can easily understand. For example, instead of saying “We may utilize your protected health information for treatment, payment, and healthcare operations,” try “We will use your health information to provide you with care, bill your insurance, and improve our services.” Avoid technical terms; explain concepts simply. A good example is replacing “de-identification” with “removing identifying information like your name and address.” The goal is to ensure patients understand the implications of their consent.
Sample Informed Consent Form, FTC OCR warns telehealth companies hospitals online trackers
This sample form illustrates key elements. Remember, legal requirements vary by jurisdiction; consult with legal counsel to ensure compliance.
Telehealth Platform Data Collection Consent Form
Patient Name: [Patient Name]
Date: [Date]
Platform Name: [Platform Name]Information Collection: We collect information necessary to provide you with telehealth services. This may include personal information (name, address, date of birth), health information (medical history, diagnoses, test results), and usage data (dates and times of sessions, types of services used).
Purpose of Collection: We use this information to provide you with care, manage your account, bill your insurance, improve our services, and comply with legal requirements.
Data Sharing: We may share your information with trusted third-party service providers (e.g., billing companies, data storage providers) who assist us in providing services. We will only share the minimum necessary information.
Data Security: We employ robust security measures to protect your information from unauthorized access, use, or disclosure. These measures include [List specific security measures, e.g., encryption, access controls].
Your Rights: You have the right to access, correct, and request deletion of your data. You can withdraw your consent at any time, although this may affect your ability to use our services.
Consent: By checking the box below, I acknowledge that I have read and understand this consent form and voluntarily consent to the collection, use, and sharing of my information as described above.
[ ] I consent.
Patient Signature: [Signature]
Printed Name: [Printed Name]The FTC and OCR are cracking down on telehealth companies and hospitals using online trackers, rightfully raising concerns about patient privacy. This news comes at a time of significant leadership change, as you may have heard about the retirement of AdventHealth CEO Terry Shaw, reported here: adventhealth ceo retire terry shaw. The implications of these regulatory actions are far-reaching, especially for large healthcare systems undergoing transitions like AdventHealth.
It’s a reminder that data security needs to be a top priority, regardless of leadership changes.
Enforcement and Compliance Strategies
Navigating the complex landscape of telehealth data privacy and security requires a proactive approach to compliance. Failure to adhere to regulations set by the Federal Trade Commission (FTC) and the Office for Civil Rights (OCR) can lead to significant consequences for telehealth companies and hospitals alike. Understanding potential penalties and implementing robust compliance strategies are crucial for protecting patient data and avoiding costly repercussions.The FTC and OCR wield considerable power to enforce compliance with HIPAA and other relevant privacy laws.
Non-compliance can result in a range of penalties, depending on the severity and nature of the violation.
Potential Penalties for Non-Compliance
Penalties for non-compliance can be substantial and far-reaching. The FTC can impose significant civil penalties, including monetary fines. These fines can vary widely depending on factors such as the nature of the violation, the number of individuals affected, and the company’s history of compliance. In addition to monetary penalties, the FTC can also issue cease-and-desist orders, requiring companies to stop engaging in unlawful practices.
OCR, under HIPAA, can levy even more significant penalties, ranging from warnings and corrective action plans to substantial monetary penalties per violation. For example, a failure to properly secure patient data leading to a data breach could result in penalties in the hundreds of thousands or even millions of dollars. Furthermore, reputational damage and loss of patient trust can be equally, if not more, devastating.
Strategies for Ensuring Ongoing Compliance
Maintaining ongoing compliance requires a multi-faceted approach. This includes implementing robust data security measures, such as encryption, access controls, and regular security audits. Telehealth companies and hospitals should develop and implement comprehensive data privacy policies that are readily accessible to employees and patients. Regular employee training on data privacy and security best practices is also crucial. Staying updated on evolving regulations and best practices is essential, necessitating participation in relevant conferences, webinars, and continuous professional development opportunities.
Furthermore, regular risk assessments can identify vulnerabilities and help prioritize security investments. Proactive monitoring and detection systems can help quickly identify and address potential data breaches.
The Role of Audits and Internal Reviews
Regular audits and internal reviews play a vital role in maintaining data security and privacy. These assessments provide a systematic way to evaluate the effectiveness of existing security measures and identify areas for improvement. Internal audits should be conducted by independent personnel or external consultants to ensure objectivity. These reviews should cover all aspects of data handling, from data collection and storage to data transmission and disposal.
Findings from audits should be documented and used to develop corrective action plans. The results of these audits should also be reported to senior management to demonstrate commitment to compliance.
Checklist for Mitigating FTC/OCR Investigation Risks
A proactive approach to data security and privacy can significantly reduce the risk of an FTC or OCR investigation. Telehealth companies should take the following actions:
- Implement a comprehensive data security and privacy policy that aligns with HIPAA and other relevant regulations.
- Conduct regular security risk assessments and penetration testing to identify vulnerabilities.
- Establish robust data access controls and authentication mechanisms.
- Encrypt all sensitive patient data both in transit and at rest.
- Provide regular employee training on data privacy and security best practices.
- Implement a data breach response plan and regularly test its effectiveness.
- Maintain detailed records of all data processing activities.
- Conduct regular audits and internal reviews to assess compliance.
- Establish a process for handling patient complaints and data breach notifications.
- Develop a system for promptly investigating and addressing security incidents.
Future of Telehealth Data Privacy
The rapid expansion of telehealth has brought unprecedented benefits to healthcare access and delivery. However, this growth has also highlighted significant vulnerabilities in protecting patient data. The future of telehealth data privacy hinges on proactively addressing these challenges through technological innovation, robust regulation, and a collaborative approach involving stakeholders across the healthcare ecosystem. This requires a multifaceted strategy that anticipates emerging threats and capitalizes on opportunities presented by new technologies.The increasing reliance on interconnected devices and artificial intelligence (AI) in telehealth presents both opportunities and challenges for data privacy.
Emerging technologies like blockchain, federated learning, and differential privacy offer innovative solutions to enhance security and anonymization, but their implementation requires careful consideration of ethical and practical implications. Furthermore, the cross-border exchange of health data, a common feature of global telehealth initiatives, necessitates harmonization of data protection regulations across jurisdictions.
Emerging Technologies and Their Impact
AI-powered diagnostic tools and remote patient monitoring devices collect vast amounts of sensitive health data. While these technologies improve healthcare efficiency, they also expand the attack surface for cybercriminals. Blockchain technology, with its decentralized and immutable ledger, offers a potential solution for secure data storage and sharing, enhancing transparency and accountability. Federated learning allows for collaborative AI model training without directly sharing sensitive patient data, preserving privacy while improving the accuracy of diagnostic algorithms.
Differential privacy techniques add carefully calibrated noise to datasets, making it difficult to identify individual patients while still allowing for valuable aggregate analysis. The successful integration of these technologies depends on robust cybersecurity measures and interoperability standards.
Challenges and Opportunities in Regulating Data Privacy
The dynamic nature of telehealth poses significant challenges for regulators. Keeping pace with technological advancements and ensuring consistent data protection across various platforms and jurisdictions is crucial. Harmonizing international data privacy regulations is essential for facilitating cross-border telehealth services while maintaining high standards of patient data protection. Balancing the need for data sharing for research and public health initiatives with individual privacy rights requires careful consideration and transparent mechanisms for consent and data governance.
Opportunities exist to develop more flexible and adaptable regulatory frameworks that leverage technological advancements to enhance data security and accountability. For example, incorporating principles of privacy by design into the development of telehealth applications can prevent privacy breaches from the outset.
Innovative Approaches to Data Anonymization and Security
Data anonymization techniques are crucial for protecting patient privacy while enabling valuable data analysis. Homomorphic encryption allows computations to be performed on encrypted data without decryption, ensuring confidentiality. Differential privacy, as mentioned earlier, adds noise to data to protect individual identities while preserving statistical utility. Furthermore, advanced access control mechanisms and multi-factor authentication can enhance the security of telehealth platforms.
Implementing robust data encryption both in transit and at rest is paramount. Regular security audits and penetration testing are essential to identify and address vulnerabilities proactively. The adoption of zero-trust security models, which assume no implicit trust within a network, is increasingly important in the telehealth context.
The Role of Industry Self-Regulation
While government regulation provides a necessary framework, industry self-regulation plays a vital role in fostering a culture of data privacy and security within the telehealth sector. Industry bodies can develop and enforce best practices, promote the adoption of security standards, and establish mechanisms for accountability. The creation of industry-wide codes of conduct and ethical guidelines can incentivize companies to prioritize data privacy and build trust with patients.
Transparent reporting mechanisms for data breaches and security incidents can enhance accountability and facilitate learning from past mistakes. Collaborative efforts between industry stakeholders, including telehealth providers, technology developers, and patient advocacy groups, are crucial for establishing effective self-regulatory mechanisms. This collaborative approach can lead to the development of innovative solutions and the establishment of a culture of responsible data handling within the telehealth industry.
Closing Notes: FTC OCR Warns Telehealth Companies Hospitals Online Trackers

Source: govhealthit.com
The FTC and OCR warnings serve as a stark reminder: the digital age demands vigilance in protecting patient data. Telehealth offers incredible opportunities for healthcare access, but it comes with serious responsibilities. Ignoring data privacy and security is not an option. By understanding the regulations, implementing robust security protocols, and prioritizing informed consent, telehealth companies and hospitals can navigate this complex landscape and ensure the ethical and legal use of patient data.
The future of telehealth depends on it.
FAQ Resource
What types of online trackers are most concerning in telehealth?
Cookies, pixels, device IDs, and other tracking technologies that collect data about patient visits, health information, and browsing habits are of significant concern. These can be used to create detailed profiles without the patient’s knowledge or consent.
What are the potential penalties for non-compliance?
Penalties can be substantial, ranging from significant fines to legal action, reputational damage, and loss of patient trust. The severity depends on the nature and extent of the violation.
How can patients protect their privacy when using telehealth services?
Patients should carefully review privacy policies, ask questions about data collection practices, and only use telehealth platforms from reputable providers. They should also be aware of their rights under HIPAA and other relevant regulations.
Is anonymization a viable solution for protecting patient data?
Anonymization can help, but it’s not foolproof. Advanced techniques can sometimes re-identify anonymized data. A multi-layered approach to data security is necessary.