Doctor Corporate Ownership Growing Hospital Insurer, PAI Avalere
Doctor corporate ownership growing hospital insurer pai avalere – it’s a headline that screams change in the healthcare landscape. We’re seeing a massive shift, with large corporations gobbling up physician practices at an alarming rate. This isn’t just about money, though the financial incentives are undeniable; it’s reshaping the power dynamics between doctors, hospitals, and insurance companies, impacting everything from patient care to healthcare costs.
This post dives deep into this evolving situation, exploring the implications for all stakeholders.
The rise of corporate medicine has profound implications. Consider the changing negotiation landscape between hospitals and insurers – the presence of large corporate physician groups significantly alters the balance of power. We’ll examine how this consolidation influences pricing, reimbursement strategies, and even the availability of certain treatments. We’ll also explore Avalere’s role in analyzing these trends and offering insights into this complex and rapidly changing market.
It’s a story of consolidation, influence, and the ultimate question: what does it all mean for patients?
The Rise of Corporate Doctor Ownership
The healthcare landscape is undergoing a dramatic transformation, with a significant shift towards corporate ownership of physician practices. This trend, fueled by a complex interplay of economic, regulatory, and technological factors, is reshaping how healthcare is delivered and impacting both physicians and patients. This consolidation is raising important questions about the future of healthcare access, quality, and cost.
Factors Contributing to Corporate Ownership of Physician Practices
Several factors are driving the increasing consolidation of physician practices under corporate umbrellas. The rising administrative burden placed on independent practices, including billing, coding, and regulatory compliance, makes it increasingly difficult and expensive to operate independently. Simultaneously, the increasing complexity of healthcare reimbursement models, coupled with the pressure to adopt electronic health records (EHRs) and other technologies, necessitates significant upfront investment.
Furthermore, the increasing power of large hospital systems and insurance companies creates an environment where independent practices often find themselves at a disadvantage when negotiating contracts and securing favorable reimbursement rates. The resulting financial pressures often lead physicians to seek the stability and resources offered by corporate ownership.
Financial Incentives Driving Consolidation, Doctor corporate ownership growing hospital insurer pai avalere
Corporate ownership offers significant financial incentives for both physicians and investors. For physicians, it can provide a pathway to greater financial stability through guaranteed salaries, reduced administrative burdens, and access to capital for investment in technology and infrastructure. The corporate structure can also offer enhanced benefits packages, including retirement plans and malpractice insurance coverage, that are often difficult for small, independent practices to provide.
For investors, the healthcare industry represents a lucrative opportunity, with the potential for significant returns on investment through economies of scale and increased market share. The acquisition of physician practices allows for the creation of larger, more efficient networks that can leverage their size to negotiate better rates with insurers and suppliers.
Business Models of Corporate Physician Groups
Different corporate physician groups employ diverse business models. Some operate as independent physician associations (IPAs), where physicians maintain their individual practices but contract with the IPA for administrative services and managed care contracts. Others function as physician-owned hospital systems, integrating physicians into hospital-based practices. Still others operate as large, multi-specialty groups, offering a wide range of services under a single corporate umbrella.
Each model presents its own advantages and disadvantages regarding physician autonomy, financial risk, and the potential for conflicts of interest. For example, IPAs generally offer greater physician autonomy than fully integrated hospital-based practices, but they may also carry a higher degree of financial risk.
Market Share of Major Corporate Physician Ownership Groups
The market share of major corporate physician ownership groups is constantly evolving, making precise figures difficult to obtain. However, a representative snapshot (hypothetical data for illustrative purposes) might look like this:
| Corporate Group | Market Share (%) | Specialization Focus | Geographic Reach |
|---|---|---|---|
| MegaHealth Systems | 15 | Multi-specialty | National |
| CareAlliance Group | 10 | Primary Care | Regional |
| Physician Partners Inc. | 8 | Cardiology & Oncology | Regional |
| HealthFirst Network | 7 | Multi-specialty | National |
The Impact on Hospital-Insurer Relationships: Doctor Corporate Ownership Growing Hospital Insurer Pai Avalere
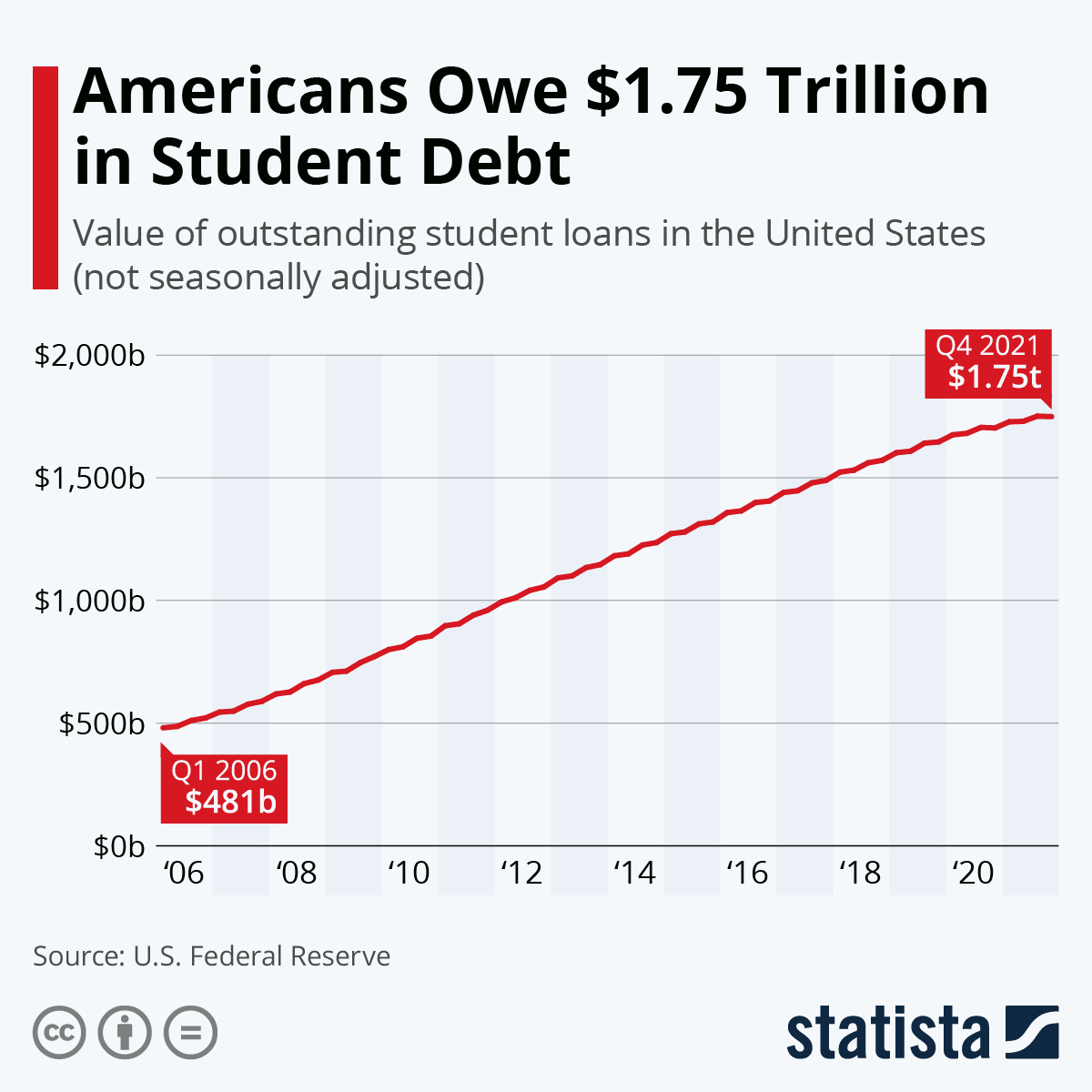
Source: statcdn.com
The rise of corporate physician ownership significantly alters the dynamics of negotiations between hospitals and insurers. Previously characterized by a more balanced power dynamic, the landscape is now shifting, with implications for healthcare pricing, reimbursement strategies, and overall market concentration. The integration of physician groups into larger corporate entities introduces new complexities and potential risks for hospitals seeking to maintain financial stability and competitive advantage.The introduction of large corporate physician groups as powerful negotiating entities fundamentally changes the bargaining power in healthcare negotiations.
Hospitals, previously negotiating with individual physician practices or smaller groups, now face consolidated entities with greater leverage. This shift impacts not only reimbursement rates but also the terms of contracts, potentially leading to reduced hospital revenue and decreased flexibility in service offerings.
Changes in Healthcare Pricing and Reimbursement Strategies
Corporate physician ownership frequently leads to revised healthcare pricing and reimbursement strategies. For example, a large corporate group might leverage its market share to negotiate higher reimbursement rates from insurers, effectively increasing the cost of care for patients. Conversely, they might use their influence to steer patients towards specific, often more expensive, procedures or treatments offered within their network, maximizing profits for the corporation.
This can create pressure on hospitals to align with these corporate strategies, even if it means accepting lower reimbursement rates for certain services to maintain access to a significant patient base. The potential for anti-competitive practices, such as price fixing or exclusionary conduct, also increases with concentrated corporate ownership. Consider a scenario where a large corporate group controls a significant portion of specialists in a given region.
This gives them considerable bargaining power to negotiate higher reimbursement rates from insurers, effectively driving up the overall cost of healthcare.
Increased Market Concentration and its Consequences
The consolidation of physician practices under corporate ownership contributes to increased market concentration in healthcare. This concentration can lead to reduced competition, potentially resulting in higher prices for consumers and less choice in healthcare providers. A region dominated by a few large corporate physician groups may see limited options for patients seeking specialized care, potentially affecting the quality of care and access to diverse treatment approaches.
Furthermore, this concentration can stifle innovation, as the incentive to develop new and cost-effective healthcare solutions diminishes in a less competitive market. For instance, a hypothetical scenario where one corporate group controls 70% of the cardiology practices in a state would significantly reduce competition and potentially lead to higher prices for cardiac procedures.
Strategies for Hospitals to Mitigate Risks
Hospitals need proactive strategies to mitigate the risks associated with the growing influence of corporate physician ownership. These strategies include developing strong data-driven negotiation strategies, cultivating strategic partnerships with other healthcare providers to increase bargaining power, and investing in innovative care models that offer value-based care and reduce reliance on fee-for-service models. Diversification of revenue streams, focusing on high-value services and building strong relationships with payers who value quality over cost are also critical.
For instance, a hospital could partner with other independent physician practices to create a larger network, thereby gaining more leverage in negotiations with insurers. Another strategy involves developing specialized centers of excellence that attract patients from a wider geographic area, making the hospital less reliant on local corporate physician groups.
Avalere’s Role in the Healthcare Landscape
Avalere Health is a prominent healthcare consulting firm that plays a significant role in analyzing and shaping the evolving landscape of physician ownership and its impact on hospital-insurer dynamics. Their expertise lies in providing data-driven insights and strategic guidance to various stakeholders within the healthcare industry, including hospitals, physician groups, and insurers. Understanding Avalere’s contributions is crucial for comprehending the complexities of this rapidly changing sector.Avalere’s key services directly relate to the rise of corporate physician ownership and its effects on hospital-insurer relationships.
They offer a wide range of services, including market research and analysis, strategic planning, regulatory compliance support, and performance improvement consulting. These services are specifically tailored to help clients navigate the challenges and opportunities presented by the increasing consolidation of physician practices and the shifting power dynamics between hospitals and insurers. For example, their market research can identify key trends in physician employment models and predict their impact on healthcare costs and quality, allowing hospitals and insurers to proactively adapt their strategies.
Avalere’s Analyses and Reports on Market Trends
Avalere regularly publishes reports and analyses focusing on the market trends within the healthcare sector, specifically concerning corporate physician ownership and its influence on hospital-insurer interactions. These publications often incorporate extensive data analysis, qualitative research, and expert interviews to provide a comprehensive understanding of the issues at hand. Their work frequently highlights the implications of these trends for healthcare costs, access to care, and the overall quality of patient care.
For instance, a report might detail the impact of a large physician group’s acquisition on a local market, examining the resulting changes in pricing negotiations with insurers and the potential effects on patient choice.
Avalere’s Involvement in Significant Events
A timeline illustrating Avalere’s involvement in significant events related to corporate physician ownership and hospital-insurer dynamics would highlight their contributions to the ongoing discussion. While a precise timeline requires access to their internal records, we can infer their involvement based on publicly available information and the nature of their services. For example, their participation in industry conferences and publications suggests ongoing engagement with the topic’s key players and trends.
The publication of their research reports, which often address specific regulatory changes or market shifts, indicates their responsiveness to significant events within the healthcare sector.
Key Findings from Avalere’s Publications
Avalere’s publications on corporate physician ownership and its impact on hospital-insurer relationships consistently reveal several key findings. These findings often shape the strategic decisions of hospitals and insurers.
- Increased market concentration among physician groups leads to greater negotiating power with insurers, potentially resulting in higher reimbursement rates.
- The shift towards corporate physician ownership can affect the quality of patient care, depending on the integration strategies employed by the acquiring entities.
- Regulatory changes and antitrust concerns play a significant role in shaping the landscape of corporate physician ownership and acquisitions.
- The financial implications of these ownership models are complex and can vary significantly depending on factors such as market dynamics and the specific business model of the acquiring entity.
- Data analysis and predictive modeling are crucial for understanding the long-term effects of corporate physician ownership on healthcare costs and access.
Patient Care Implications
The rise of corporate physician ownership within the healthcare landscape presents a complex picture regarding its impact on patient care. While proponents highlight potential efficiencies and improved access, concerns remain about the potential for prioritizing profits over patient well-being, ultimately altering the patient experience. Understanding these potential effects is crucial for navigating this evolving healthcare model.The potential impact of corporate physician ownership on patient access to care is multifaceted.
The increasing corporate ownership of doctor practices, highlighted by the Avalere report on hospital insurer partnerships, raises concerns about healthcare access and affordability. It makes me think about life choices and the future, like Karishma Mehta’s decision to freeze her eggs, as detailed in this article karishma mehta gets her eggs frozen know risks associated with egg freezing , which reminds us that personal health decisions are often complex and expensive, mirroring the complexities of the changing healthcare landscape under growing corporate influence.
Ultimately, both issues highlight the need for greater transparency and patient advocacy.
Larger corporate entities might possess the resources to expand services into underserved areas, potentially improving access for patients in rural communities or those lacking convenient access to specialists. However, this increased access could be offset by rising costs, leading to reduced affordability and limited access for patients with insufficient insurance coverage or those reliant on public assistance programs. The prioritization of profitable procedures over less lucrative but equally necessary ones could also limit access to specific types of care.
Access to Care and Affordability
Corporate ownership can lead to both increased and decreased access to care, depending on various factors. For instance, a large hospital system acquiring a group of independent physician practices might increase access to specialized services in a previously underserved region. However, this same system might also consolidate services, potentially closing smaller clinics in less profitable areas, thus reducing access for patients in those locations.
Furthermore, the potential for higher prices associated with corporate structures could make care less affordable, especially for patients without comprehensive insurance coverage. The balance between improved geographic access and financial accessibility remains a significant concern.
Quality of Care under Different Ownership Models
Comparing patient experiences under different models requires a nuanced approach. Studies have shown varying results, with some indicating that patient satisfaction scores are similar across different ownership models, while others suggest that patients in corporate-owned practices may experience less personalized attention. Independent practices, often characterized by stronger physician-patient relationships, may offer a higher level of personalized care, but may lack the resources and infrastructure of larger corporate entities.
The quality of care isn’t solely determined by ownership structure but is also influenced by factors such as staffing levels, technology utilization, and adherence to evidence-based guidelines.
Potential Benefits and Drawbacks for Patients
Potential benefits of corporate physician ownership include increased access to advanced technology and specialized care, potentially leading to improved treatment outcomes in certain cases. Economies of scale might also allow for better negotiation of prices with insurers, potentially leading to lower costs for patients. However, potential drawbacks include a decrease in the personal touch of physician-patient interactions, potential conflicts of interest due to financial incentives, and the risk of prioritizing profitability over patient needs.
For example, a corporate entity might incentivize physicians to order more expensive tests or procedures, even if less expensive alternatives would be equally effective, thus increasing costs for patients. The potential for reduced physician autonomy could also negatively impact the quality of care.
Regulatory and Policy Considerations
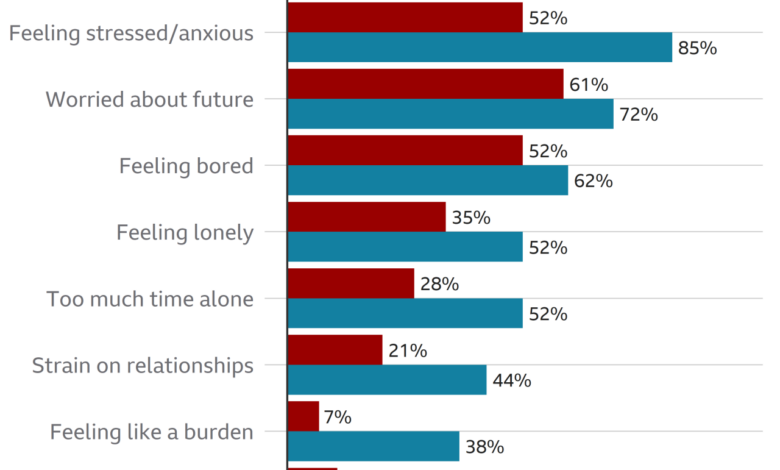
Source: co.uk
The rise of corporate physician ownership presents a complex web of regulatory and policy challenges. Existing frameworks, designed for a different healthcare landscape, are struggling to keep pace with this rapidly evolving model, raising concerns about market competition, patient care, and overall healthcare costs. Understanding current regulations and potential areas for reform is crucial for navigating this transformative period in healthcare delivery.Current regulations concerning corporate physician ownership vary significantly across states and often lack a cohesive national standard.
The increasing corporate ownership of doctor practices, highlighted by the recent Pai Avalere report on hospital insurer partnerships, raises concerns about potential conflicts of interest. Understanding these potential issues is crucial, especially considering the severity of conditions like stroke, where pre-existing conditions significantly impact outcomes. Check out this article on risk factors that make stroke more dangerous to see how these factors might be influenced by healthcare access and cost.
Ultimately, the growing influence of corporate entities on healthcare delivery needs careful monitoring, particularly concerning patient well-being and equitable access to care.
The Stark Law and the Anti-Kickback Statute, for example, aim to prevent physician self-referral and financial incentives that could compromise patient care, but their application in the context of large corporate ownership structures can be ambiguous and challenging to enforce. Furthermore, antitrust laws, designed to prevent monopolies and promote competition, are increasingly relevant as corporate consolidation in healthcare intensifies.
However, the application of these laws in the healthcare sector is often complex due to the unique characteristics of the industry, such as the presence of non-profit hospitals and the inherent complexities of healthcare markets.
Current Regulations and Policies
The current regulatory landscape governing corporate physician ownership is fragmented and often insufficient to address the potential risks associated with this trend. Federal regulations, such as the Stark Law and the Anti-Kickback Statute, aim to prevent conflicts of interest, but their effectiveness in managing the complexities of large corporate physician networks remains a subject of ongoing debate. State-level regulations also vary considerably, leading to inconsistencies in oversight and enforcement.
For instance, some states have stricter rules regarding physician compensation and ownership structures than others. This lack of uniformity can create regulatory arbitrage, where corporate entities seek out states with more lenient regulations. The result is a patchwork of rules that may not adequately protect patients or promote fair competition.
Potential Areas for Regulatory Reform
Several areas require increased regulatory scrutiny and potential reform. Clarifying the application of existing federal laws, such as the Stark Law and Anti-Kickback Statute, to large corporate physician ownership structures is crucial. This includes developing clearer guidelines and enforcement mechanisms to address potential conflicts of interest and ensure transparency in financial arrangements. Strengthening state-level regulations to create a more uniform national standard could also help to prevent regulatory arbitrage and ensure consistent oversight.
Furthermore, enhancing data collection and analysis on the impact of corporate physician ownership on healthcare costs, quality, and access is essential for informed policymaking. This could involve creating standardized reporting requirements for corporate physician groups and improving data sharing among state and federal agencies.
Policy Solutions to Address Concerns
Several policy solutions could help mitigate concerns related to corporate physician ownership. These include strengthening enforcement of existing regulations, improving transparency and disclosure requirements for corporate physician arrangements, and developing clearer guidelines for evaluating the potential impact of these arrangements on competition and patient care. Furthermore, investing in independent research and data analysis to better understand the long-term effects of corporate physician ownership on healthcare costs, quality, and access is essential.
Finally, exploring alternative models of healthcare delivery that emphasize value-based care and promote competition could provide a counterbalance to the increasing consolidation in the industry.
Impact of Antitrust Laws
Antitrust laws play a critical role in preventing monopolies and promoting competition in various sectors, including healthcare. However, applying these laws to the healthcare industry presents unique challenges due to its complex structure and the presence of non-profit entities. The increasing consolidation of healthcare providers, including the rise of corporate physician ownership, raises concerns about potential anti-competitive practices that could lead to higher costs, reduced choice, and compromised quality of care.
Enforcing antitrust laws effectively in this context requires a nuanced understanding of the healthcare market and the potential benefits and drawbacks of consolidation. Careful analysis is needed to differentiate between legitimate efficiencies resulting from consolidation and anti-competitive behavior that harms consumers. For example, the merger of two large hospital systems might lead to reduced costs through economies of scale, but it could also limit patient choice and increase market power, potentially leading to higher prices.
Balancing these competing considerations requires a thorough and rigorous approach to antitrust enforcement in the healthcare sector.
Future Trends and Predictions
The increasing consolidation of physician practices under corporate ownership is poised for significant evolution in the coming years. Several factors, including technological advancements and shifting regulatory landscapes, will shape the future trajectory of this trend, impacting healthcare delivery, costs, and patient experience in profound ways. Understanding these potential developments is crucial for stakeholders across the healthcare ecosystem.The integration of technology will be a pivotal driver of future trends.
This isn’t simply about adopting electronic health records; it’s about leveraging AI for diagnostics, remote patient monitoring, and personalized medicine.
The rise of doctor corporate ownership and the growing influence of hospital insurer giants like Avalere are reshaping healthcare. This consolidation raises concerns about access and affordability, especially when considering the technological advancements discussed by Sean Kennedy on Salesforce’s healthcare AI initiatives, salesforce healthcare ai sean kennedy. Ultimately, these tech solutions might even exacerbate the issues created by concentrated ownership if not carefully implemented within a fair and equitable system.
Technological Advancements and Their Effects
Telemedicine, already accelerated by the pandemic, will further integrate with corporate physician networks. Imagine a scenario where a large corporate medical group uses AI-powered diagnostic tools to analyze patient data remotely, providing faster and more accurate diagnoses. This could lead to more efficient resource allocation, potentially reducing wait times and improving patient outcomes. The use of AI in administrative tasks, such as billing and scheduling, could free up physicians to focus on patient care.
Simultaneously, the increased use of data analytics will allow these corporations to better understand population health needs, leading to more proactive and preventative care strategies. For example, a corporation might identify a high incidence of diabetes in a specific geographic area served by its network and implement targeted preventative programs.
A Potential Future Healthcare Landscape
Consider this scenario: By 2035, several large corporate entities dominate the healthcare landscape. These corporations own extensive networks of hospitals, clinics, and physician practices, all seamlessly integrated through advanced technology. Patients benefit from convenient access to care, personalized treatment plans based on AI-driven analysis, and proactive health management through remote monitoring. However, concerns about potential monopolies, equitable access, and data privacy remain.
This highly consolidated system could offer superior efficiency and coordinated care, but the potential for increased costs and reduced choice for patients needs careful consideration. The rise of specialized corporate entities focusing on niche areas, such as oncology or cardiology, may also become more prevalent, offering deeper expertise but potentially limiting patient choice within a specific area.
Future Challenges and Opportunities
The future of corporate physician ownership presents both significant challenges and opportunities.
- Challenge: Maintaining the physician-patient relationship in a large corporate structure. Balancing the need for efficiency with the importance of personalized care is crucial.
- Challenge: Ensuring equitable access to care across different socioeconomic groups. The potential for increased costs and limited access in underserved communities needs to be addressed proactively.
- Challenge: Addressing concerns about data privacy and security in a highly interconnected system. Robust safeguards are essential to protect patient information.
- Opportunity: Improving efficiency and reducing healthcare costs through better coordination of care and utilization of technology.
- Opportunity: Advancing medical research and innovation through the aggregation of large datasets and collaborative efforts.
- Opportunity: Implementing proactive and preventative care strategies based on population health data analysis, leading to improved patient outcomes.
Last Word
The growing corporate ownership of physician practices is undeniably transforming healthcare. While offering potential efficiencies and streamlined processes, it also raises significant concerns about market concentration, potential conflicts of interest, and the ultimate impact on patient care and access. Understanding the role of companies like Avalere in analyzing these trends is crucial. As this trend continues to evolve, we must carefully consider the long-term implications for the quality, affordability, and accessibility of healthcare for everyone.
The conversation is far from over, and staying informed is more important than ever.
Commonly Asked Questions
What are the potential antitrust concerns related to corporate physician ownership?
Increased market concentration through corporate acquisitions can lead to reduced competition, potentially resulting in higher prices and less choice for patients. Antitrust laws are designed to prevent such monopolies, but their application in this complex healthcare market is constantly being challenged and refined.
How does corporate ownership impact physician autonomy?
This is a complex issue. While some physicians find benefits in reduced administrative burden and access to resources, others worry about decreased clinical autonomy and pressure to prioritize profitability over patient care.
What are some examples of Avalere’s specific reports or analyses on this topic?
To find specific examples, you’d need to visit Avalere’s website and search their publications. They frequently release reports on market trends in healthcare, including those related to physician practice consolidation.
