New York Safe Staffing Critical Care Ratios
New York safe staffing critical care ratios are a hot topic right now, and for good reason! The debate around nurse-to-patient ratios in critical care units is impacting patient outcomes, hospital budgets, and the very lives of healthcare professionals. This post dives deep into the current situation in New York, comparing it to other states and exploring the economic and human factors at play.
We’ll look at the data, the perspectives of those on the front lines, and what needs to happen to ensure safe and effective care for everyone.
From the bustling ICUs of NYC to the smaller hospitals upstate, the realities of critical care staffing vary widely. We’ll examine the current ratios, the impact on patient mortality and medical errors, and what the data tells us about patient satisfaction. We’ll also explore the financial implications of improving ratios, considering the potential impact on hospital budgets and the strategies needed to address these challenges.
Finally, we’ll hear from the healthcare professionals themselves – nurses, doctors, and administrators – to understand their perspectives and the potential conflicts arising from differing priorities.
Current New York State Critical Care Staffing Ratios
New York State, like many other states, grapples with the complexities of critical care staffing ratios. Finding the optimal balance between providing high-quality patient care and ensuring the well-being of healthcare professionals is a constant challenge. The issue is further complicated by variations in hospital size, location, and the specific needs of different critical care units. While a statewide mandated ratio doesn’t exist, understanding the current landscape of staffing levels is crucial for improving patient outcomes and working conditions.
Nurse-to-Patient Ratios in New York’s Critical Care Units
The nurse-to-patient ratio in New York’s critical care units varies significantly. This fluctuation depends on several factors, including the acuity of patients, the availability of support staff (like respiratory therapists and patient care technicians), and the specific policies of individual hospitals. While some hospitals may strive for lower ratios to ensure more individualized attention, others might operate with higher ratios due to staffing shortages or budgetary constraints.
The ideal ratio is often debated among healthcare professionals, with many advocating for lower ratios to improve patient safety and reduce nurse burnout. It’s important to note that even within a single hospital, ratios can differ between units based on patient needs.
Variations in Staffing Ratios Across Critical Care Settings
The differences in staffing ratios are particularly evident when comparing various critical care settings. Intensive Care Units (ICUs) typically have the most critically ill patients, often requiring highly specialized care and continuous monitoring. Consequently, ICUs generally aim for lower nurse-to-patient ratios than Cardiac Care Units (CCUs), which may have patients with less complex needs. Similarly, other specialized units like Neurological ICUs or Neonatal ICUs might have their own unique staffing considerations based on patient acuity and the intensity of required care.
The fight for New York’s safe staffing critical care ratios is crucial for patient well-being, demanding better nurse-to-patient ratios. This increased workload highlights the need for efficient documentation, which is why news about nuance integrating generative AI scribe with Epic EHRs is so interesting. Imagine the time saved! Ultimately, this tech could free up nurses to focus more directly on patient care, indirectly bolstering the effectiveness of those hard-fought-for safe staffing ratios.
This variability highlights the need for flexible staffing models that adapt to the dynamic needs of each unit.
Examples of Hospitals in New York with Varying Staffing Levels
It’s challenging to provide precise, publicly available, real-time data on nurse-to-patient ratios for specific New York hospitals. This information is often considered proprietary and not consistently reported publicly. However, we can illustrate the potential range of ratios with hypothetical examples, reflecting the general variability observed across the state. Remember that these are illustrative examples and do not represent actual, confirmed ratios.
| Hospital Name | Location | Nurse-to-Patient Ratio (ICU) | Nurse-to-Patient Ratio (CCU) |
|---|---|---|---|
| Hypothetical Hospital A | New York City | 1:1 | 1:2 |
| Hypothetical Hospital B | Upstate New York | 1:2 | 1:3 |
| Hypothetical Hospital C | New York City | 1:1.5 | 1:2.5 |
| Hypothetical Hospital D | Upstate New York | 1:2.5 | 1:4 |
Impact of Staffing Ratios on Patient Outcomes
The implementation of mandated nurse-to-patient ratios in New York’s critical care units has sparked significant debate, with a central focus on the impact on patient outcomes. While the effects are complex and not always immediately apparent, a growing body of research suggests a strong correlation between adequate staffing and improved patient care. This section will explore the relationship between staffing levels and key patient outcome indicators.Improved nurse staffing levels in critical care settings directly influence several key patient outcomes.
This is because nurses are the frontline providers, responsible for direct patient care, medication administration, and close monitoring of vital signs. Reduced workloads allow for more attentive and proactive care, leading to better patient management.
Nurse-to-Patient Ratios and Patient Mortality Rates
Studies have consistently shown a link between lower nurse-to-patient ratios and increased patient mortality rates in critical care settings. For example, research published in theAmerican Journal of Nursing* demonstrated a statistically significant association between higher nurse workloads (indicated by lower ratios) and a higher risk of in-hospital mortality for patients in intensive care units. This increased mortality risk is likely attributable to factors such as delayed response to critical events, increased medication errors due to rushed care, and reduced time for effective communication and collaboration among the healthcare team.
The improved ability of nurses to provide timely and effective interventions in better-staffed units is a significant factor in reducing mortality risk.
Staffing Levels and the Incidence of Medical Errors
Adequate staffing is crucial in reducing medical errors. Overworked nurses are more prone to making mistakes due to fatigue, stress, and cognitive overload. A study conducted by the Agency for Healthcare Research and Quality (AHRQ) indicated a direct correlation between high nurse-to-patient ratios and an increased incidence of medication errors, falls, and other preventable adverse events in critical care.
This underscores the importance of maintaining appropriate staffing levels to minimize risks associated with human error in high-pressure environments. The reduction in errors contributes directly to improved patient safety.
Patient Satisfaction Scores and Nurse Staffing Levels
Patient satisfaction is another critical indicator of the quality of care received. Numerous studies have shown a positive correlation between higher nurse staffing levels and improved patient satisfaction scores. Patients in units with lower nurse-to-patient ratios consistently report higher levels of perceived nurse attentiveness, responsiveness to their needs, and overall satisfaction with their care.
The fight for better New York safe staffing critical care ratios is crucial for patient safety. It makes you wonder about the resources hospitals are allocating – I just read about Mass General Brigham’s buyout of a digital unit, as detailed in this article: Mass General Brigham Buyouts Digital Unit. This kind of investment in technology highlights the need for similar financial commitments to improving nurse-to-patient ratios in New York’s critical care units.
Ultimately, it’s about prioritizing patient well-being.
The following bullet points summarize the key connections between staffing ratios and patient outcomes:
- Lower nurse-to-patient ratios: Associated with increased patient mortality rates, higher incidence of medical errors, and lower patient satisfaction scores.
- Higher nurse-to-patient ratios: Associated with decreased patient mortality rates, lower incidence of medical errors, and improved patient satisfaction scores.
- Improved nurse-patient communication: Better staffing allows for more time for nurses to communicate effectively with patients and their families, leading to increased patient trust and improved satisfaction.
- Reduced nurse burnout: Appropriate staffing levels help reduce nurse burnout and improve job satisfaction, leading to improved patient care and outcomes.
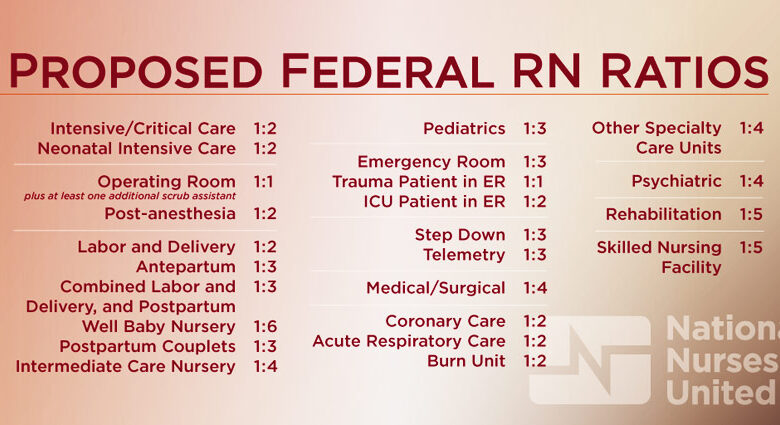
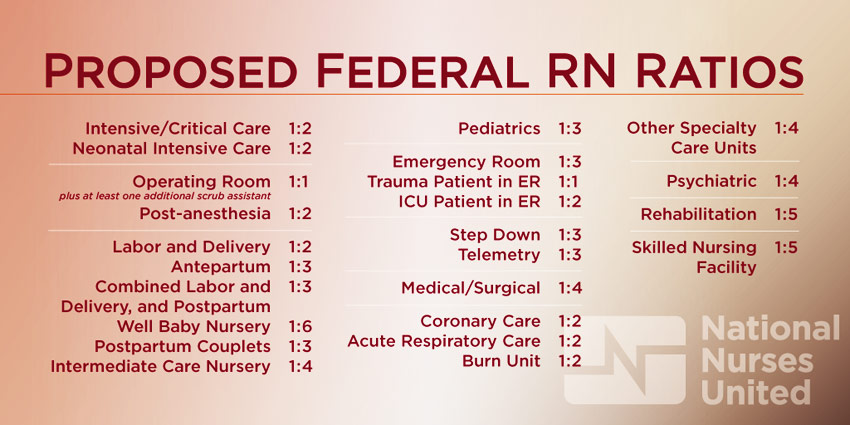
Comparison with Other States’ Staffing Regulations
New York’s recent strides in establishing critical care staffing ratios represent a significant step towards improving patient safety and nurse well-being. However, it’s crucial to understand how New York’s regulations compare to those in other states to gauge its effectiveness and identify potential areas for further improvement. This comparison will highlight the variations in approaches and their potential impact on patient care quality.
Analyzing staffing regulations across different states reveals a patchwork of approaches, ranging from mandated ratios to less prescriptive guidelines. This variability reflects differing political priorities, healthcare systems, and resource availability. Understanding these differences is crucial for evaluating the overall effectiveness of various regulatory strategies in ensuring safe patient care.
State-by-State Comparison of Critical Care Staffing Ratios
The following table compares New York’s critical care staffing regulations with those of California, Pennsylvania, and Texas. It’s important to note that the specifics of these regulations can be complex, and this table provides a simplified overview. Always consult the official state legislation for the most accurate and up-to-date information.
| State | Nurse-to-Patient Ratio (ICU) | Nurse-to-Patient Ratio (CCU) | Relevant Legislation |
|---|---|---|---|
| New York | 1:3 (with exceptions) | 1:3 (with exceptions) | New York State’s Safe Staffing for Nurses Act |
| California | Varies by hospital and unit; generally higher ratios than New York | Varies by hospital and unit; generally higher ratios than New York | California’s regulations are less prescriptive than New York’s, focusing on nurse-to-patient ratios in specific situations rather than setting a blanket ratio. |
| Pennsylvania | No mandated ratios | No mandated ratios | Pennsylvania relies on hospital-specific staffing plans and committees to determine appropriate nurse-to-patient ratios. |
| Texas | No mandated ratios | No mandated ratios | Texas does not have state-mandated nurse-to-patient ratios for critical care units. Hospitals are responsible for their own staffing plans. |
Implications of Differing Staffing Regulations
The significant differences in staffing regulations across these states have considerable implications for patient care. States with mandated ratios, like New York (with its exceptions), aim to ensure a minimum level of nurse attention for each patient. This can lead to improved patient outcomes, reduced medical errors, and enhanced nurse job satisfaction. However, the implementation of mandated ratios can also lead to increased healthcare costs and potential challenges in staffing during periods of high demand.
Conversely, states without mandated ratios may experience greater variability in staffing levels, potentially impacting patient safety and nurse burnout. For example, a hospital in Pennsylvania might have adequate staffing one day, and critically low staffing the next, depending on various factors.
The absence of mandated ratios in states like Pennsylvania and Texas allows for greater flexibility in staffing decisions but potentially increases the risk of understaffing. This can result in increased patient mortality, longer hospital stays, and higher rates of medical errors. California’s less prescriptive approach presents a middle ground, offering more flexibility than New York while still providing some regulatory oversight.
The ultimate impact on patient care depends on the effectiveness of hospital-specific staffing plans and oversight mechanisms.
Economic Considerations of Safe Staffing Ratios
Implementing safer nurse-to-patient ratios in New York’s critical care units will undoubtedly have significant financial implications for hospitals. While improved patient outcomes are a crucial benefit, the increased cost of staffing needs careful consideration and strategic planning to ensure fiscal sustainability. This section explores the potential economic impact and strategies for mitigation.The immediate and most obvious impact is increased labor costs.
Higher nurse-to-patient ratios necessitate employing more nurses, leading to a substantial increase in payroll expenses. This increase will vary depending on factors such as the specific ratio implemented, the size of the critical care unit, and the prevailing wage rates for nurses in New York. For example, a hospital with a 10-bed critical care unit might see a 20% increase in nursing payroll if the ratio changes from 1:4 to 1:3.
This translates to significant additional expenditure annually. Furthermore, the increased demand for nurses could lead to competitive bidding for qualified professionals, potentially driving up wages further.
Increased Hospital Budgetary Strain
The increased labor costs associated with safer staffing ratios will directly strain hospital budgets. Hospitals operate on tight margins, and significant increases in personnel costs could impact other areas, such as investments in new equipment, facility upgrades, or research initiatives. This could potentially lead to reduced investment in other essential areas or necessitate exploring alternative revenue streams. Hospitals may need to reassess their overall financial strategies and potentially seek additional funding sources to offset the increased expenses.
For instance, a hospital might need to explore options such as increasing patient charges, seeking government grants, or optimizing operational efficiencies.
Strategies for Mitigating Economic Challenges
Several strategies can help mitigate the economic challenges associated with increased staffing. These include optimizing staffing models to maximize efficiency, exploring innovative financial models, and seeking external funding opportunities. For example, hospitals could implement advanced scheduling systems that predict staffing needs more accurately, reducing overtime costs. They could also explore partnerships with nursing schools to develop training programs that produce a pipeline of qualified nurses, potentially lowering recruitment costs in the long run.
Innovative Financial Models and External Funding
Exploring innovative financial models, such as value-based reimbursement, can also help alleviate budgetary pressures. Value-based reimbursement ties payments to the quality of care provided, rather than simply the volume of services. Improved patient outcomes resulting from safer staffing ratios could lead to higher reimbursements under this model, potentially offsetting some of the increased labor costs. Furthermore, hospitals could actively seek external funding opportunities, such as grants from foundations or government agencies specifically dedicated to improving healthcare quality and safety.
New York’s safe staffing critical care ratios are a hot topic, and rightly so – patient safety depends on it! But the staffing challenges aren’t limited to big city hospitals; the struggles are real even in rural areas, as highlighted by this article on the impact of staffing shortages on rural hospitals’ labor and delivery services: Rural Hospitals Labor Delivery &.
Understanding these broader issues helps us see how crucial safe staffing ratios are, not just in New York’s critical care units, but across the entire healthcare system.
Securing these grants could provide significant financial support for implementing and sustaining safer staffing ratios. Examples of such funding sources include the New York State Department of Health grants focused on improving patient care quality and safety.
Perspectives of Healthcare Professionals

Source: ytimg.com
The implementation of safe staffing ratios in New York’s critical care units has elicited a wide range of responses from healthcare professionals. Understanding these perspectives is crucial for evaluating the effectiveness and impact of the new regulations. The opinions expressed vary significantly depending on professional role, individual experiences, and the specific context of their work environment.
Nurse Perspectives on Safe Staffing Ratios, New york safe staffing critical care ratios
Nurses, being the most directly impacted by staffing levels, offer valuable insights. Many nurses report feeling significantly less stressed and burnt out under improved staffing ratios. They describe having more time for patient care, leading to improved patient outcomes and a greater sense of job satisfaction. Conversely, some nurses express concerns about the potential for increased workload if the ratios are not properly implemented or if there is a shortage of qualified staff to meet the requirements.
The increased responsibility for individual nurses could lead to greater stress in some scenarios if appropriate support systems aren’t in place. Anecdotal evidence suggests that improved nurse-to-patient ratios are associated with a decrease in medication errors and a reduction in patient falls.
Physician Perspectives on Safe Staffing Ratios
Physicians, while not directly affected by the nurse-to-patient ratios in the same way as nurses, also have a vested interest in safe staffing levels. Improved nurse staffing often translates to better patient monitoring and more timely responses to critical events. This allows physicians to focus on more complex aspects of patient care and improves overall efficiency within the unit.
However, some physicians might express concerns about the potential cost implications of increased staffing levels, particularly in already financially strained hospitals. Concerns about the potential for administrative bottlenecks in implementing and managing the new ratios have also been raised.
Perspectives of Other Healthcare Professionals
The impact of safe staffing ratios extends beyond nurses and physicians. Respiratory therapists, pharmacists, and other allied health professionals benefit from a better-supported nursing staff. Improved nurse-patient ratios can lead to more efficient collaboration and improved communication among the healthcare team. This collaborative approach leads to enhanced patient safety and improved overall care delivery. Conversely, some professionals may worry about increased workload if the increased staffing does not translate to a better division of labor.
Proper implementation and training are key to avoiding potential negative consequences.
Potential for Conflict Between Hospital Administration and Healthcare Providers
The implementation of safe staffing ratios often creates tension between hospital administration and healthcare providers. Administrators may be concerned about the financial implications of increased staffing costs, potentially leading to conflicts with nurses and other healthcare professionals who advocate for safe staffing levels. This conflict can manifest in various ways, including disagreements over the interpretation of the regulations, disputes over resource allocation, and even labor disputes.
Finding a balance between ensuring patient safety and maintaining financial viability requires open communication, collaboration, and a commitment to finding mutually beneficial solutions. Successful implementation requires a collaborative approach, involving all stakeholders in the decision-making process.
Advocacy and Policy Recommendations

Source: slidesharecdn.com
The fight for safer critical care staffing ratios in New York is a complex battle fought on multiple fronts, involving tireless advocacy from various groups and a constant push for policy changes that prioritize patient safety. This section details the ongoing efforts and proposes concrete policy recommendations to achieve and maintain safer staffing levels.The current situation highlights a critical need for stronger legislation and enforcement.
While some progress has been made, the persistent challenges underscore the necessity of a multi-pronged approach involving advocacy, policy reform, and effective implementation strategies.
Efforts of Advocacy Groups and Professional Organizations
Numerous organizations have championed the cause of improved critical care staffing ratios. The New York State Nurses Association (NYSNA), for example, has been a vocal advocate, lobbying for legislation and actively engaging in public awareness campaigns to highlight the link between understaffing and negative patient outcomes. Similar efforts have been undertaken by other professional organizations representing critical care physicians, respiratory therapists, and other healthcare professionals.
These groups often collaborate, pooling resources and expertise to amplify their collective voice and influence policy decisions. Their strategies include lobbying state legislators, participating in public forums and hearings, and publishing research and reports highlighting the detrimental effects of inadequate staffing. Furthermore, they leverage media attention to raise public awareness and pressure policymakers to act. For instance, NYSNA’s public campaigns have included powerful testimonials from nurses detailing the challenges of providing safe care in understaffed units.
Policy Recommendations for Achieving Safer Staffing Levels
To ensure safer staffing levels, a comprehensive approach is necessary. This involves a combination of legislative action, regulatory oversight, and resource allocation.
- Mandated Minimum Staffing Ratios: The state should enact legislation establishing mandatory minimum staffing ratios for critical care units, based on evidence-based research and best practices. These ratios should be adjusted to reflect the complexity of patient care needs and the acuity of the unit.
- Increased Funding for Healthcare Facilities: Adequate funding is crucial for hospitals to meet mandated staffing ratios. This may involve increased state and federal funding, as well as innovative reimbursement models that incentivize safe staffing practices.
- Enhanced Enforcement Mechanisms: Stronger enforcement mechanisms are needed to ensure compliance with mandated staffing ratios. This could involve regular audits, penalties for non-compliance, and transparent reporting of staffing levels and patient outcomes.
- Data Collection and Transparency: A robust system for collecting and publicly reporting data on staffing levels, patient outcomes, and nurse-to-patient ratios is essential for monitoring compliance and identifying areas needing improvement. This transparency would allow for better accountability and informed decision-making.
- Investment in Workforce Development: Addressing the nursing shortage is critical. This requires increased funding for nursing education programs, loan forgiveness initiatives, and recruitment strategies to attract and retain qualified critical care nurses.
Implementation Strategies for Policy Recommendations
Effective implementation requires a phased approach with clear timelines and accountability measures.The initial phase could focus on establishing the mandated minimum staffing ratios, with a gradual implementation timeline allowing hospitals time to adjust. Simultaneously, the state could increase funding for healthcare facilities, providing financial support to meet the new requirements. A robust data collection system should be implemented concurrently, providing a baseline for monitoring compliance and evaluating the impact of the new ratios.
The next phase would focus on strengthening enforcement mechanisms, including regular audits and penalties for non-compliance. Finally, sustained investment in workforce development is crucial for long-term success. This includes not only recruitment but also ongoing professional development opportunities for critical care nurses to enhance their skills and expertise. Regular evaluation and adjustments to the policy based on data analysis are essential for ensuring its effectiveness and responsiveness to evolving needs.
For example, the initial implementation could focus on the most critical units (e.g., ICUs with the highest patient acuity) before expanding to other critical care areas. This phased approach would minimize disruption and allow for continuous improvement based on ongoing monitoring and feedback.
Illustrative Case Studies: New York Safe Staffing Critical Care Ratios
Source: nclexquiz.com
This section presents two contrasting case studies to illustrate the impact of safe staffing ratios on patient outcomes in New York’s critical care units. One case demonstrates the benefits of adequate staffing, while the other highlights the negative consequences of understaffing. These examples are not intended to represent every scenario, but rather to provide concrete illustrations of the principles discussed previously.
Positive Outcomes of Adequate Staffing: Case Study 1
This case involves a 65-year-old male patient admitted to a New York City ICU with acute respiratory distress syndrome (ARDS) following a severe pneumonia infection. The ICU, operating with a nurse-to-patient ratio of 1:2, allowed for meticulous attention to the patient’s complex needs. Nurses were able to consistently monitor vital signs, administer medications precisely, and promptly address any changes in the patient’s condition.
The dedicated nursing staff implemented proactive measures, including meticulous pulmonary hygiene and early mobilization protocols, preventing secondary infections and promoting faster recovery. The patient responded well to treatment, experienced a steady improvement in oxygenation, and was eventually weaned off mechanical ventilation after 10 days. He was discharged to a rehabilitation facility after a total of three weeks in the hospital, showing significant functional improvement.
The close monitoring and timely interventions directly attributable to the adequate staffing played a crucial role in his successful recovery.
Negative Outcomes of Inadequate Staffing: Case Study 2
In contrast, this case study focuses on a 72-year-old female patient admitted to a rural New York ICU with a severe myocardial infarction (heart attack) complicated by cardiogenic shock. The ICU was operating with a nurse-to-patient ratio of 1:4 due to staff shortages. The high patient load significantly impacted the quality of care. Nurses struggled to maintain consistent monitoring of vital signs, leading to a delayed response to a critical drop in blood pressure.
Medication administration was also affected by the workload, resulting in a slight delay in administering crucial life-saving drugs. The patient’s condition deteriorated rapidly, necessitating emergency interventions including intubation and the use of vasopressors. Despite these interventions, the patient experienced prolonged complications, including acute kidney injury and prolonged mechanical ventilation. Her hospital stay extended to six weeks, and she experienced significant functional limitations upon discharge.
The delayed responses and suboptimal care directly linked to the inadequate staffing significantly contributed to the patient’s prolonged recovery and diminished quality of life.
Conclusive Thoughts
Ultimately, ensuring safe staffing ratios in New York’s critical care units is a complex issue with far-reaching consequences. It’s not just about numbers on a page; it’s about the lives of patients and the well-being of healthcare professionals. By understanding the current situation, the economic realities, and the perspectives of all stakeholders, we can work towards creating a system that prioritizes both quality of care and the sustainability of our healthcare system.
The path forward requires collaboration, data-driven decision-making, and a commitment to improving patient outcomes and protecting our healthcare heroes. Let’s keep the conversation going and advocate for positive change.
Commonly Asked Questions
What are the potential legal ramifications of unsafe staffing ratios?
Hospitals failing to meet minimum staffing requirements could face legal action from patients or families who experience negative outcomes due to understaffing. This could include malpractice lawsuits and regulatory penalties.
How do safe staffing ratios affect nurse burnout?
Adequate staffing can significantly reduce nurse burnout by lessening workload and stress. Conversely, understaffing contributes to exhaustion, compassion fatigue, and increased risk of making errors.
Are there specific certifications or training programs related to safe staffing advocacy?
While there isn’t a specific certification, many professional organizations offer training and resources on advocacy, policy, and healthcare management relevant to safe staffing initiatives. Look into resources offered by nursing unions and healthcare advocacy groups.

