Benefits of Lemon Cucumber Honey Water for Clear Skin
Benefits of lemon cucumber and honey water for clear skin? Let’s dive in! We all crave that radiant, healthy glow, and this simple, delicious drink might just be the key. This post explores the individual powers of lemon, cucumber, and honey – each a skincare superstar in its own right – and how their combined magic can work wonders for your complexion.
Get ready to unlock your skin’s natural radiance!
Imagine a refreshing drink that not only quenches your thirst but also helps clear your skin. That’s the promise of lemon, cucumber, and honey water. We’ll uncover the science behind why these ingredients are so beneficial, from boosting collagen production to soothing inflammation. Plus, we’ll share a simple recipe and address any potential concerns you might have.
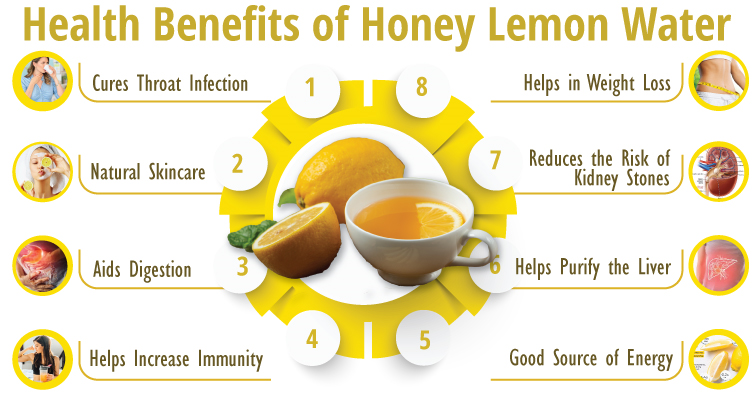
Benefits of Lemon, Cucumber, and Honey Water for Skin

Source: ytimg.com
Lemon, cucumber, and honey, individually potent ingredients for skin health, combine synergistically to create a refreshing and effective drink that can contribute to clearer, healthier skin. This revitalizing concoction offers a natural and delicious way to boost your skin’s radiance and address various skin concerns. The combined effects of these three natural ingredients offer a holistic approach to skincare, addressing hydration, inflammation, and overall skin tone.This drink leverages the individual benefits of each ingredient to create a powerful, yet gentle, skin-enhancing elixir.
Lemon’s high Vitamin C content acts as a potent antioxidant, protecting skin from free radical damage and promoting collagen production for firmer, smoother skin. Cucumber, rich in water and antioxidants, hydrates the skin from the inside out, reducing puffiness and inflammation. Honey, a natural humectant, draws moisture from the air to the skin, keeping it hydrated and preventing dryness.
The combination of these three creates a powerful trifecta for skin health.
Individual Ingredient Benefits
Lemon’s high concentration of Vitamin C is a key player in collagen synthesis, a crucial protein for skin elasticity and firmness. It also acts as a powerful antioxidant, neutralizing free radicals that contribute to premature aging and skin damage. Furthermore, its citric acid can help gently exfoliate the skin, removing dead skin cells and promoting a brighter complexion.
The potent antibacterial properties of lemon can also help combat acne-causing bacteria.Cucumber’s high water content contributes significantly to skin hydration. Its refreshing properties help reduce puffiness and inflammation, soothing irritated skin. It’s also a rich source of antioxidants like vitamin K and caffeic acid, which help protect the skin from damage and reduce dark circles under the eyes.
The gentle cooling effect of cucumber can provide relief from sunburns or other skin irritations.Honey, a natural humectant, draws moisture from the air and binds it to the skin, keeping it hydrated and preventing dryness. Its antibacterial and anti-inflammatory properties can help soothe acne and other skin conditions. Furthermore, honey contains various antioxidants and nutrients that contribute to overall skin health and a healthy glow.
Synergistic Effects of Combined Ingredients
The combined effect of lemon, cucumber, and honey in water creates a powerful synergy. The lemon provides a boost of Vitamin C and antioxidants, while the cucumber hydrates and soothes. Honey, meanwhile, seals in moisture and provides additional antibacterial and anti-inflammatory benefits. This combined action leads to improved skin hydration, reduced inflammation, a brighter complexion, and a reduction in acne and other skin imperfections.
The water itself serves as a crucial base, ensuring the easy absorption of the nutrients and promoting overall hydration. For example, drinking this concoction regularly can lead to noticeably smoother, clearer skin within a few weeks, provided a consistent healthy diet and lifestyle are also maintained.
Lemon’s Role in Skin Clarity
Lemons, a vibrant citrus fruit, offer a wealth of benefits for the skin, largely thanks to their impressive nutritional profile. Beyond their refreshing taste, they pack a powerful punch when it comes to achieving clearer, healthier skin. Let’s delve into the specific ways lemons contribute to skin clarity.
Vitamin C and Collagen Production
Lemons are an excellent source of Vitamin C, a potent antioxidant crucial for collagen synthesis. Collagen is a protein that provides structure and elasticity to the skin, keeping it firm and youthful. Vitamin C acts as a co-factor in the enzymatic reactions that build collagen, meaning it’s essential for the process to occur efficiently. A deficiency in Vitamin C can lead to reduced collagen production, resulting in wrinkles, sagging skin, and a less vibrant complexion.
Consuming lemon water, or applying topical treatments containing lemon extract (in moderation, due to its acidity), can help boost collagen levels and maintain skin’s structural integrity.
Lemon’s Antioxidant Properties and Free Radical Damage
Free radicals are unstable molecules that damage skin cells, leading to premature aging and various skin problems. Lemons are rich in antioxidants, including Vitamin C and flavonoids, which neutralize these harmful free radicals. This antioxidant action protects skin cells from oxidative stress, reducing the appearance of wrinkles, fine lines, and age spots. By combating free radical damage, lemons help preserve the skin’s youthful appearance and overall health.
Lemon’s Ability to Lighten Skin and Reduce Hyperpigmentation
The citric acid in lemons possesses natural bleaching properties. This can help lighten dark spots and hyperpigmentation, such as age spots, sunspots, and acne scars. However, it’s crucial to use lemon juice topically with caution and in diluted form, as its high acidity can irritate sensitive skin. Always perform a patch test before applying it directly to the face, and avoid prolonged sun exposure after application, as it can increase photosensitivity.
The lightening effect is due to the inhibition of melanin production, the pigment responsible for skin color.
Comparison of Lemon’s Skin Benefits to Other Citrus Fruits
| Name | Vitamin C content (mg/100g) | Antioxidant Properties | Skin benefits |
|---|---|---|---|
| Lemon | 53 | High (Vitamin C, flavonoids) | Collagen production, antioxidant protection, skin lightening |
| Orange | 53 | High (Vitamin C, flavonoids) | Antioxidant protection, hydration |
| Grapefruit | 44 | High (Vitamin C, lycopene) | Antioxidant protection, potential anti-aging effects |
| Lime | 34 | Moderate (Vitamin C) | Antioxidant protection, skin brightening |
Cucumber’s Contribution to Skin Health
Source: medium.com
So, I’ve been really into this lemon, cucumber, and honey water for clearer skin – it’s amazing! I’m always looking for ways to boost my health, inside and out, which got me thinking about preventative health measures. I read this fascinating article on how an eye test might help detect dementia risk in older adults – check it out: can eye test detect dementia risk in older adults.
It’s incredible how interconnected our health is! Anyway, back to my glowing skin – the lemon water really seems to be making a difference.
Cucumbers aren’t just a refreshing snack; they’re a powerhouse of skin-loving nutrients. Their high water content and unique composition make them a fantastic natural remedy for various skin concerns, contributing significantly to a clearer, healthier complexion when incorporated into a skincare routine.Cucumber’s hydrating properties and their effect on skin moisture are remarkable. The high water content in cucumbers (around 96%) acts as a natural humectant, drawing moisture from the air and locking it into the skin.
This helps to plump up the skin, reducing the appearance of fine lines and wrinkles, and leaving it feeling soft and supple. This intense hydration is particularly beneficial for dry or dehydrated skin types, combating dryness and restoring a healthy moisture balance.
Cucumber’s Anti-inflammatory and Soothing Properties
Cucumber possesses remarkable anti-inflammatory properties, thanks to its rich concentration of antioxidants and other beneficial compounds. These properties make it incredibly soothing for irritated, inflamed, or sunburned skin. The cooling effect of cucumber further enhances its soothing capabilities, providing immediate relief from redness and discomfort. Applying chilled cucumber slices directly to irritated skin can provide instant comfort and reduce inflammation.
This makes cucumber a valuable ingredient for those with sensitive skin or conditions like eczema or rosacea.
Cucumber’s Ability to Reduce Puffiness and Dark Circles
The cooling and anti-inflammatory properties of cucumber make it an effective remedy for reducing puffiness and dark circles under the eyes. The high water content helps to de-puff the delicate skin around the eyes, while the antioxidants combat inflammation that can contribute to dark circles. The gentle application of cucumber slices or a cucumber-based eye mask can visibly reduce puffiness and improve the overall appearance of the under-eye area.
This is because the cool temperature constricts blood vessels, reducing swelling, and the antioxidants help to brighten the skin.
Various Ways to Use Cucumber for Skincare
Cucumber’s versatility makes it a valuable addition to a wide range of skincare applications. It’s easily incorporated into various homemade remedies and commercial products.
- Cucumber Masks: Pureed cucumber can be applied directly to the face as a mask, leaving the skin feeling refreshed and hydrated. Adding other ingredients like yogurt or honey can further enhance the benefits.
- Cucumber Toner: Cucumber juice, easily extracted by blending and straining cucumber, can be used as a natural toner to tighten pores and refresh the skin.
- Cucumber Eye Compresses: Chilled cucumber slices placed over the eyes can reduce puffiness and dark circles.
- Cucumber Face Wash: Blended cucumber can be incorporated into a homemade face wash for gentle cleansing and hydration.
- Cucumber Scrubs: Combining finely grated cucumber with other exfoliating ingredients can create a gentle facial scrub.
Honey’s Impact on Skin Tone and Texture
Honey, a natural sweetener, boasts remarkable properties that extend far beyond culinary uses. Its application in skincare is increasingly recognized for its ability to improve skin tone and texture, offering a gentle yet effective approach to achieving a healthier complexion. This stems from its unique composition, rich in antibacterial, antimicrobial, and humectant properties.
Honey’s Antibacterial and Antimicrobial Properties for Acne
Honey’s antibacterial and antimicrobial actions are largely attributed to its high sugar content, low water activity, and the presence of hydrogen peroxide and other bioactive compounds. These properties effectively combat acne-causing bacteria,Propionibacterium acnes*, reducing inflammation and preventing further breakouts. Studies have shown that applying honey topically can significantly reduce the severity of acne lesions, leading to clearer skin.
The effectiveness varies depending on the type of honey used, with some exhibiting stronger antimicrobial activity than others. For instance, Manuka honey, known for its high concentration of methylglyoxal, demonstrates particularly potent antibacterial effects.
Honey’s Humectant Properties and Moisture Retention
Honey acts as a natural humectant, meaning it attracts and retains moisture from the surrounding environment. This property is crucial for maintaining skin hydration, preventing dryness, and promoting a supple, healthy appearance. By drawing moisture into the skin, honey helps to plump up the complexion, reducing the appearance of fine lines and wrinkles. This moisturizing effect is particularly beneficial for individuals with dry or dehydrated skin, offering a natural alternative to harsh chemical-based moisturizers.
Honey’s Role in Wound Healing and Scar Reduction
Honey’s long history of use in wound healing is well-documented. Its ability to promote tissue regeneration and reduce inflammation contributes to faster healing times and minimized scarring. The antibacterial properties prevent infection, while the humectant properties keep the wound moist, promoting cell growth and reducing the risk of complications. Several studies have demonstrated honey’s effectiveness in treating various wounds, including burns and ulcers, highlighting its potential for scar reduction and improved skin texture.
The application of honey to minor skin abrasions can also facilitate faster healing and prevent the formation of unsightly scars.
Comparison of Honey Types for Skincare
The effectiveness of honey in skincare can vary depending on its type and origin. Different honeys possess varying concentrations of bioactive compounds, impacting their antibacterial, humectant, and overall skin benefits.
So, I’ve been really into this lemon, cucumber, and honey water for clearer skin – it’s amazing! The hydration boost is incredible, and I’ve noticed a real difference in my complexion. It’s fascinating how natural remedies can be so effective, especially when you consider the breakthroughs in medical science, like the recent news that the FDA approves clinical trials for pig kidney transplants in humans , which is pretty mind-blowing.
But back to my skin routine – this simple drink is a game-changer!
| Honey Type | Antibacterial Properties | Humectant Properties | Skin Benefits |
|---|---|---|---|
| Manuka Honey | High, due to high methylglyoxal content | Moderate to High | Effective against acne, wound healing, scar reduction |
| Raw Honey | Moderate, varies depending on floral source | Moderate | General skin hydration, mild acne treatment |
| Buckwheat Honey | Moderate to High | Moderate | Antioxidant properties, supports wound healing |
| Clover Honey | Low | Moderate | Gentle moisturizing, suitable for sensitive skin |
Recipe and Preparation of Lemon Cucumber Honey Water
This refreshing drink is surprisingly easy to make, requiring only a few simple ingredients and minimal effort. The precise quantities can be adjusted to your taste preferences, but the following recipe provides a good starting point for experiencing the benefits. Remember, consistency is key to seeing noticeable results for your skin.
This recipe Artikels the preparation of a single serving, easily scalable for larger quantities. Remember to always use fresh, high-quality ingredients for optimal results.
Ingredients and Quantities
The following ingredients are crucial for achieving the desired taste and skin benefits. Adjust the amounts to your liking, keeping in mind that less honey might be preferable for those watching their sugar intake.
- 1 cup (240ml) filtered water
- 1/2 medium cucumber, thinly sliced
- 1/4 lemon, juiced (approximately 1 tablespoon)
- 1 teaspoon honey (adjust to your sweetness preference)
Preparation Instructions, Benefits of lemon cucumber and honey water for clear skin
Follow these simple steps to prepare your invigorating lemon cucumber honey water. The process is quick and straightforward, allowing you to enjoy the benefits quickly.
- Combine the filtered water, cucumber slices, and lemon juice in a pitcher or jar.
- Stir gently to ensure the lemon juice is distributed evenly.
- Cover and refrigerate for at least 30 minutes to allow the flavors to meld. For a more intense flavor, refrigerate overnight.
- Before serving, add the honey and stir well until dissolved. Taste and adjust honey to your liking.
- Strain the mixture to remove the cucumber slices before drinking, if desired. Some prefer to leave the cucumber slices in for added texture and nutrients.
Tips for Optimizing Taste and Effectiveness
Several adjustments can enhance both the flavor and the potential benefits of this drink. Experiment with these suggestions to find your perfect blend.
- Use high-quality honey: Raw honey is preferred for its potential health benefits, and its distinct flavor adds complexity to the drink.
- Adjust sweetness: Start with a smaller amount of honey and add more to taste. You can also substitute with other natural sweeteners like agave or maple syrup.
- Experiment with variations: Add a few mint leaves for a refreshing twist, or a pinch of ginger for an extra kick.
- Consider the time of day: Drinking this in the morning can provide a hydrating and energizing start to your day.
Storage and Shelf Life
Proper storage is crucial to maintain the quality and freshness of your lemon cucumber honey water. Avoid leaving it at room temperature for extended periods.
Store the prepared water in an airtight container in the refrigerator. It is best consumed within 24-48 hours for optimal freshness and to minimize the risk of bacterial growth. After 48 hours, the drink may begin to lose its flavor and nutritional value.
Potential Side Effects and Precautions
While lemon cucumber honey water offers numerous skin benefits, it’s crucial to be aware of potential side effects and take necessary precautions to ensure safe and effective use. Overconsumption or individual sensitivities can lead to undesirable consequences, so moderation and awareness are key.Excessive consumption of this drink, particularly the lemon component, can have some drawbacks. It’s important to consider these factors before incorporating it into your daily routine.
Tooth Enamel Erosion
The high acidity of lemon juice can erode tooth enamel over time, leading to increased sensitivity and potential damage. Regular and prolonged exposure to citric acid weakens the protective layer of your teeth, making them more susceptible to cavities and discoloration. This is particularly true if you drink it frequently throughout the day or swish it around your mouth before swallowing.
To mitigate this risk, it’s recommended to drink the mixture through a straw to minimize contact with teeth, rinse your mouth with plain water afterward, and limit your daily intake. Consider waiting at least 30 minutes after drinking it before brushing your teeth to allow your saliva to neutralize the acid.
So, I’ve been really focusing on this lemon, cucumber, and honey water for clearer skin – it’s amazing! The hydration boost alone is worth it, but I’m also learning about the importance of holistic well-being. For example, I read a fascinating article on strategies to manage Tourette syndrome in children , highlighting how managing stress can impact overall health, including skin.
Getting enough sleep and managing stress are key, just like drinking plenty of this delicious, skin-loving water!
Allergic Reactions
Although rare, allergic reactions to lemon, cucumber, or honey are possible. Symptoms can range from mild skin rashes and itching to more severe reactions like swelling, difficulty breathing, or anaphylaxis. If you have a known allergy to any of these ingredients, avoid consuming this beverage. If you experience any adverse reactions after consuming the drink, discontinue use immediately and consult a doctor or allergist.
It’s always advisable to introduce new foods and drinks gradually to observe any potential allergic responses.
Precautions for Specific Skin Conditions
Individuals with certain skin conditions should exercise caution. For example, those with sensitive skin might experience irritation from the lemon’s acidity. A small patch test on a less sensitive area of skin before widespread use is recommended to assess tolerance. Those with acne-prone skin should use this drink in moderation, as the sugar content in honey could potentially exacerbate breakouts in some individuals.
Furthermore, people with existing gastrointestinal issues, such as acid reflux or ulcers, might find the acidity of the drink aggravates their condition. If you have any pre-existing health concerns, consult your doctor before regularly incorporating lemon cucumber honey water into your diet. Always prioritize listening to your body and adjusting your intake accordingly.
Illustrative Examples
Seeing is believing, and when it comes to skincare, results speak volumes. Let’s explore two hypothetical scenarios to illustrate the potential benefits – and potential limitations – of incorporating lemon cucumber honey water into your skincare routine. Remember, individual results may vary.These examples highlight the importance of consistency, proper usage, and understanding your skin’s unique needs. While this drink offers potential benefits, it’s not a miracle cure and shouldn’t replace other aspects of a healthy skincare regimen.
Successful Skin Transformation
Imagine Sarah, a 28-year-old with combination skin prone to occasional breakouts and dullness. Her skin texture was uneven, with enlarged pores on her nose and cheeks. Her skin tone appeared slightly uneven, with some areas appearing slightly darker than others. After consistently drinking a glass of lemon cucumber honey water daily for three months, Sarah noticed a significant improvement.
Her skin’s overall texture became smoother and more refined. The enlarged pores appeared less prominent, and her skin tone became more even and radiant. Her breakouts reduced significantly, and her complexion gained a healthy glow. Her skin’s clarity dramatically improved, with a noticeable reduction in blemishes and a more even skin tone. The overall improvement was a testament to the consistent hydration and the gentle exfoliating and brightening effects of the drink.
Lack of Improvement and Potential Negative Reactions
Now, consider Mark, a 35-year-old with sensitive skin who experienced no noticeable improvement after drinking lemon cucumber honey water for two months. He even experienced a slight increase in redness and irritation. This is likely due to the acidity of the lemon interacting negatively with his sensitive skin. Mark’s skin remained prone to dryness and flaking, and he didn’t observe any changes in his skin’s tone or texture.
In his case, the lemon’s acidity may have been too harsh for his sensitive skin, leading to irritation. This highlights the importance of understanding your skin type and potentially adjusting the recipe or discontinuing use if irritation occurs. For instance, he might have benefited from reducing the amount of lemon juice or diluting the drink further. Another contributing factor could be that he didn’t maintain a consistent skincare routine alongside the drink, which is crucial for optimal results.
Ultimate Conclusion: Benefits Of Lemon Cucumber And Honey Water For Clear Skin
So, there you have it – the amazing potential of lemon, cucumber, and honey water for clearer, healthier skin. While individual results may vary, incorporating this simple drink into your daily routine could be a game-changer. Remember to listen to your body, be patient, and enjoy the refreshing taste while you work towards that radiant glow. Cheers to healthy skin!
Query Resolution
Can I drink this every day?
Yes, but moderation is key. Too much lemon can erode tooth enamel. Rinse your mouth with plain water after drinking.
How long does it take to see results?
Results vary, but many see improvements in skin tone and clarity within a few weeks of consistent consumption.
What if I’m allergic to honey?
If you have a honey allergy, this drink isn’t suitable for you. Consider alternatives like aloe vera juice or green tea.
Can I use this if I have sensitive skin?
Start with a small amount to test for any reactions. If you experience irritation, discontinue use.
