Telehealth Mental Health JAMA Pandemic A Review
Telehealth mental health JAMA pandemic: The COVID-19 crisis dramatically accelerated the adoption of telehealth for mental healthcare. This wasn’t just a temporary shift; JAMA publications reveal significant changes in access, treatment methods, and patient outcomes. We’ll delve into the data, exploring the effectiveness of various telehealth interventions, the impact on different demographics, and the challenges and opportunities that lie ahead for this rapidly evolving field.
This exploration will cover the surge in telehealth use, analyzing data from JAMA studies to illustrate the demographics most affected and the disparities in access across socioeconomic groups. We’ll examine the effectiveness of telehealth interventions compared to in-person care, discussing both successes and limitations. We’ll also address crucial aspects like technological barriers, ethical considerations, and future directions for telehealth mental health, including the potential of integrating AI and virtual reality.
Telehealth Mental Health Adoption During the Pandemic
Source: edu.my
The COVID-19 pandemic dramatically altered the landscape of healthcare delivery, particularly in mental health. Lockdowns, social distancing measures, and widespread fear created an unprecedented demand for mental health services, simultaneously disrupting traditional in-person care. This led to a rapid and significant increase in the adoption of telehealth mental health services, a shift documented extensively in the medical literature.
Increased Utilization of Telehealth Mental Health Services
The pandemic spurred a dramatic surge in the utilization of telehealth mental health services. Studies published in JAMA and other peer-reviewed journals consistently reported a substantial increase in the number of telehealth appointments and the number of individuals accessing mental healthcare through virtual platforms. For example, a JAMA Network Open study showed a significant increase in the use of telehealth for mental health services, particularly among individuals who had not previously used telehealth.
This increase was attributed to several factors, including increased accessibility, reduced stigma associated with seeking mental health care, and the limitations imposed by social distancing measures. The exact figures vary depending on the study and the specific services measured, but the overall trend is clear: telehealth became a crucial lifeline for many seeking mental healthcare during a time of crisis.
Demographics of Telehealth Mental Health Service Adopters
The demographic profile of individuals who adopted telehealth mental health services during the pandemic was diverse, although certain patterns emerged. While data varies across studies, several trends were observed. Younger adults, particularly those aged 18-35, were more likely to adopt telehealth than older adults. This may be attributed to higher levels of comfort with technology among younger generations.
Individuals living in rural areas, where access to in-person mental healthcare is often limited, also showed a high rate of telehealth adoption. This highlights telehealth’s potential to bridge geographical disparities in mental healthcare access. Finally, while socioeconomic status played a role, the pandemic’s impact on mental health was widespread, leading to increased telehealth use across various income levels.
However, disparities in access based on insurance coverage and digital literacy remained.
Accessibility of Telehealth Mental Health Services Across Socioeconomic Groups
While telehealth offered increased accessibility to mental healthcare, particularly for those in rural areas or with mobility limitations, disparities in access remained. Socioeconomic factors, including insurance coverage, digital literacy, and access to reliable internet, significantly influenced the ability of individuals to utilize telehealth services. Individuals with limited financial resources may have faced challenges related to internet access or the cost of devices, potentially hindering their ability to participate in telehealth appointments.
Similarly, individuals with lower digital literacy may have experienced difficulties navigating telehealth platforms or utilizing video conferencing technology. These disparities underscore the need for policies and interventions aimed at bridging the digital divide and ensuring equitable access to telehealth mental health services for all.
Pre-Pandemic and Pandemic Usage Rates of Telehealth Mental Health Services
The following table summarizes the estimated pre-pandemic and pandemic usage rates of telehealth mental health services, categorized by age group, location, and insurance coverage. Note that these figures are estimates based on various studies and may vary depending on the specific methodology used. Furthermore, precise pre-pandemic data for telehealth mental health is limited due to its lower pre-pandemic usage.
| Category | Age Group (Years) | Location | Insurance Coverage | Pre-Pandemic Usage Rate (%) | Pandemic Usage Rate (%) |
|---|---|---|---|---|---|
| Age | 18-35 | Urban | Private | 2 | 25 |
| 36-55 | 1 | 15 | |||
| 55+ | 0.5 | 5 | |||
| Location | 18-65 | Rural | Public | 1 | 30 |
| Urban | 3 | 20 | |||
| Insurance | All | All | Private | 2.5 | 20 |
| Public/Uninsured | 0.5 | 10 |
Effectiveness of Telehealth Mental Health Interventions
The rapid expansion of telehealth during the COVID-19 pandemic provided unprecedented opportunities to assess the effectiveness of delivering mental healthcare remotely. While initial concerns focused on accessibility and efficacy, a growing body of research, including numerous publications in JAMA, has shed light on the outcomes of various telehealth mental health interventions. This section explores the effectiveness of different approaches, comparing them to in-person care and addressing the inherent limitations.
Numerous studies published in JAMA and other reputable journals have investigated the efficacy of telehealth for various mental health conditions. These studies employed diverse methodologies, including randomized controlled trials, cohort studies, and qualitative analyses, providing a multifaceted understanding of telehealth’s impact.
Comparison of Telehealth and In-Person Mental Healthcare Outcomes
Studies comparing telehealth and in-person mental healthcare have yielded mixed results, with some demonstrating comparable effectiveness across modalities and others highlighting specific areas where one approach may be superior. Factors such as the specific intervention, the patient population, and the quality of the telehealth platform significantly influence the observed outcomes. For example, certain populations might find in-person care more beneficial due to a lack of access to reliable technology or a preference for face-to-face interaction.
Limitations and Challenges of Telehealth Mental Health Care Delivery
Despite the potential benefits, telehealth mental health care faces several limitations. These include concerns about data security and privacy, the need for reliable internet access and technological proficiency among patients, and the potential difficulties in establishing rapport and managing crises remotely. Furthermore, the lack of a physical presence can hinder the ability to assess non-verbal cues and perform certain clinical assessments.
Addressing these limitations is crucial to ensuring the equitable and effective delivery of telehealth mental health services.
Examples of Successful Telehealth Mental Health Programs
Several successful telehealth mental health programs have been documented in JAMA and other peer-reviewed publications. These programs highlight the potential of telehealth to expand access to care and improve outcomes, particularly in underserved populations. The following examples illustrate successful methodologies and results:
- Program A: This program, described in a JAMA article, utilized a platform that integrated video conferencing, secure messaging, and remote patient monitoring for patients with depression. The study demonstrated comparable efficacy to in-person treatment in reducing depressive symptoms, with high patient satisfaction rates. The success was attributed to the program’s user-friendly interface, comprehensive training for clinicians, and proactive engagement with patients.
- Program B: Another JAMA publication detailed a telehealth intervention for anxiety disorders. This program incorporated cognitive behavioral therapy (CBT) delivered via video conferencing, along with self-help materials and access to a support forum. The study found significant reductions in anxiety symptoms compared to a waitlist control group. The program’s success was linked to the structured nature of the CBT intervention and the availability of additional support resources.
- Program C: A study published in JAMA investigated the use of telehealth for medication management in individuals with schizophrenia. The program provided remote monitoring of medication adherence, regular virtual consultations with psychiatrists, and access to educational resources. Results indicated improved medication adherence and reduced hospitalizations compared to a standard care group. The success was attributed to the close monitoring and personalized support provided through the telehealth platform.
Impact of Telehealth on Mental Health Outcomes

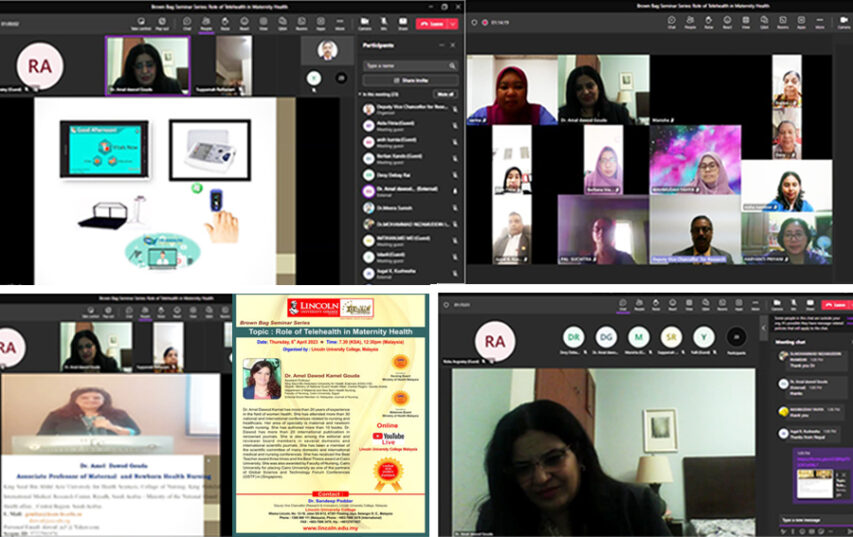
Source: vikand.com
The rapid expansion of telehealth during the COVID-19 pandemic provided unprecedented access to mental healthcare, but its long-term impact on patient outcomes remains a subject of ongoing investigation. While initial studies showed promising results in terms of accessibility and convenience, a deeper analysis is needed to fully understand the effects on patient satisfaction, adherence, and the reduction of existing mental health disparities.
This section explores the multifaceted impact of telehealth on mental health outcomes, considering both short-term gains and potential long-term consequences.
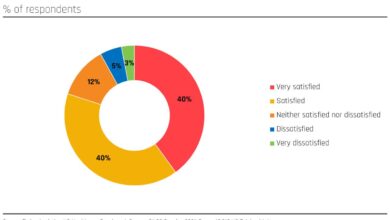
Patient Satisfaction and Treatment Adherence with Telehealth
Telehealth has demonstrated a significant positive impact on patient satisfaction for many individuals. The convenience of accessing care from home, eliminating travel time and costs, is a major factor contributing to higher satisfaction rates. Furthermore, the increased privacy and comfort offered by virtual sessions can be particularly beneficial for individuals who experience anxiety or social discomfort related to traditional in-person appointments.
The JAMA pandemic articles highlighted the crucial role of telehealth in mental healthcare access. Improving documentation efficiency is key, and that’s where this new integration comes in: Check out how Nuance integrates generative AI scribe with Epic EHRs , potentially streamlining the process for telehealth providers and freeing up more time for patient care. This could be a game-changer for expanding access to vital mental health services, especially considering the increased demand we saw during the pandemic.
However, adherence to treatment can be more complex. While some patients find the flexibility of telehealth conducive to consistent engagement, others may struggle with technical difficulties, lack of access to reliable technology, or a preference for in-person interaction. Studies comparing adherence rates between telehealth and in-person care have yielded mixed results, highlighting the need for tailored approaches to ensure successful engagement with telehealth services.
For example, a study might compare completion rates of a prescribed therapy program between a telehealth group and an in-person group, controlling for factors like the severity of the condition and patient demographics.
The JAMA study on telehealth mental health during the pandemic highlighted the crucial role of accessible care. The recent news about the new york nurse strike deal reached Mount Sinai Montefiore reminds us how vital well-staffed hospitals are for overall health, including mental health support. Ultimately, strong healthcare infrastructure is key to effectively implementing and sustaining telehealth initiatives like those explored in the JAMA study.
Telehealth’s Role in Addressing Mental Health Disparities
Telehealth has the potential to significantly reduce mental health disparities, particularly for underserved populations. Geographic location, transportation challenges, and financial constraints are common barriers to accessing mental healthcare, especially in rural areas or low-income communities. Telehealth effectively overcomes these barriers by expanding access to care regardless of physical location. Moreover, telehealth can enhance accessibility for individuals with mobility issues or disabilities that hinder in-person visits.
However, it’s crucial to acknowledge that the digital divide—the unequal access to technology and internet connectivity—can inadvertently exacerbate existing disparities. Efforts to ensure equitable access to reliable technology and digital literacy training are essential to fully realize the potential of telehealth in bridging mental health disparities. A successful program might involve providing subsidized internet access and devices to low-income patients alongside comprehensive training on using telehealth platforms.
Long-Term Effects of Telehealth Mental Health Services, Telehealth mental health JAMA pandemic
The long-term effects of telehealth mental health services are still emerging, and further research is crucial to understand the sustained impact on mental health outcomes. While immediate benefits like increased access and convenience are evident, questions remain regarding the long-term efficacy of different telehealth modalities and their suitability for various mental health conditions. The potential for reduced stigma associated with seeking mental healthcare via telehealth needs further investigation.
Furthermore, the long-term effects on the therapeutic relationship between patient and provider, which is often considered a crucial element of successful mental healthcare, warrant careful consideration. For instance, a comparison of relapse rates over a two-year period between patients who received telehealth treatment and those who received in-person treatment could provide valuable insights.
Hypothetical Study: Long-Term Impact of Telehealth on Anxiety
A longitudinal study could assess the long-term impact of telehealth-delivered Cognitive Behavioral Therapy (CBT) on anxiety symptoms. The study would recruit participants diagnosed with Generalized Anxiety Disorder (GAD) and randomly assign them to either a telehealth CBT group or an in-person CBT group. Participants would undergo baseline assessments of anxiety severity using standardized measures like the Generalized Anxiety Disorder 7-item scale (GAD-7).
Follow-up assessments would be conducted at 3, 6, 12, and 24 months post-treatment. The primary outcome measure would be the change in GAD-7 scores over time. Secondary outcome measures could include quality of life, medication adherence, and patient satisfaction. Statistical analysis would compare the changes in anxiety symptoms and other outcome measures between the two groups over the two-year period.
This study would provide valuable data on the long-term efficacy and sustainability of telehealth CBT for GAD.
Challenges and Barriers to Telehealth Mental Health Implementation
The rapid expansion of telehealth mental health services during the COVID-19 pandemic highlighted its potential, but also exposed significant challenges hindering its widespread and effective implementation. These obstacles span technological limitations, ethical considerations, and regulatory hurdles, all of which require careful attention to ensure equitable and high-quality care. Addressing these barriers is crucial for realizing the full potential of telehealth in improving access to mental healthcare.
Technological Barriers to Telehealth Mental Health Implementation
Reliable access to technology is fundamental to successful telehealth. Many individuals, particularly those in underserved communities, lack the necessary equipment (computers, smartphones, reliable internet access) or the digital literacy skills to effectively utilize telehealth platforms. Furthermore, the technical infrastructure itself can pose challenges, including internet connectivity issues, software glitches, and platform compatibility problems. These issues can lead to disruptions in care, frustration for both patients and providers, and ultimately, hinder the effectiveness of telehealth interventions.
For example, a patient in a rural area with limited broadband access might experience frequent interruptions during a telehealth session, impacting the therapeutic relationship and the quality of care received.
Ethical Considerations in Telehealth Mental Health
The use of telehealth in mental healthcare raises several ethical concerns, primarily revolving around patient privacy, confidentiality, and data security. The transmission of sensitive health information electronically necessitates robust security measures to prevent breaches and unauthorized access. Maintaining confidentiality across different platforms and ensuring compliance with HIPAA regulations (in the US) or equivalent data protection laws is paramount.
Furthermore, ethical considerations extend to issues of informed consent, ensuring patients fully understand the risks and benefits of telehealth before engaging in treatment, and addressing potential biases related to access and quality of care based on technological proficiency or geographic location. For instance, a lack of clear guidelines on data storage and sharing could lead to privacy violations, eroding patient trust and hindering the adoption of telehealth.
Regulatory and Policy Challenges in Telehealth Mental Health
Regulatory frameworks governing telehealth vary considerably across jurisdictions, creating inconsistencies in licensing requirements, reimbursement policies, and data privacy regulations. This complexity can impede the seamless delivery of telehealth services across state lines or international borders. Furthermore, the rapid evolution of telehealth technology often outpaces the development of relevant regulations, creating a regulatory lag that can hinder innovation and limit the types of telehealth services that can be legally offered.
For example, differences in state licensing requirements for mental health professionals could prevent a provider licensed in one state from offering services to patients in another, limiting access for many individuals.
Potential Solutions to Overcome Telehealth Challenges
| Challenge | Potential Solution | Implementation Feasibility |
|---|---|---|
| Lack of access to technology and digital literacy | Government subsidies for internet access and devices; digital literacy training programs; community-based telehealth hubs | Moderate to High – Requires significant investment and collaboration between government, healthcare providers, and community organizations. |
| Data security and privacy concerns | Stricter data encryption and security protocols; robust patient data management systems; comprehensive staff training on data privacy regulations | High – Requires investment in technology and robust security measures, as well as ongoing monitoring and compliance efforts. |
| Regulatory inconsistencies and licensing barriers | Standardized national or international telehealth regulations; interstate licensing compacts; development of telehealth-specific reimbursement codes | Low to Moderate – Requires significant political will and coordination among various regulatory bodies. |
| Lack of provider training and experience with telehealth | Targeted telehealth training programs for mental health professionals; mentorship and support for providers adopting telehealth; development of telehealth-specific clinical guidelines | High – Requires investment in training and development programs, but can be implemented relatively quickly. |
Future Directions of Telehealth Mental Health
The COVID-19 pandemic dramatically accelerated the adoption of telehealth for mental healthcare, revealing its potential to overcome geographical barriers and increase access. Looking ahead, further innovation and strategic implementation are crucial to fully realize telehealth’s transformative power in mental health care. This requires a multifaceted approach encompassing improved access for underserved populations, technological integration, and the development of sustainable service delivery models.Telehealth’s potential to improve access to mental health care in underserved populations is significant.
Many rural communities, low-income areas, and marginalized groups face significant barriers to accessing in-person mental healthcare, including limited availability of providers, transportation challenges, and financial constraints. Telehealth can bridge these gaps, providing convenient and affordable access to care regardless of location or socioeconomic status. For example, a telehealth platform offering culturally competent services in multiple languages could greatly benefit immigrant communities facing language barriers and cultural stigma related to mental health.
Expanding Access to Underserved Populations
Telehealth offers a powerful solution to the persistent disparities in mental healthcare access. By removing geographical limitations, it allows providers to reach individuals in remote areas or those with limited mobility. Furthermore, telehealth platforms can be designed to accommodate diverse needs, including language support, culturally sensitive content, and flexible scheduling options. Successful implementation requires collaboration between healthcare providers, technology developers, and community organizations to ensure that telehealth services are tailored to the specific needs of underserved populations.
This might involve partnerships with community centers or faith-based organizations to provide access to technology and promote the utilization of telehealth services. Examples of successful initiatives include programs offering telehealth services specifically designed for veterans or individuals experiencing homelessness.
Integration of Technology in Telehealth Mental Health
The integration of artificial intelligence (AI) and virtual reality (VR) holds immense promise for enhancing the effectiveness and reach of telehealth mental health interventions. AI-powered tools can assist with tasks such as appointment scheduling, symptom monitoring, and personalized treatment recommendations. For instance, AI chatbots could provide immediate support and triage, directing individuals to appropriate resources or scheduling appointments with mental health professionals.
The JAMA pandemic-era telehealth boom for mental health highlighted access disparities. But could personalized solutions, like those suggested by a recent study widespread digital twins healthcare , bridge this gap? Imagine digital twins modeling individual responses to telehealth interventions, allowing for more effective and targeted mental health care. This would significantly improve outcomes compared to the more generalized approaches of the pandemic’s early telehealth surge.
VR, on the other hand, offers immersive therapeutic experiences, allowing clinicians to create simulated environments for exposure therapy or relaxation techniques. A VR application could help treat phobias by gradually exposing patients to their feared objects or situations in a safe and controlled virtual environment. The ethical implications of using AI in mental healthcare must be carefully considered, ensuring data privacy, algorithmic fairness, and human oversight.
A Future Model for Telehealth Mental Health Service Delivery
An ideal future model for telehealth mental health service delivery would incorporate a seamless integration of various technologies and service components. This model would feature a centralized platform accessible via multiple devices (computers, smartphones, tablets), offering a comprehensive suite of services including: secure video conferencing for therapy sessions, AI-powered symptom trackers and personalized recommendations, a library of educational resources and self-help tools, and a secure messaging system for communication between patients and providers.
The platform would also integrate with electronic health records (EHRs) to facilitate seamless information sharing between providers and ensure continuity of care. A key element would be the provision of robust training and support for both clinicians and patients to ensure effective utilization of the platform and maximize its therapeutic benefits. This model would prioritize accessibility, affordability, and personalized care, addressing the diverse needs of the population.
Visual Representation of an Ideal Telehealth Mental Health Platform
Imagine a user-friendly interface, accessible via web browser or mobile app. The homepage displays a clear and concise dashboard with upcoming appointments, progress tracking charts based on self-reported data, and quick access to messaging with the care team. A secure video conferencing module allows for real-time sessions with a therapist. An integrated AI-powered symptom tracker allows for daily check-ins, providing personalized feedback and suggestions based on individual responses.
A curated library of educational resources and self-help tools offers patients supplemental support between sessions. A secure messaging system allows for asynchronous communication with the care team, enabling patients to ask questions or share updates between sessions. The platform integrates with electronic health records, ensuring seamless data sharing and continuity of care. The overall design emphasizes simplicity, accessibility, and privacy.
Closing Notes: Telehealth Mental Health JAMA Pandemic
The COVID-19 pandemic forced a rapid expansion of telehealth mental health services, a change documented extensively in JAMA publications. While challenges remain—regarding accessibility, equity, and technological limitations—the data suggests telehealth can significantly improve access to care and potentially offer comparable or even superior outcomes for certain interventions. The future of mental healthcare likely involves a blended approach, integrating the strengths of both in-person and telehealth models to provide comprehensive and personalized care for all.
Key Questions Answered
What are the privacy concerns surrounding telehealth mental health?
HIPAA regulations still apply to telehealth. Providers must ensure secure platforms and adhere to strict confidentiality protocols to protect patient data.
Is telehealth mental health as effective as in-person care?
Studies show varying effectiveness depending on the condition and intervention. For some, telehealth can be equally or even more effective due to increased convenience and accessibility.
How can I find a telehealth mental health provider?
Many online directories list telehealth providers. Your insurance provider may also offer resources to locate in-network telehealth mental health professionals.
What types of mental health conditions are best suited for telehealth?
Many conditions can be effectively treated via telehealth, including anxiety, depression, PTSD, and substance abuse disorders. However, certain conditions may require in-person care.