UnitedHealth Prior Authorization Gastroenterology Plan
Navigating the UnitedHealth prior authorization gastroenterology plan can feel like trekking through a dense jungle, but fear not! This post aims to shed light on this often-confusing process, breaking down the complexities and offering practical tips to help you get the care you need. We’ll explore everything from understanding your plan’s coverage to successfully appealing a denied authorization, ultimately empowering you to advocate for your health.
From deciphering the jargon to understanding the steps involved in submitting a prior authorization request, we’ll cover the essential aspects of interacting with UnitedHealthcare for gastroenterology services. We’ll also delve into strategies for managing costs and finding in-network providers, making the entire process smoother and less stressful. Think of this as your personal guide to conquering the UnitedHealth gastroenterology authorization maze.
UnitedHealthcare Gastroenterology Plans
Navigating the world of health insurance can be confusing, especially when dealing with specialized care like gastroenterology. UnitedHealthcare offers a range of plans, each with its own level of coverage and cost-sharing. Understanding these differences is crucial for making informed decisions about your healthcare. This post aims to clarify the key features of several UnitedHealthcare gastroenterology plans.
UnitedHealthcare Gastroenterology Plan Overview
UnitedHealthcare provides various plans catering to different needs and budgets. These plans often fall under broader categories like HMO (Health Maintenance Organization), PPO (Preferred Provider Organization), and POS (Point of Service) plans. Each type impacts how you access care and what you pay. HMO plans typically require you to see doctors within their network, while PPO plans offer more flexibility but usually come with higher costs for out-of-network care.
POS plans offer a blend of both. Specific gastroenterology coverage details will vary depending on the specific plan you choose and your location. Always refer to your plan’s Summary of Benefits and Coverage (SBC) for the most accurate and up-to-date information.
Common Gastroenterology Procedures and Coverage
Many common gastroenterology procedures are typically covered under UnitedHealthcare plans, but the extent of coverage and cost-sharing will depend on the specifics of your plan. Examples include colonoscopies (routine screenings and diagnostic), endoscopies (upper and lower), biopsies, and treatment for conditions like GERD (gastroesophageal reflux disease), Crohn’s disease, and ulcerative colitis. However, pre-authorization may be required for certain procedures, so it’s essential to check with your plan and provider beforehand.
Some experimental or cutting-edge procedures may not be covered, even under comprehensive plans.
Comparison of Three UnitedHealthcare Gastroenterology Plans
The following table compares three hypothetical UnitedHealthcare gastroenterology plans to illustrate the differences in cost-sharing. Remember, these are examples, and actual plans and costs will vary based on your location, plan specifics, and the network of providers. Always check your plan documents for the precise details.
| Plan Type | Deductible | Copay (Office Visit) | Out-of-Pocket Maximum |
|---|---|---|---|
| Example HMO Plan A | $1,000 | $40 | $5,000 |
| Example PPO Plan B | $2,000 | $60 (in-network), $100 (out-of-network) | $7,500 |
| Example POS Plan C | $1,500 | $50 (in-network), $80 (out-of-network) | $6,000 |
Prior Authorization Process for Gastroenterology Services
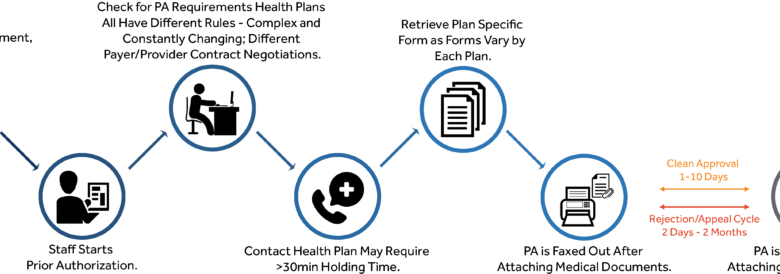
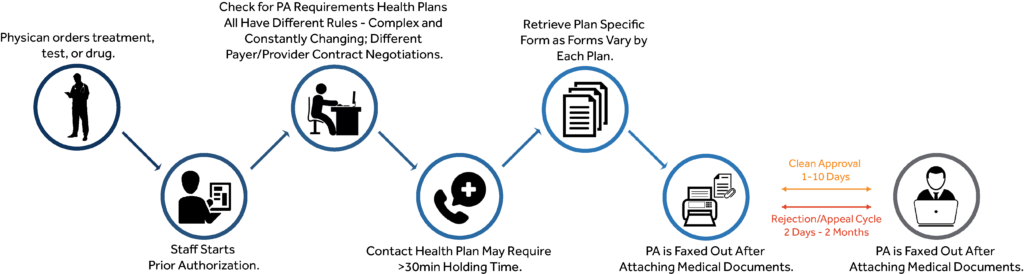
Source: simplifypriorauth.ca
Navigating the prior authorization process for gastroenterology services with UnitedHealthcare can feel overwhelming, but understanding the steps involved can significantly streamline the process and ensure timely access to necessary care. This guide Artikels the key steps, required documentation, and a visual representation of the process to help you prepare.
The prior authorization process is designed to ensure that the services you receive are medically necessary and appropriately cost-effective. While it might seem like an extra hurdle, it’s a crucial part of managing healthcare costs and ensuring quality of care. By providing complete and accurate documentation upfront, you can expedite the review and approval process.
Required Documentation for Prior Authorization Requests
Submitting a complete application is essential for a smooth and efficient prior authorization process. Missing or incomplete information can lead to delays. The required documentation typically includes, but is not limited to, the following:
The specific requirements can vary depending on the procedure or service requested. It’s always best to check with your provider and UnitedHealthcare directly to confirm the exact documentation needed for your specific case. Proactive communication is key.
- Patient Information: This includes the patient’s name, date of birth, address, phone number, and UnitedHealthcare member ID number.
- Physician Information: The referring physician’s name, address, phone number, and NPI (National Provider Identifier) number.
- Procedure/Service Information: A clear and concise description of the requested procedure or service, including the CPT (Current Procedural Terminology) code.
- Medical Necessity Justification: Detailed medical records supporting the medical necessity of the requested service. This might include the patient’s history, physical examination findings, diagnostic test results (lab reports, imaging studies), and progress notes. The documentation should clearly demonstrate why the requested service is medically necessary and appropriate for the patient’s condition.
- Prior Authorization Form: The completed and signed prior authorization form provided by UnitedHealthcare. This form typically includes sections for patient demographics, procedure details, and physician justification.
Prior Authorization Process Flowchart, Unitedhealth prior authorization gastroenterology plan
A visual representation can simplify understanding of the steps involved. Imagine a flowchart with the following stages:
The flowchart would begin with ” Physician Submits Prior Authorization Request” and then branch into ” UnitedHealthcare Receives Request“. Next, a decision point: ” Complete and Accurate Documentation?” If yes, it leads to ” Request Approved” and then ” Procedure Scheduled“. If no, it leads to ” Request Denied/Incomplete” followed by ” Physician Provided Additional Information” which loops back to ” UnitedHealthcare Receives Request“. Finally, the process concludes with ” Procedure Scheduled (if approved)“.
Network Providers and Specialists
Finding the right gastroenterologist within the UnitedHealthcare network is crucial for ensuring your services are covered and you receive the best possible care. This involves understanding how to effectively utilize the resources provided by UnitedHealthcare to locate in-network providers near you and verifying their participation in your specific plan.Navigating the UnitedHealthcare provider directory is straightforward and offers several tools to streamline your search.
The website provides a user-friendly interface that allows you to filter your search by specialty (gastroenterology), location (zip code, city, state), and even specific services offered. This ensures you find a provider who meets your individual needs and accepts your UnitedHealthcare plan.
Locating In-Network Gastroenterologists
The UnitedHealthcare website is the primary resource for finding in-network gastroenterologists. Their online provider directory allows you to search by location (using zip code, city, or state), and then filter the results by specialty, selecting “Gastroenterology.” You can further refine your search by specifying additional criteria such as language spoken, gender, and whether the provider accepts new patients.
Navigating the UnitedHealth prior authorization gastroenterology plan can feel like a maze, but imagine a future where AI streamlines the process. This is where the news about nuance integrates generative ai scribe epic ehrs becomes relevant; faster documentation could mean quicker approvals. Ultimately, this type of technological advancement could significantly reduce the headaches associated with UnitedHealth’s prior authorization procedures for gastroenterology services.
The results will display a list of gastroenterologists within your chosen area, along with their contact information, office addresses, and, importantly, confirmation of their participation in your specific UnitedHealthcare plan.
Utilizing UnitedHealthcare’s Online Tools
UnitedHealthcare provides several online tools to simplify the process of finding in-network providers. The most important is their online provider directory, accessible directly through their website. This directory allows for sophisticated searches based on location, specialty, and other relevant criteria. In addition to the directory, UnitedHealthcare’s website often features FAQs, articles, and videos that guide members through the process of finding and selecting a provider.
These supplementary resources provide additional support and answer common questions related to provider selection.
Frequently Asked Questions Regarding In-Network Provider Access
Understanding the nuances of in-network access is vital. The following points address common concerns:
- Question: What happens if I see an out-of-network provider? Answer: Seeing an out-of-network provider will likely result in higher out-of-pocket costs. Your plan may cover some portion of the services, but your responsibility for payment will be significantly greater than if you used an in-network provider.
- Question: How often is the provider directory updated? Answer: UnitedHealthcare regularly updates its provider directory to reflect changes in network participation. It is always recommended to verify a provider’s in-network status immediately before scheduling an appointment.
- Question: Can I change my in-network provider? Answer: Yes, you can change your provider at any time. Simply find a new in-network provider using the online directory and schedule your appointments accordingly.
- Question: What if my preferred gastroenterologist is not in the network? Answer: If your preferred gastroenterologist is out-of-network, you may want to explore options like requesting a referral to an in-network specialist or considering alternative providers within the network who offer similar services.
Appealing a Denied Prior Authorization
Getting a prior authorization denied can be frustrating, especially when you need timely access to gastroenterology services. However, UnitedHealthcare provides an appeals process to review denials and ensure you receive the care you need. Understanding this process and preparing your appeal effectively increases your chances of a successful outcome.The procedure for appealing a denied prior authorization involves submitting a detailed appeal to UnitedHealthcare within the specified timeframe Artikeld in your denial letter.
This timeframe is crucial; missing the deadline can result in the appeal being rejected. The appeal should clearly state your disagreement with the initial decision and provide compelling evidence supporting the medical necessity of the requested service. This process often involves interacting with both your physician’s office and UnitedHealthcare’s appeals department.
Necessary Documentation for an Appeal
Supporting your appeal with comprehensive documentation is vital. A poorly documented appeal is significantly less likely to be successful. The necessary documentation generally includes, but isn’t limited to, the original prior authorization request, the denial letter, and detailed medical records relevant to the requested service. These records should clearly demonstrate the medical necessity of the procedure or treatment, highlighting the diagnosis, treatment plan, and the expected benefits for the patient.
Supporting statements from your physician explaining the rationale behind the requested service and why alternative treatments are inadequate are also highly beneficial. Copies of any relevant peer-reviewed medical literature that supports the prescribed treatment can further strengthen your appeal.
Examples of Successful Appeal Strategies
A successful appeal often hinges on clearly demonstrating the medical necessity of the requested service and the lack of suitable alternatives. For instance, an appeal for a specific, advanced endoscopic procedure might be successful if the appeal documents demonstrate that less invasive methods have been tried and failed, and that the requested procedure offers a significantly better chance of a successful outcome, minimizing risks and improving the patient’s quality of life.
Another example might involve a case where a patient requires a specialized medication not covered by the standard formulary. A successful appeal would need to show that the requested medication is medically necessary due to the patient’s unique condition and that alternative medications have proven ineffective or have unacceptable side effects. In both cases, detailed medical records, physician statements, and possibly supporting literature from reputable medical journals would significantly strengthen the appeal.
It is important to meticulously review the denial reason and tailor the appeal to directly address those specific concerns.
Cost Considerations and Financial Planning
Navigating the financial aspects of gastroenterology care can be daunting, especially when dealing with insurance coverage like UnitedHealthcare. Understanding your plan’s specifics, potential out-of-pocket costs, and available financial assistance programs is crucial for effective budgeting and managing expenses. This section will explore strategies to help you plan for and manage the financial burden of gastroenterology treatment.Understanding your out-of-pocket expenses is the first step towards effective financial planning.
This includes deductibles, co-pays, and coinsurance. Many UnitedHealthcare plans offer different levels of coverage, impacting your overall costs. Actively researching your specific plan details and understanding your responsibility for payment is vital. You should also consider the potential need for additional services, such as medications, follow-up appointments, and potential hospital stays, which can significantly impact your total cost.
Navigating UnitedHealthcare’s prior authorization process for gastroenterology can be a real headache, especially when dealing with complex cases. I recently stumbled upon a fascinating article, study widespread digital twins healthcare , which got me thinking about how digital twins could streamline this whole process. Imagine a system that automatically pre-approves treatments based on a patient’s digital twin, eliminating much of the paperwork involved with UnitedHealth’s prior authorization for gastroenterology plans.
That would be a game changer!
Estimating Costs for Common Gastroenterology Procedures and Services
Creating a realistic budget requires anticipating the costs associated with various gastroenterology services. The following sample budget Artikels potential expenses, but remember that actual costs can vary based on your specific plan, location, and the complexity of your care. It’s always best to contact your provider and UnitedHealthcare directly for personalized cost estimates.
| Procedure/Service | Estimated Cost Range | Notes |
|---|---|---|
| Colonoscopy | $1,000 – $3,000 | This range varies significantly depending on anesthesia, facility fees, and the complexity of the procedure. |
| Endoscopy | $800 – $2,500 | Similar to colonoscopy, costs depend on the type of endoscopy, anesthesia, and facility fees. |
| Medication (e.g., PPI) | $50 – $200 per month | The cost of prescription medications can vary greatly depending on the specific medication and your pharmacy. |
| Office Visit | $100 – $250 | The cost of a routine office visit depends on the provider and location. |
This is just a sample; costs can vary widely depending on your specific situation. Always obtain detailed cost estimates from your provider and UnitedHealthcare before undergoing any procedure.
Comparing the Cost-Effectiveness of Different UnitedHealthcare Gastroenterology Plans
UnitedHealthcare offers various gastroenterology plans, each with different levels of coverage and cost-sharing responsibilities. Comparing these plans requires a careful analysis of several factors. Consider the premium costs, deductibles, co-pays, coinsurance, and out-of-pocket maximums. A plan with a lower premium might have a higher deductible, leading to higher out-of-pocket expenses if you need extensive care. Conversely, a plan with a higher premium may offer lower out-of-pocket costs.For example, a “high-deductible” plan might have a lower monthly premium but a much higher deductible that you must meet before the insurance company begins to cover a significant portion of your costs.
A “low-deductible” plan may have a higher monthly premium but lower out-of-pocket costs once the deductible is met. Your individual needs and anticipated healthcare usage will determine which plan is most cost-effective for you. It is crucial to carefully weigh these factors to select the plan that best aligns with your budget and healthcare needs. Contacting UnitedHealthcare directly for plan comparisons and detailed explanations is highly recommended.
Understanding Plan Benefits and Exclusions
Navigating the world of health insurance can be confusing, especially when it comes to understanding exactly what your plan covers. This section clarifies the benefits and exclusions related to gastroenterology services under various UnitedHealthcare plans. Remember that specific coverage details depend heavily on your individual plan type, so always refer to your policy documents for the most accurate information.Understanding the specifics of your UnitedHealthcare gastroenterology plan is crucial for managing healthcare costs and ensuring you receive the necessary care.
This involves knowing what procedures, tests, and medications are covered, as well as what might be excluded or require prior authorization. Failing to understand these details can lead to unexpected out-of-pocket expenses.
Preventative Care Coverage
Preventative gastroenterology services, designed to detect potential problems early, are often covered at a higher rate or even fully covered under many UnitedHealthcare plans. This is in line with the overall healthcare trend of emphasizing proactive health management. These services aim to prevent more serious and costly issues down the line.Examples of preventative services typically covered include routine colonoscopies (within the recommended screening guidelines), and possibly fecal immunochemical tests (FIT) for colorectal cancer screening.
The specific age and frequency requirements for these screenings will vary based on your individual risk factors and your plan’s guidelines. It is important to confirm these details with your provider and your UnitedHealthcare plan administrator.
Treatment Coverage for Gastroenterological Issues
Treatment for diagnosed gastroenterological conditions typically falls under the umbrella of medical necessity. Coverage for these treatments varies widely depending on the specific condition, the type of treatment, and the plan’s benefit structure. Some plans might offer extensive coverage for treatments such as endoscopies, while others may have limitations or require prior authorization for certain procedures.For example, a high deductible plan might cover a significant portion of the cost of a colonoscopy only after the deductible is met, while a lower deductible plan may cover a greater percentage of the cost from the outset.
Similarly, the treatment of Crohn’s disease or ulcerative colitis may involve various medications, some of which may be covered under the formulary of your plan, while others may require pre-authorization or may not be covered at all. Always check your plan’s formulary and benefit descriptions for specific details.
Examples of Covered and Uncovered Services
Understanding the differences in coverage is essential for effective financial planning. Here are a few examples illustrating the variation in coverage for gastroenterology services across different UnitedHealthcare plans.
Covered Services (Often, but not always, depending on the plan):
- Colonoscopies (as preventative screenings or for diagnostic purposes)
- Endoscopies (upper and lower)
- Biopsies
- Certain medications for conditions like Crohn’s disease or ulcerative colitis (subject to formulary)
Services That May Not Be Covered (Or may require prior authorization):
- Certain advanced imaging tests (such as advanced MRI scans or specific types of endoscopy)
- Experimental or investigational treatments
- Medications not included in the plan’s formulary
- Services received from out-of-network providers (unless specifically allowed under your plan)
It is crucial to remember that this is not an exhaustive list and the specific coverage for each service will depend on your individual UnitedHealthcare plan. Always confirm coverage with your provider and your UnitedHealthcare plan administrator before receiving any service.
Patient Resources and Support
Navigating a healthcare plan, especially one as complex as a UnitedHealthcare gastroenterology plan, can be challenging. Fortunately, UnitedHealthcare offers a variety of resources designed to support patients and make the process easier. Understanding these resources can significantly improve your experience and ensure you receive the care you need.Understanding your plan benefits and accessing available support is crucial for effective healthcare management.
This section Artikels the resources available to help you manage your gastroenterology care with UnitedHealthcare. From finding in-network providers to understanding your financial responsibilities, the information below should provide you with the tools you need.
Customer Service Contact Information
UnitedHealthcare provides multiple avenues for contacting customer service. Their website usually features a prominent “Contact Us” section with various options, including phone numbers, email addresses, and online chat support. You can typically find separate contact information for general inquiries and for specific plan-related questions. For example, there might be a dedicated number for prior authorization issues or a specific email address for billing inquiries.
Always refer to your member ID card or the plan documents for the most accurate and up-to-date contact information.
Available Tools and Educational Materials
UnitedHealthcare often provides online tools and educational resources to help members understand their benefits and manage their health. These resources might include online portals where you can view your claims, check your benefits, and find in-network providers. Many plans also offer educational materials, such as brochures, videos, or articles, that explain common gastroenterological conditions, treatment options, and how to manage your health effectively.
These materials can be accessed through the UnitedHealthcare website or mobile app. Some plans might also offer access to telehealth services, allowing you to connect with a healthcare provider remotely for certain consultations or follow-up appointments.
Navigating the UnitedHealth prior authorization process for gastroenterology can be a headache, especially when you consider the broader healthcare landscape. The challenges are magnified when you think about access to care, like the issues faced by rural hospitals, as highlighted in this insightful article on Rural Hospitals Labor Delivery & – it makes you realize how systemic these problems are.
Ultimately, streamlining the UnitedHealth prior authorization process is crucial for ensuring timely and appropriate care for everyone.
Finding In-Network Gastroenterologists
Locating an in-network gastroenterologist is essential for maximizing your benefits and minimizing out-of-pocket costs. UnitedHealthcare’s website usually has a provider search tool, allowing you to search for specialists based on location, specialty, and other criteria. This tool typically provides details about each provider’s qualifications, location, contact information, and whether they accept your specific plan. It’s advisable to always verify a provider’s in-network status before scheduling an appointment to avoid unexpected billing issues.
Financial Assistance Programs
UnitedHealthcare may offer financial assistance programs to help members manage the cost of their healthcare. These programs can vary depending on your specific plan and your financial circumstances. It’s important to explore these options if you are facing financial challenges. Information about financial assistance programs is usually available on the UnitedHealthcare website or by contacting their customer service department.
These programs might include payment plans, discounts, or assistance with navigating the appeals process if a claim is denied.
Comparing UnitedHealthcare to Other Insurers: Unitedhealth Prior Authorization Gastroenterology Plan
Choosing a health insurance plan, especially when dealing with a specific condition like gastroenterological issues, requires careful consideration of various factors. Understanding the differences between major providers is crucial for making an informed decision that best suits your needs and budget. This comparison focuses on gastroenterology coverage, highlighting key differences in prior authorization processes, network sizes, and cost-sharing between UnitedHealthcare and two other prominent insurers: Aetna and Anthem.
Direct comparison of insurance plans is complex because coverage varies widely based on specific plan details (e.g., HMO, PPO, POS), location, and the individual’s chosen plan. The information below represents general trends and should not be considered exhaustive or a substitute for reviewing your specific policy documents. Always contact the insurance provider directly for the most accurate and up-to-date details.
Prior Authorization Procedures
Prior authorization requirements significantly impact access to care. UnitedHealthcare often requires pre-authorization for certain procedures and medications, varying by plan and the specific gastroenterologist. Aetna and Anthem also have prior authorization processes, but the specifics – such as the required documentation and turnaround times – may differ. For instance, while UnitedHealthcare might require detailed clinical notes for a colonoscopy, Aetna may focus more on the medical necessity justification.
Anthem’s requirements might fall somewhere in between, potentially emphasizing the use of their preferred provider network. The level of bureaucratic complexity and the time it takes to secure authorization can vary considerably between these insurers.
Network Sizes and Access to Specialists
Network size directly affects the choice of gastroenterologists. UnitedHealthcare boasts a large national network, but the availability of specialists within a specific geographic area can still be limited. Aetna and Anthem also maintain extensive networks, but their provider directories will vary. A potential patient needs to check the specific provider directory for their plan to ensure their preferred gastroenterologist is in-network.
A smaller network might lead to higher out-of-pocket costs if you see an out-of-network provider. The size and composition of the network are crucial factors to consider when comparing plans.
Cost-Sharing: Premiums, Deductibles, and Co-pays
Cost-sharing is a critical element. Premiums, deductibles, and co-pays differ significantly across insurers and even within the same insurer’s plan options. UnitedHealthcare offers various plans with different cost-sharing structures. Similarly, Aetna and Anthem provide a range of plans, each with its own premium, deductible, and co-pay levels. For example, a high-deductible plan with a low premium might be suitable for individuals who are generally healthy but want to lower their monthly payments, while a lower-deductible plan with a higher premium might be preferable for those anticipating more frequent healthcare needs.
Comparing these cost elements across the three insurers requires careful examination of individual plan details.
| Feature | UnitedHealthcare | Aetna | Anthem |
|---|---|---|---|
| Prior Authorization Process | Varies by plan and procedure; often requires detailed documentation. | Varies by plan and procedure; emphasis may vary on medical necessity. | Varies by plan and procedure; potential emphasis on in-network providers. |
| Network Size | Large national network; availability of specialists varies geographically. | Extensive network; geographic variations exist. | Extensive network; geographic variations exist. |
| Cost-Sharing | Wide range of plans with varying premiums, deductibles, and co-pays. | Wide range of plans with varying premiums, deductibles, and co-pays. | Wide range of plans with varying premiums, deductibles, and co-pays. |
End of Discussion
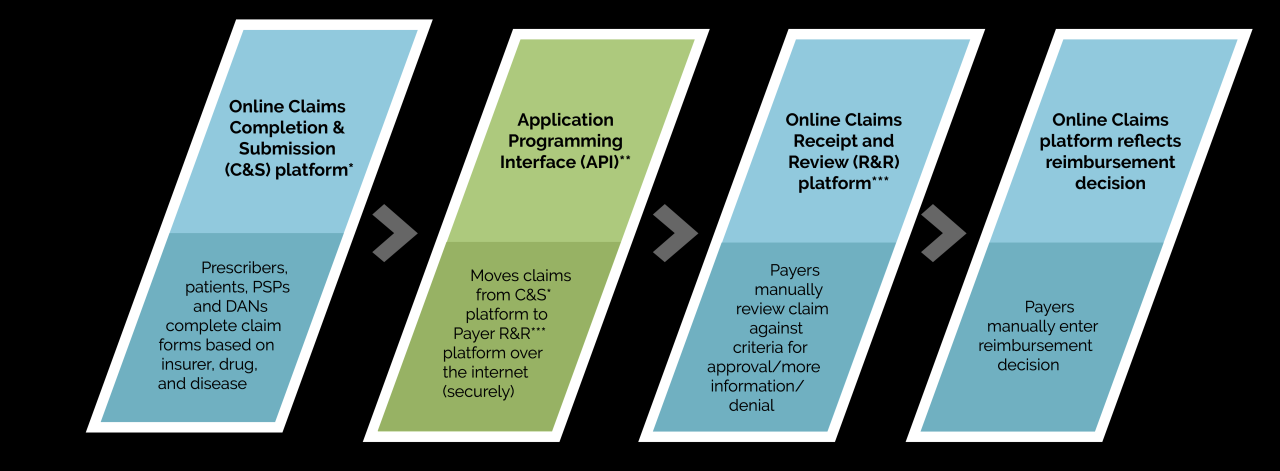
Source: myndshft.com
Successfully navigating the UnitedHealth prior authorization process for gastroenterology services requires preparation, understanding, and a bit of persistence. Remember, you’re not alone in this journey. By understanding your plan, gathering the necessary documentation, and knowing your rights, you can significantly increase your chances of a smooth and successful experience. Don’t hesitate to reach out to UnitedHealthcare directly if you need further assistance.
Your health is important, and advocating for it is key!
Question & Answer Hub
What happens if my prior authorization is denied?
Don’t panic! You have the right to appeal the decision. UnitedHealthcare Artikels a specific appeals process; carefully review their materials and follow the steps precisely. Make sure to include all necessary supporting documentation.
How long does the prior authorization process typically take?
Processing times vary, but it’s generally best to submit your request well in advance of your scheduled procedure. Allow at least a few weeks, and check in with UnitedHealthcare for updates if you haven’t heard back within a reasonable timeframe.
Can I get a pre-authorization for a second opinion?
Yes, often you can. It’s always best to check with your UnitedHealthcare plan to confirm their policy on pre-authorizations for second opinions, as requirements may vary.
What if I don’t have a PCP (Primary Care Physician)?
While having a PCP is often recommended, it’s not always mandatory for obtaining prior authorization for certain procedures. However, contacting UnitedHealthcare directly to clarify their specific requirements in your situation is advisable.